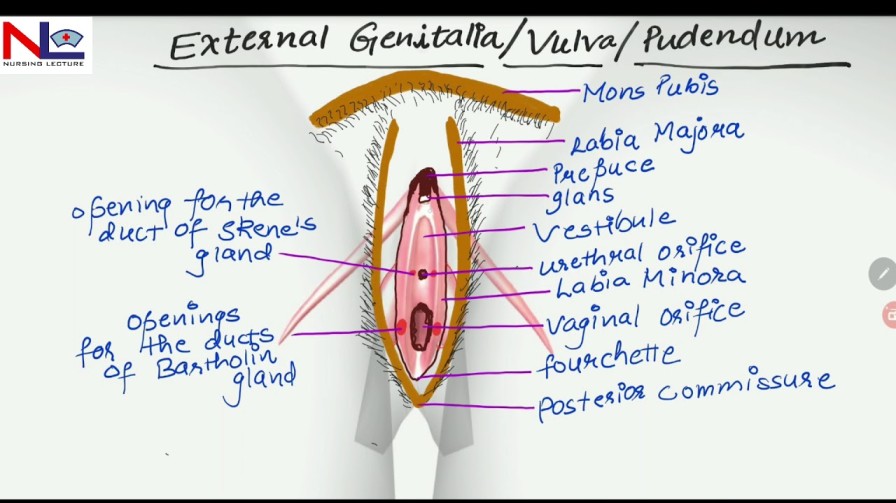
FEMALE EXTERNAL GENITAL
ORGANS
Female external genitalia (the vulva) include the mons pubis, labia majora, labia minora, clitoris, vestibule, the greater vestibular glands (Bartholin’s glands) and bulbs of the vestibule
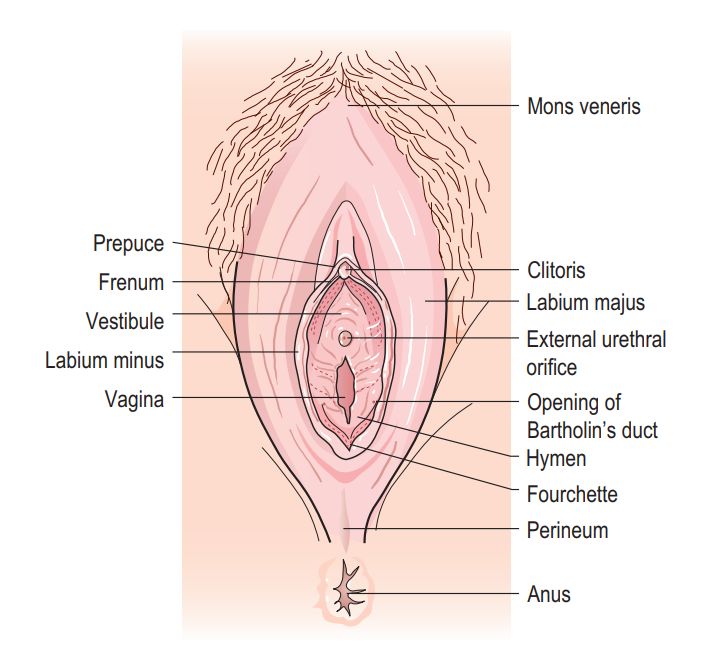
• The mons pubis is a rounded pad of fat lying anterior to the symphysis pubis. It is covered with pubic hair from the time of puberty.
• The labia majora (‘greater lips’) are two folds of fat and areolar tissue which are covered with skin and pubic hair on the outer surface and have a pink, smooth inner surface.
• The labia minora (‘lesser lips’) are two small subcutaneous folds, devoid of fat, that lie between the labia majora. Anteriorly, each labium minus divides into two parts: the upper layer passes above the clitoris to form along with its fellow a fold, the prepuce, which overhangs the clitoris. The prepuce is a retractable piece of skin which surrounds and protects the clitoris. The lower layer passes below the clitoris to form with its fellow the frenulum of the clitoris.
• The clitoris is a small rudimentary sexual organ corresponding to the male penis. The visible knob-like portion is located near the anterior junction of the labia minora, above the opening of the urethra and vagina. Unlike the penis, the clitoris does not contain the distal portion of the urethra and functions solely to induce the orgasm during sexual intercourse.
• The vestibule is the area enclosed by the labia minora in which the openings of the urethra and the vagina are situated.
• The urethral orifice lies 2.5 cm posterior to the clitoris and immediately in front of the vaginal orifice. On either side lie the openings of the Skene’s ducts, two small blind-ended tubules 0.5 cm long running within the urethral wall.
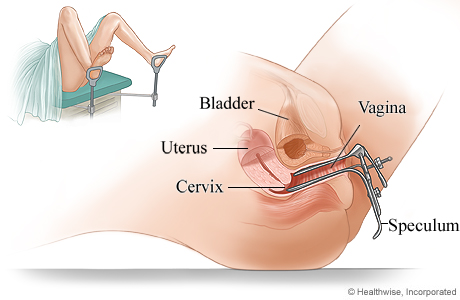
• The vaginal orifice, also known as the introitus of the vagina, occupies the posterior two-thirds of the vestibule. The orifice is partially closed by the hymen, a thin membrane that tears during sexual intercourse. The remaining tags of hymen are known as the ‘carunculae myrtiformes’ because they are thought to resemble myrtle berries.
• The greater vestibular glands (Bartholin’s glands) are two small glands that open on either side of the vaginal orifice and lie in the posterior part of the labia majora. They secrete mucus, which lubricates the vaginal opening. The duct may occasionally become blocked, which can cause the secretions from the gland to accommodate within it and form a cyst.
• The bulbs of the vestibule are two elongated erectile masses flanking the vaginal orifice.
Blood supply
The blood supply comes from the internal and the external pudendal arteries. The blood drains through corresponding veins.
Lymphatic drainage
Lymphatic drainage is mainly via the inguinal glands.
Innervation
The nerve supply is derived from branches of the pudendal nerve.
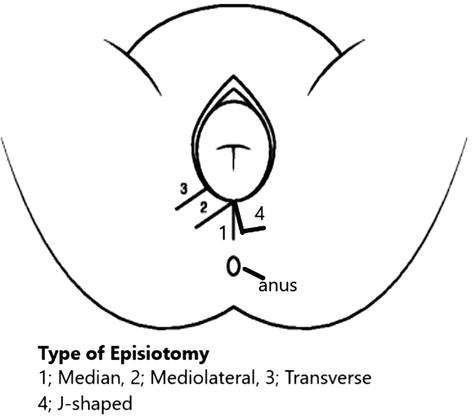
THE PERINEUM
The perineum corresponds to the pelvis outlet, forming a somewhat lozenge-shaped area. It is bordered anteriorly by the pubic arch, posteriorly by the coccyx, and laterally by the ischiopubic rami, ischial tuberosities, and sacrotuberous ligaments.
A transverse line drawn between the ischial tuberosities divides the perineum into two triangular portions. The anterior triangle, housing the external urogenital organs, is referred to as the urogenital triangle, while the posterior triangle, encompassing the termination of the anal canal, is known as the anal triangle.
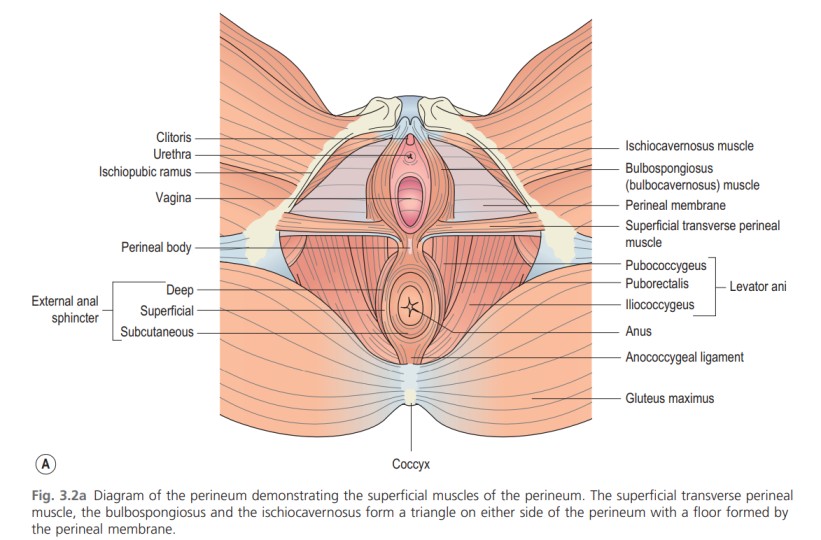
The Urogenital Triangle: The urogenital triangle is bounded anteriorly and laterally by the pubic symphysis and the ischiopubic rami. It comprises two compartments: the superficial and deep perineal spaces, separated by the perineal membrane that spans between the ischiopubic rami. The levator ani muscles attach to the cranial surface of this membrane. The vestibular bulb and clitoral crus are fused with the caudal surface of the membrane, covered by the bulbospongiosus and ischiocavernosus muscles.
Superficial Muscles of the Perineum: Superficial Transverse Perineal Muscle: Arising from the inner and forepart of the ischial tuberosity, the superficial transverse muscle is a narrow slip of muscle inserted into the central tendinous part of the perineal body. It connects with the external anal sphincter (EAS) from behind and the bulbospongiosus in the front, all attaching to the central tendon of the perineal body.
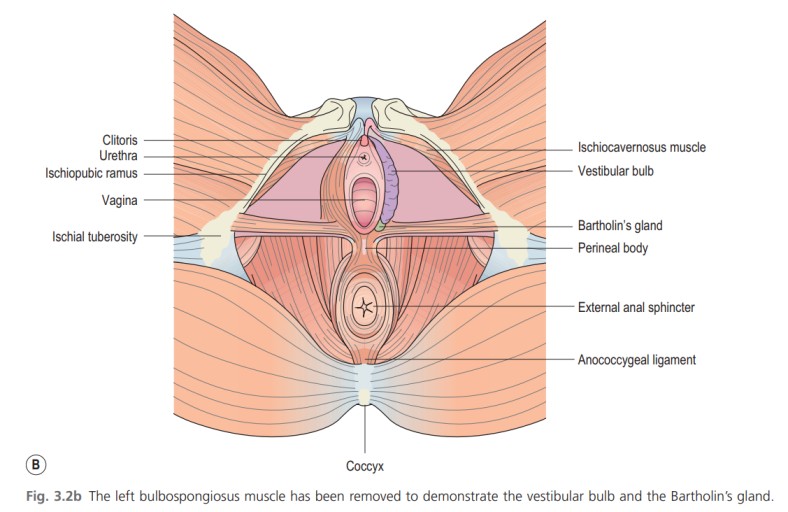
Bulbospongiosus Muscle: Running along each side of the vaginal orifice, the bulbospongiosus muscle covers the lateral aspects of the vestibular bulb anteriorly and Bartholin’s gland posteriorly. Some fibers merge with the superficial transverse perineal muscle and the EAS in the central fibromuscular perineal body. Anteriorly, its fibers extend around the vagina and insert into the corpora cavernosa clitoridis, compressing the deep dorsal vein. This muscle contributes to clitoral erection and narrows the vaginal orifice.
Ischiocavernosus Muscle: Situated on the lateral boundary of the perineum, the ischiocavernosus muscle is elongated, broader at its middle, and arises from the inner surface of the ischial tuberosity, crus clitoridis, and adjacent portions of the ischial ramus.
Innervation: Nerve supply is provided by branches of the pudendal nerve.
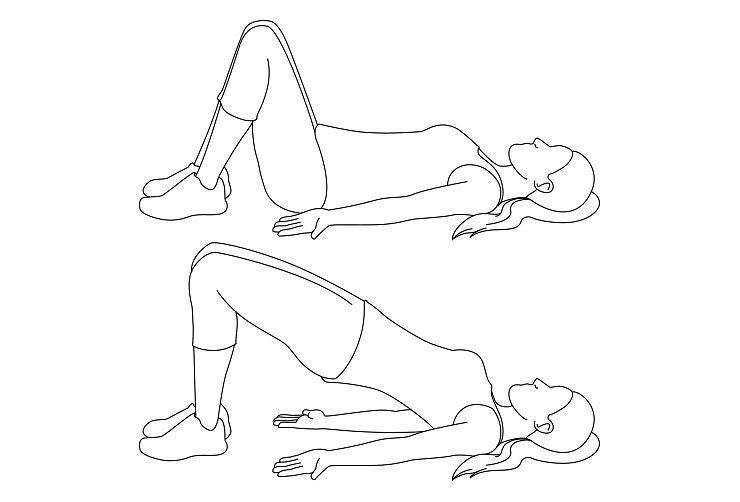
PELVIC FLOOR MUSCLES
Pelvic floor is a muscular partition which separates the pelvic cavity from the anatomical perineum.
It consists of three sets of muscles on either side—pubococcygeus, iliococcygeus and ischiococcygeus and these are collectively called levator ani.
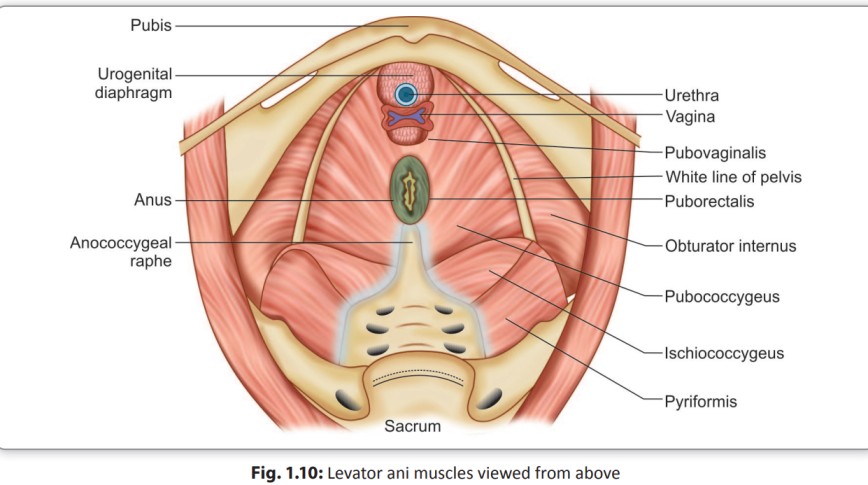
Its upper surface is concave and slopes downwards, backwards and medially and is covered by parietal layer of pelvic fascia. The inferior surface is convex and is covered by anal fascia. The muscle with the covering fascia is called the pelvic diaphragm/pelvic floor.
ORIGIN: Each levator ani arises from the back of the pubic rami, from the condensed fascia covering the obturator internus (white line) and from the inner surface of the ischial spine.
INSERTION: From this extensive origin, the fibers pass, backwards and medially to be inserted in the midline from before backwards to the vagina (lateral and posterior walls), perineal body and anococcygeal raphe, lateral borders of the coccyx and lower part of the sacrum (Fig. 1.10)
The muscles of the levator ani exhibit distinctive characteristics compared to most other skeletal muscles. These include:
- Sustaining continuous tone, except during activities like voiding, defecation, and the Valsalva maneuver.
- Demonstrating the capability to contract rapidly during moments of acute stress, such as coughing or sneezing, to uphold continence.
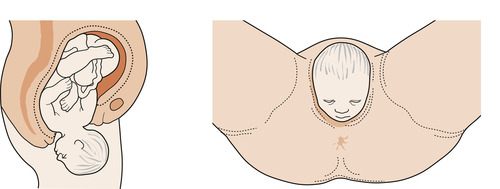
- Significantly expanding during childbirth to accommodate the passage of a full-term infant, followed by contracting after delivery to return to regular function.
THE PUDENDAL NERVE
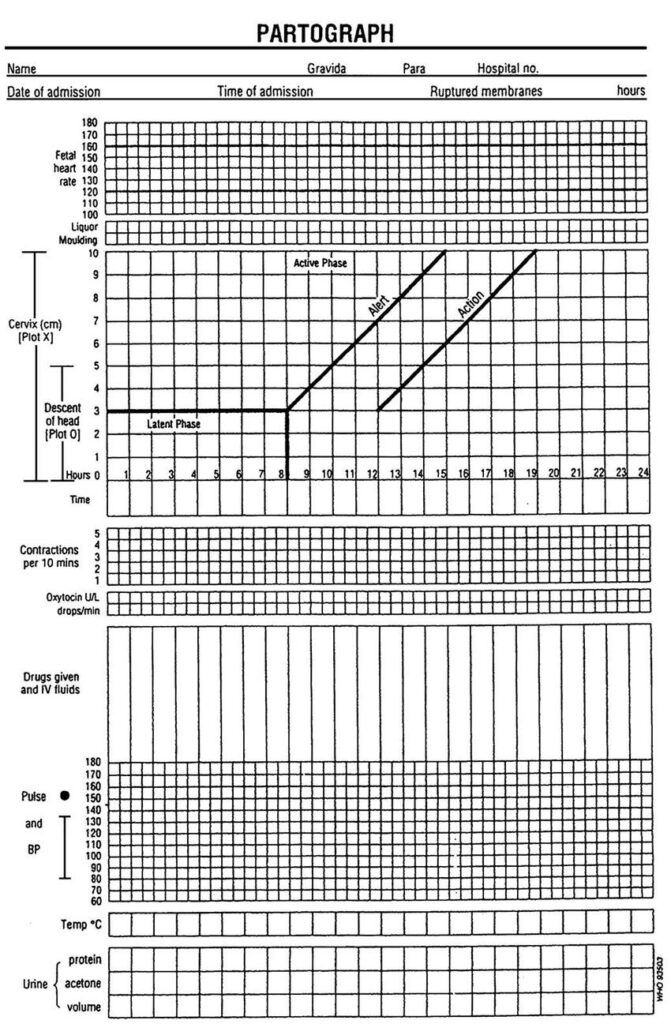
The pudendal nerve serves as a mixed motor and sensory nerve, drawing fibers from the ventral branches of the second, third, and fourth sacral nerves. Exiting the pelvis through the lower portion of the greater sciatic foramen, it traverses the ischial spine and reenters the pelvis via the lesser sciatic foramen. Progressing alongside the internal pudendal vessels, it courses upward and forward along the lateral wall of the ischioanal fossa within a protective sheath of the obturator fascia termed Alcock’s canal (Fig. 3.7). Notably, during an extended second stage of labor, the pudendal nerve is susceptible to stretch injury at this site due to its limited mobility.
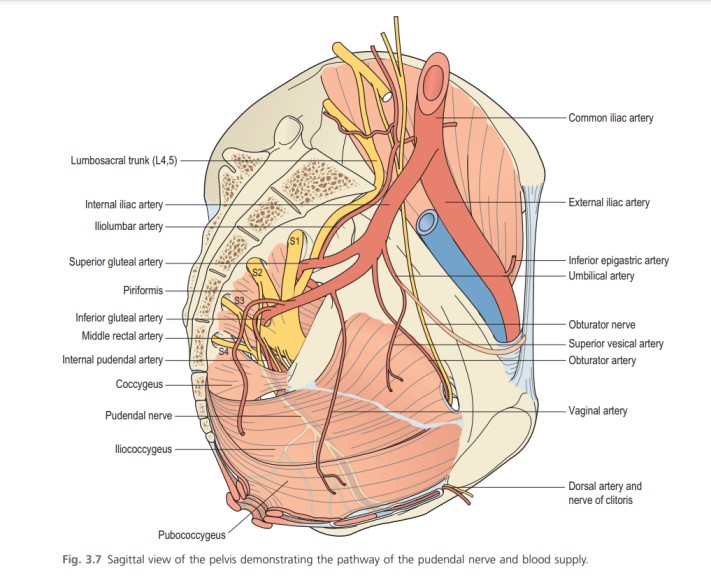
From the pudendal nerve’s posterior extension, the inferior haemorrhoidal (rectal) nerve diverges to innervate the external anal sphincter (EAS). Further division yields two terminal branches: the perineal nerve and the dorsal nerve of the clitoris. The perineal nerve subsequently splits into posterior labial and muscular branches. The posterior labial branches supply the labia majora, while the muscular branches distribute to the superficial transverse perineal, bulbospongiosus, ischiocavernosus, and constrictor urethrae muscles. The dorsal nerve of the clitoris, the nerve deepest within the pudendal division, innervates the clitoris itself.
FEMALE EXTERNAL GENITAL ORGANS Read More »