Safe Motherhood
Safe motherhood is defined as a series of initiative, practices and protocols and service delivery guideline designed to ensure that women receive high quality gynecological, family planning, prenatal, delivery and postpartum care in order to achieve optimal health for the mother, fetus and infants during pregnancy, childbirth and postpartum
Safe motherhood means that no woman and child should die or be harmed by pregnancy or birth. Safe motherhood begins with the assurance of basic safety living as a girl and a woman in society.
❖ Safe motherhood is founded on freedom to choose when and whether to have children and family planning for all couples.
❖ Safe motherhood encourages active participation during health care. It is founded on the freedom from discrimination of any form.
❖ Safe motherhood values the girl child.
❖ Safe motherhood implies the availability, acceptability and easy access to health care for a woman’s prenatal, birth, postpartum, family planning and gynecological needs.
❖ Safe motherhood requires involvement and commitment from each community and the nation to fairly allocate resources that promote the health of all women and infants.
❖ Safe motherhood means: social equity for women, maternal health care within PHC and access to emergency obstetrics and newborn care for management of complications when they arise.
Note: Safe motherhood is the concept that no woman or fetus or baby should die or be harmed by pregnancy or childbirth.
This is made possible by providing timely appropriate and comprehensive quality obstetric care during:
- ✔ Preconception
- ✔ Pregnancy
- ✔ Childbirth
- ✔ Puerperium
The Road Map to Safe Motherhood
This is the way the health of a woman is maintained throughout their child bearing age and during pregnancy, labor and puerperium so that the mother remains in good physical and mental conditions to avoid complications which may put her life at risk.
In order to achieve a safe motherhood, the health of the mother has to be monitored during pregnancy so that she remains in a good physical condition and delivers a normal healthy well breastfed baby without any abnormality.
During childhood, female children should have good nutrition so that they remain healthy as a good diet promotes good growth and adequate pelvis with fewer complications of future deliveries.
Children should be fully immunized against the killer diseases which may interfere with normal development and growth of the children.
Adequate and early hospitalization of children to avoid serious complications which may occur due to diseases
During adolescence, girls should be educated about safe sexuality and thus should be done before the sexual period experiment and, to risk early and unplanned pregnancy with all its risks of sexually transmitted diseases.
Information and education to young girls about maternal and child health and family planning so that mothers may avoid many children will make her work hard without having adequate rest.
Community and family support. A woman needs to be valued and protected both in an emotional and physical way. She should not be allowed to work too much hard especially when she is pregnant in order to avoid complications which may put her life in danger.
Mothers during pregnancy should be encouraged to attend antenatal clinics early and regularly so that the pregnancy and her condition is monitored , disorder detected and investigated, mother is given adequate treatment and the more serious ones sent for advanced management.
Education of traditional birth attendants (TBAs) and healers about safe motherhood, management of mothers during pregnancy, labour and puerperium; and to identify at risk cases in time and to refer them to hospital.
Community should participate in organizing referral system in case of emergency Adequate management of delivery to avoid complications to the mother and baby
Proper management during puerperium to detect early any complications so that proper management is given in Post natal clinic.
The history of global safe motherhood programs began in 1987, the global strategy for safe motherhood was launched in Nairobi, Kenya in 1987 at the international conference on safe motherhood. This conference was co-sponsored by the WHO in partnership with the World Bank, the United nation Funds for Development Activity (UNFPA) and United Nation
Development Program (UNDP).
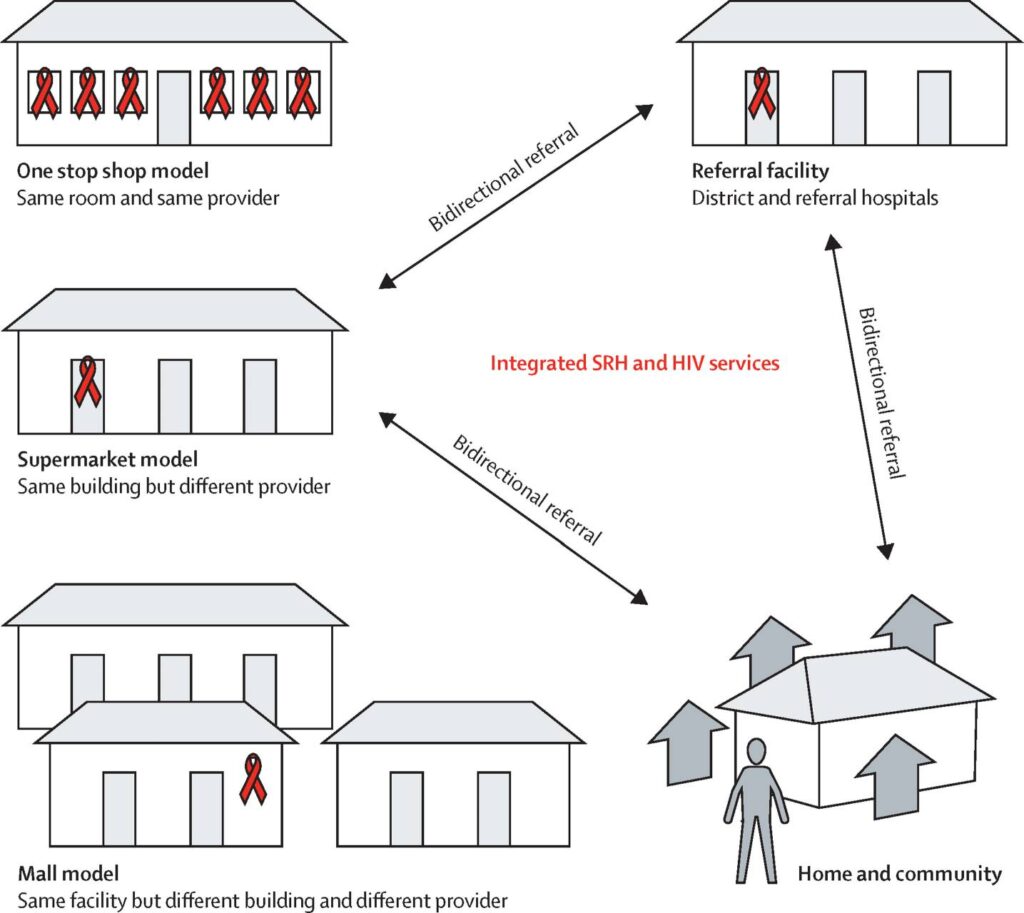
During the program of Action of the international conference on population and Development (ICPD) in 1994, a consensus was reached that meeting the reproductive health needs of women and men is a critical requirement for human and social development. The conference affirmed that reproductive health care is an integral component of primary health care and should be provided in that context. The elements (components) of reproductive health have a profound impact on the course and outcome of pregnancy and health service requirements for addressing them are closely related.
It was during this conference that consensus was built to adopt a strategy that addresses all aspects of reproductive health and provides an opportunity to develop an integrated approach to safe delivery and hence the WHO Mother Baby Package.
After about 5 years of introduction of the Mother Baby Package, WHO and partners introduced the need to improve maternal health and reduce maternal mortality through the making pregnancy safer strategy highlighted below:-
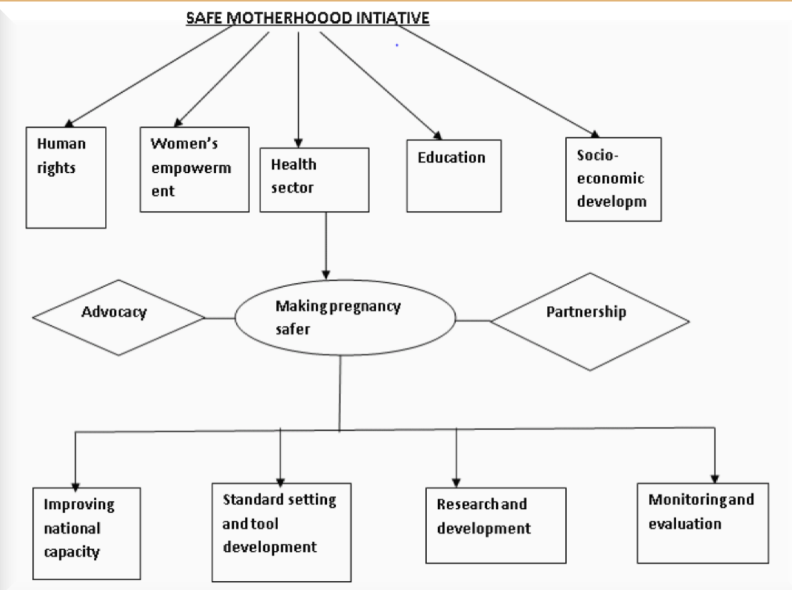
The making pregnancy safer strategy emphasizes the importance of the health sector interventions highlighted:
- – Advocacy
- – Partnerships
- – Improving national capacity
- – Standard setting and tool development
- – Research and development
- – Monitoring and evaluation
If these are well implemented they have the capacity to significantly reduce maternal mortality in countries.
What is known worldwide about adverse maternal health is that a country’s overall economic wealth is not the only important determinant.
According to national and internal human right treaties, safe motherhood is considered a human right issue. Therefore it is considered that maternal death is the reflection of ―social disadvantage not merely a― health disadvantage.
Aims of Safe Motherhood
- To ensure that all deliveries are conducted hygienically and according to accepted medical practices, thereby preventing complications that are caused or exacerbated by poor care.
- Identify complications promptly and manage them appropriately either by treating or referring them to a higher level of care.
- Provision of high quality, culturally appropriate care, ensuring necessary follow up and linkages with other services including antenatal and post-partum care as well as family planning, post abortion care and treatment of STIs.
- To enhance the quality and safety of girls‘ and women‘ lives through adaptation of a combination of health and non-health related strategies.
Note: Maternal and child health promotion is one of the key commitments in the WHO constitutions.
Safe motherhood initiative is a global effort and it is designed to operate through its partner i.e.
- – Government agencies
- – NGOs
- – Other groups and individuals
It aims to improve women‘s health through social, community and economic interventions.
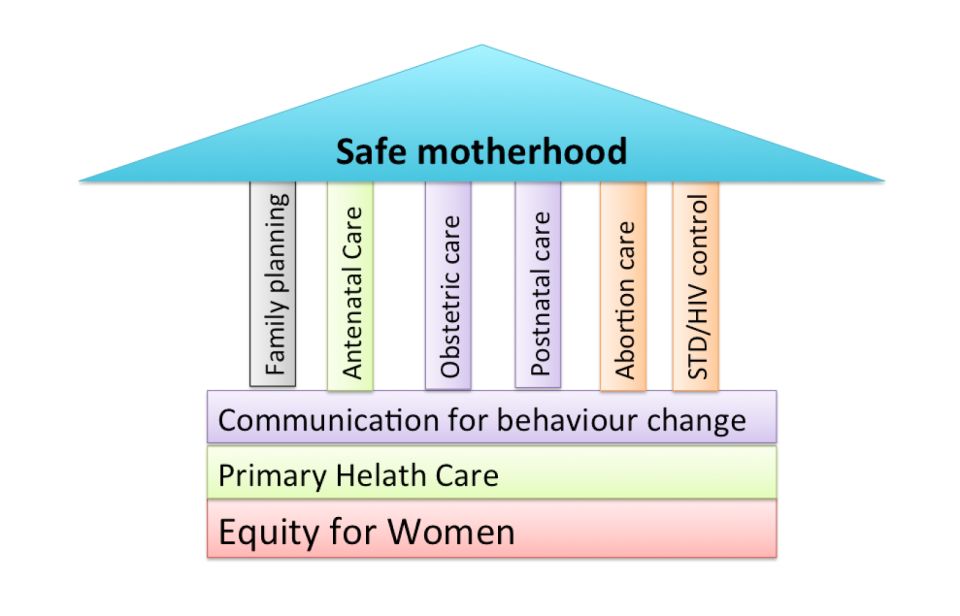
Pillars of Safe Motherhood
- Family planning; to ensure that individuals and couples have the information and services to plan the timing, number and spacing of pregnancies and thus the number of unsafe abortion.
- Antenatal care; to prevent complications where possible and ensure that complications of pregnancy are treated appropriately and very serious conditions referred within the shortest possible time.
- Clean/safe delivery and postnatal care; to ensure that all birth attendants have the knowledge, skills and equipment to perform a clean and safe delivery and provide postpartum care to the mother and baby, all women should have access to basic maternity care during delivery.
- Emergency obstetric care; to ensure that essential care for high risk pregnancies and complications is made available to all women and girls who need it. It is estimated that about 15 % of all normal pregnancies end up with complications therefore the need to always be prepared for emergency obstetric care.
- Basic maternity care
- Primary health care
- Equity for women
Components of safe motherhood
- Per-conception care
- Antenatal care
- Postpartum care
- Post abortion care
- Emergency obstetric care
- Care of the newborn
Requirements for safe motherhood
Achieving safe motherhood and reducing maternal mortality requires a 3 way strong strategy:
- All women have access to contraception to avoid unintended pregnancies.
- All pregnant women have access to skilled attendance at the time of birth.
- All women with complications have timely access to quality emergency obstetric care.
The roles of community in safe motherhood
The community can give support in several ways to make motherhood safer:
- Share the workload so that mother can avoid heavy physical work
- Encourage pregnant mother to eat a balanced diet and rest than usual especially during the last three months
- Encourage mothers to take their non-pills or other medication as provided
- Help with looking after children so that mother can go for antenatal care and delivery in the hospital
- Establish transport readiness for emergency referral and obstetrical complications
- Encourage risk mothers to use maternity waiting areas, if advised to do so during antenatal care
- Creates inform and motivated community based safe motherhood groups