Table of Contents
ToggleFirst Aid Medical Emergencies.
First aid is a crucial skill that everyone should possess, as it enables individuals to provide immediate care and assistance to someone who has been injured or is experiencing a medical emergency.
There are various medical emergencies that require prompt first aid intervention. Some of the most common ones include:
DROWNING
Drowning is defined as the process of experiencing respiratory impairment due to being submerged or immersed in water.
It occurs when the airway is blocked, preventing the person from breathing properly and leading to oxygen deprivation.
Drowning can result into death from hypothermia due to immersion in cold water, sudden cardiac arrest due to spasm of the throat blocking the air way or inhalation of water and consequent air way obstruction.
CAUSES OF DROWNING
Lack of swimming ability: Inability to swim or lack of proper swimming skills increases the risk of drowning, especially in situations where individuals find themselves unexpectedly in water.
Absence of barriers: Insufficient barriers, such as pool fences or lifeguards, can lead to unsupervised access to water bodies, putting individuals, especially children, at higher risk of drowning.
Alcohol consumption: Alcohol impairs judgment, coordination, and reaction time, increasing the likelihood of accidents and drowning incidents in water-related activities.
Seizures or medical conditions: Individuals with conditions like epilepsy or seizure disorders face a higher risk of drowning if an episode occurs while they are near water.
Lack of supervision: Insufficient adult supervision, particularly for children and inexperienced swimmers, can lead to tragic outcomes when accidents happen in or near water.
- Fatigue: Especially when a person has been swimming for too long and gets too tired to continue.
Question: What happens during drowning? The drowning victim struggles of inhale air as much as possible but eventually he goes beneath the water whereby he must exhale air and inhale water.
If this person is not rescued as early as possible, accidental death will result.
SIGNS AND SYMPTOMS
- Difficulty in breathing
- Noisy breathing
- Water comes out from the mouth and the nose.
- Distended abdomen
- Cyanosis
- Confusion
- Rapid pulse
- Unconsciousness
- Fits may occur
- Breathing may stop.
FIRST AID MANAGEMENT:
Aims of Management
- To restore adequate breathing.
- To keep the casualty warm.
- To arrange for urgent transport to hospital.
(a) REACHING A VICTIM
- Pull the victim from the water using a rope, a branch of a tree, a stick, a shirt etc.
- Lie down flat on your stomach and extend your hand or leg to the victim.
- Throw him an object that will float for example a tire, a log, plastic toes, cautions etc.
- Make sure that your own position is safe to rescue to the victim.
- You can also use a boat and a life jacket if available and swim or tow the casualty to shore or bank.
(b) WHEN THE CASUALTY HAS REACHED THE SHORE
- Help him lie down a coat, or a rug or any piece of cloth with his head lower than the rest of the body so that the water can drain easily from the mouth and nose. This reduces the risk of inhaling water.
- Treat the casualty for hypothermia, remove wet clothing and replace with dry ones if possible and cover him with dry blanket or any piece of cloth.
- If the casualty is fully conscious, give him a warm drink if available.
- If the casualty is unconscious, open the air way, check the breathing and if not breathing , initiate cardiopulmonary resuscitation. (CPR)
- Give five (5) initial rescue breaths before you start chest compressions.
- Call for emergency help even if the casualty appears to have recovered fully because of the risk of secondary drowning.
- Any water entering lungs causes them to become irritated and the air passages may begin to swell several hours later this condition is known as secondary drowning.
- Monitor and record vital signs such as level of response, breath and pulse until help arrives.
PREVENTING DROWNING
Learn to swim: Acquiring swimming skills and encouraging others, especially children, to learn how to swim significantly reduces the risk of drowning.
Constant supervision: Ensure active and serious supervision when individuals, especially children, are in or near water. Avoid distractions like phones or other activities that may take away attention.
Use appropriate barriers: Install and maintain proper barriers like pool fences, covers, or gates to restrict access to water bodies and prevent unsupervised entry. Pool nets to cover pools are helpful too when having children around.
Wear life jackets: In situations where swimming ability is limited or uncertain, wearing properly fitted life jackets can be essential and increase safety.
BURNS AND SCALDS:
BURNS: Are tissue injuries caused by dry heat, extreme cold corrosive substances, friction or radiation. Or: Is the destruction of the body surface by dry heat.
SCALDS: Are tissue injuries caused by wet heat from hot liquids and vapor.
TYPES OF BURNS:
(a) DRY BURNS: Dry burns occur when the skin comes into direct contact with a dry heat source. Examples of dry heat sources include flames, hot objects, or heated surfaces such as stoves, flat iron.
COMMON CAUSES
- Contact with hot object
- Friction
- Flames
(b) ELECTRICAL BURNS: Electrical burns occur when the body comes into contact with an electrical current. These burns can result from accidents involving faulty electrical appliances, exposed wiring, lightning strikes, or high-voltage power lines.
COMMON CAUSES
- High voltage current
- Lightening
(c) CHEMICAL BURNS: Chemical burns occur when the skin or eyes come into contact with corrosive or harmful chemicals. Chemical burns can result from contact with acids, alkalis, solvents, cleaning agents, or industrial chemicals.
COMMON CAUSES
- Industrial chemicals including inhaled fumes and corrosive gases, domestic chemicals and agents. For example paint, pesticides, bleaching agents or any other strong acid or alkaline chemical.
(d) RADIATION BURNS: These are caused by over exposure to ultraviolet rays from the sun, exposure to radioactive sources such as x – rays.
(e) COLD INJURY: Cold burns, also known as frostbite, occur when the skin and underlying tissues are exposed to extreme cold temperatures. Cold burns can result from direct contact with extremely cold objects, exposure to freezing temperatures, or prolonged exposure to cold, contact with freezing vapor such as oxygen or nitrogen. Frostbite can cause the affected areas to become numb, pale, and firm to the touch.
PEOPLE AT RISK OF BURNS
-
- Children mostly under five years of age.
- Elderly.
- Those with medical related conditions like seizure due to epilepsy, diabetes, leprosy, and albinism.
- Alcoholic or drug abusers.
- Factory workers.
- Petrol station pump attendants/ workers.
CAUSES:
The causes of burns and scalds are external and can be grouped as follows.
- Dry heat can be from flame or any hot object.
- Moist heat can be from hot water or steam.
- Corrosive chemicals such as acid and alkaline
- Electricity.
- X –rays or ionizing radiation including radiation dermatitis.
- Friction.
- Smoke and inhalation of toxic substances.
SIGNS AND SYMPOMS
- Reddening of the skin
- Swelling
- Blister formation
- Pain due to exposure to the nerves common in 2nd degree burn
- Peeling off the skin.
- The victim is restless.
- Dehydration
- Signs may be present
- For air way burns, there is;
- Difficulty in breathing
- Hoarseness of the voice.
- Shivering due heat loss.
CLASSIFICATION OF BURNS:
Burns are classified according to depth and the extent of damage.
(a)BASED ON DEPTH
- Superficial burns.
- Partial thickness burns
- Full thickness burn.
1. SUPERFICIAL BURNS/ FIRST DEGREE BURNS
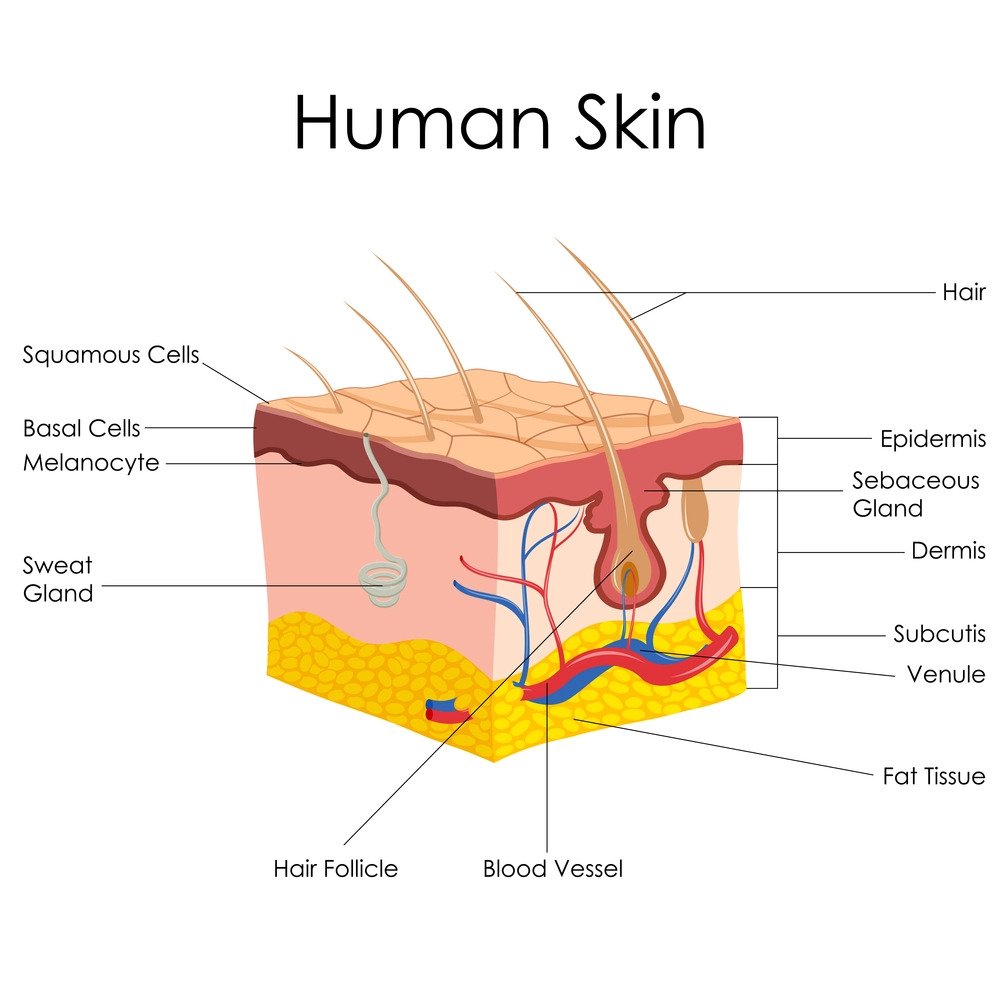
This involves only the outer most layer of the skin. It is characterized by pain, redness, swelling, and tenderness but do not result in blistering. It usually heals well if first aid is given promptly.
2. PARTIAL THICKNESS/ SECOND DEGREE BURNS
It involves the epidermis and dermis layers of the skin, the skin may peel off. In this case, medical treatment may be needed.
3. FULL THICKNESS BURNS/ THIRD DEGREE BURNS.
All the layers of the skin are burnt. There may be some damage to the nerves, the fatty tissues and muscles. Full thickness burns are characterized by loss of pain sensation. This may mislead both the first aider and the casualty about the true severity of the injury. Urgent medical attention is always essential for such burns (pain loss is a sign of nerve damage and not a sign of fairness).
( b)BASED ON DEGREE OF SEVERITY
(i) FIRST DEGREE: Epidermis is only involved reddening of the skin (erythema), no blisters formed.
(ii) SECOND DEGREE: Epidermis and some dermis are destroyed, blister formation, severe pain due to nerve exposure, mild to moderate edema.
(iii) THIRD DEGREE: Epidermis, dermis and hypodermis are involved some muscles get burnt it looks dry, waxy or hard skin and there is no pain.
(iv) FOURTH DEGREE: The whole skin is burnt including muscles, bones, tendons and ligaments.
EXTENT OF BURNS
It is vital to assess the extent of the area affected by the burn. This is because, the greater the surface area affected, the greater the fluid loss and the higher the risk for shock.
The extent of the burnt area is assessed using a simple formula known as WALLACE’S RULE OF NINE TO ADULTS.
The rule of nine divides the body into areas of about 9% as follows
- Head and neck – 09%
- Frontal trunk – 18%
- Back trunk – 18%
- Each arm – 9*2= 18%
- Lower limbs – 18*2=36%
- Perineum – 1%
- Total – 100%
RULE OF SEVEN FOR CHILDREN:
- Head – 28%
- Front trunk – 14%
- Back trunk – 14%
- Each lower limb – 14*2=28%
- Each upper limb – 7*2=14%
- Perineum – 2%
- Total – 100%
This formula divides the body in areas about 7% and is used in estimation of burns in children.
NOTE: If 60% of the skin is burnt or 40% in the very young or very old, kidney failure is likely to occur up to 6 weeks post burning. 30 – 40% burns and above, the patient is considered as having severe burns and should be hospitalized.
FIRST AID MANAGEMENT
(a) FOR MINOR BURNS
These include superficial burns and those covering a small area.
Aims
- To reduce pain
- To prevent complications
- To reassure the victim
- To arrange for urgent transport.
MANAGEMENT
- Put out the fire by pouring water or rapping the victim in a blanket. Do not allow the person on fire to run about especially into fresh air
- Cool the burnt area immediately by immersing it in cold water or putting it under gentle cold water for at least 10 minutes. Do not apply ice onto the skin.
- A clean cold towel can also be applied to help in reducing the pain (cold compress).
- If blister form, leave them untempered with i.e. do not break them.
- Dry the area with clean piece of cloth and cover with a dry sterile non adhesive dressing to help prevent contamination on and infection.
- The first aider should pack the area while drying.
- Protect the burn area from pressure and friction.
- Reassure the casualty to reduce on the anxiety.
- Seek medical help if the burn involves the airways, eyes, hands or genitals.
- Seek medical advice if the patient develops signs of infection.
- Obtain an up to date information from the patient about tetanus immunization i.e. is this casualty fully immunized against tetanus.
FIRST AID MANAGEMENT FOR SUPERFICIAL BUT EXTENSIVE BURNS:
Burns that are not deep but cover a bigger %age of the body require a prompt medical attention.
- Call for help
- Put out fire by pouring in water or rapping a blanket.
- Remove clothing’s from the burnt area if they come off easily, otherwise do not disrupt the burn if the clothing’s are stuck to the skin.
- Reassure the victim to relieve anxiety.
- Remove any ring or constricting items since the burnt area may swell any time making it difficult to remove them.
- If the burnt area is smaller than the victim’s chest, cool the burn by lowering it with a clean cold wet towel or gently running cold water.
- If the burn is larger than the victims chest do not immerse the burn in cold water because there is risk of overcooling the victim instead cover the burn with a dry sterile non adhesive dressing to prevent contamination.
- If fingers or toes are burnt, separate them with a dry sterile non adhesive dressing.
- If there is shock, carry out measures to treat it or other ways to prevent it.
- Treat shock.
- Transfer to hospital as early as possible and keep the head in one position during transit.
- Stay with victim until he gets medical help.
- Keep dressing clean, dry and change them whenever necessary.
- Obtain information about tetanus immunization.
COMPLICATIONS OF BURNS
Immediate
- Vascular, tendon& nerve injury
- Foreign body inclusion
- Skin loss& necrosis
- Airway obstruction of respiratory distress
Intermediate
- Secondary infection
- Shock due to pain
- Dehydration
- Reduced circulatory volume
- Electrolyte imbalance
Late
- Infections
- Contractures
- Renal failure
- Unstable scars
- Alopecia
- Marjolin’s ulcer(squamous cell carcinoma developing from the old scar)
ELETRIC BURNS:
Electric injuries are due to effect of high electric current voltage. The heat generated during the passage of current then through the body causes the deep burns.
In case of direct shock at the source, the victim remains stuck to the source of electricity until current is less. There may be:
- Physical injury when the victim falls down
- Respiratory arrest.
- Cardiac arrest.
Sources of electric current.
High current from cables from the main sources or low current from appliances.
- Electrical appliances such as coffee grinders, iron boxes, shaving machines, washing machines, television sets, work shop and shops’ appliances, offices installations, etc. These are usually connected to a direct power source either of low voltage or high voltage.
Note: Dump clothing’s, foot wear and ground increases electrical conductivity and makes the damage worse.
DANGERS OF ELECTRIC BURNS:
- Cardiac arrest due to passage of current through the heart
- Severe burns
- Shock
- Unconscious
MANAGEMENT
- Switch off the current and remove the plug from the socket to break contact of the casualty with the electric source.
- If the patient is lying in water keep out of it yourself as water is an excellent conductor of electricity.
- If the patient is in contact with a live wire and the current cannot be switched off, separate the wire from the victim using a long wooden stick and while standing on a non – conductor of electricity such as a wooden board or a pile of news papers. Wear gloves if available.
- Give artificial respiration and external cardiac massage if necessary.
- Flood the injury with cold water at least 10 minutes or until the pain is relieved. If water is not available, any cold harmless liquid can be used.
- Gently remove any jewelry, watches, belts or constricting clothes from the injured area before it begins to swell.
- Cover the burnt area using a sterile non – adhesive dressing and bandaging loosely.
- Treat shock if present.
- Give fluids to drink if conscious.
- Reassure the casualty.
- Monitor and record vital signs e.g. level of response, breathing and pulse.
- Arrange and send the casualty to hospital.
DON’TS
- Do not touch the casualty if he is in contact with electric current.
- Do not use any thing that is wet to break the electrical contact with victim.
- Do not approach high voltage wires until the power is turned off.
- Do not move a person with electrical injury unless he is immediate danger and is no longer in contact with one.
PREVENTION OF ELECTRICAL INJURIES IN THE HOMES OR AT WORK PLACE
- Wiring in the house must be checked by a competent electrician at intervals and rewiring is necessary
- Adequate number of power points is essential instead of having only one plug where many appliances are run risking power over load is very dangerous.
- Plugs should also be wired correctly
- Follow manufacturer’s instructions when using electrical appliances.
- Switches and electrical appliances must not be touched with wet hands or wall heaters and lights should be having cord pulls.
- Electrical appliances should be kept out of bath rooms
- Shavers should be used with properly insulated sockets.
- Children should not be allowed to have access in areas where these appliances are connected or used and should be taught dangers of electric shock.
CHEMICAL BURNS:
Certain chemicals may irritate, harm or be abserbed through the skin, causing wide spread and sometimes fetal damage. Signs however, develop slowly unlike in burns.
SIGNS AND SYMPTOMS
- – Evidence of chemical in the vicinity.
- – Intense, stinging pain.
- – Later, discoloration, and blistering, peeling and swelling of the affected area.
TREATMENT
Aims
- To disperse the harmful chemical.
- To arrange transport to hospital.
- To make the area safe and inform the relevant authorities.
STEPS
- First make sure the area is safe by assessing for signs of hazardous substances around you and the casualty.
- Remove the casualty from the area if necessary.
- Flood the affected area with water to disperse the chemical and to stop the burning. Do this for as long as 20 minutes.
- Gently remove any contaminated clothing while flooding the injury.
- Take or send the casualty to hospital, watch for airway and breathing closely.
- Ask the casualty if she can identify the chemical, and take care not to contaminate yourself by putting on gloves.
- Never attempt to neutralize an acid or alkali burns unless you are trained to do so and do not delay starting treatment by searching for an antidote.
- Note and pass the details about the chemical to the medical personnel.
CHEMICAL BURN TO THE EYE
- Splashes of chemicals in the eye can cause serious injury if not treated quickly.
- Chemical can damage the surface of the eye, resulting in scarring and blindness.
- When irrigating the eye, be especially careful that the contaminated rinsing water does not splash you or the casualty.
- Wear gloves if available.
SIGNS AND SYMPTOMS
-
- Intense pain in the eye.
- Inability to open the injured eye.
- Redness and swelling around the eye
- Copious watering of the eye.
- Evidence of chemical substances or containers in the immediate area.
TREATMENT
AIMS
- To disperse the harmful chemical
- To arrange removal to the hospital.
STEPS OF ACTIONS
- Do not allow the casualty to touch the injured eye or forcifully remove contact lens.
- Hold the affected eye under gently running cold water for at least 10 minutes.
- Make sure that you irrigate both sides of the eye eyelid thoroughly. It is easier to pour water from a glass or eye irrigator or tap.
- If the eye is shut in a spasm of pain, gently but firmly pull the eye lids open. Be careful that the contaminated water does not splash to uninjured eye.
- Ask the casualty to hold a sterile eye pad of clean, non – fluffy material over the injured eye and put bandage over the eye pad.
- Take or send the casualty to the hospital.
- Identify the chemical if possible and give details.
SHOCK
Shock is a condition which occurs when the circulatory system fails. And as a result, vital organs like heart, brain are deprived from oxygen.
OR: Shock is a cute circulatory failure. The severities of shock vary with nature and extend of injury. It is a common cause of death incase of severe injury. Shock may develop suddenly or gradually. It can be made worse or pain.
Inadequate tissue perfusion can result in:
- Generalized cellular hypoxia (starvation)
- Wide spread impairment of cellular metabolism.
- Tissue damage – organ failure
- Death
Shock can be of two types i.e.
1. PRIMARY SHOCK: This is shock which occurs immediately after injury. It is due to excessive stimulation of nerve endings at the site of the injury, but recovers quickly if treated promptly.
2. SECONDARY SHOCK: This develops within the next 30 minutes or even an hour. This is usually caused by hemorrhage. Secondary shock is a serious condition and if not treated properly and promptly, it can cause death. Therefore, the first aider should every possible think to prevent shock development or reduce its effects.
TYPES OF SHOCK ACCORDING TO THE CAUSES:
- NERVOUS SHOCK (PSYCHOGENIC SHOCK): This type of shock is due to strong emotional upset. This could be caused by fear, pain; it could also be caused by good or bad news. It can also be due to spinal or head injury because this comes from the shock.
- HAEMORRHAGIC OR HYPOVOLEMIC SHOCK: This is due to loss of blood or loss of fluids. Bleeding could be external. It could be due to multiple injuries. It can also be due to severe vomiting or diarrhea.
- CARDIOGENIC SHOCK: This is when the cardiac muscles can not pump blood infectively either due to injury or if the person has a heart disease. This means the damaged muscles have no enough pressure to the rest of the body.
- BACTERIAL OR SEPTIC SHOCK: This refers to severe infection where there is discharge of poisons or toxin the blood stream. These bacteria or toxin tend to cause dilatation of blood vessels, and when the blood vessels are dilated they tend to withdraw blood.
- ANAPHYLATTIC SHOCK: This due to severe allergic reaction of the body to some drugs. They may also react to foreign items. In this case there is dilatation of blood vessels and again blood is withdrawn from some of the organs.
- ELECTRIC SHOCK: This is due to high voltage of an electric current. If any part of the body comes in contact with a live wire or an electric cable which has leaking current, then the person will get electric shock.
- NEUROGENIC SHOCK: Chemical injury – association with aspiration of gastrointestinal contents during general anesthesia especially in cesarean section. It is also due to dry induced – associated with spinal anesthesia.
POSSIBLE CAUSES OF SHOCK
- The most common cause of shock is severe blood loss. (Hemorrhage or bleeding)
- Other causes include severe burns and scalds.
- Fractures can also lead to shock possibly because of pain and some fractures are associated to bleeding.
- Severe pain.
- Excess fluid losses from the body – diarrhea, vomiting etc.
- Excessive fear can lead to shock.
- Some conditions like heart disease if severe.
- Severe infections.
- Low blood sugar in the body (Hypoglycemia).
- Severe allergic reactions. (Anaphylactic shock)
- Drug over dose.
- Exposure to heat and cold.
SIGNS AND SYMPTOMS OF SHOCK
- Giddiness and fainting
- Patient may have nausea and vomiting.
- Pulse is rapid and weak.
- Blood pressure is low.
- Patients may be restless.
- Breathing is shallow and rapid. (gasping)
- Temperature is sub – normal.
- The extremities are cold.
- The patient may become unconsciousness and eventually the heart may stop.
- Dizziness and weakness.
- Thirst.
GENERAL TREATMENT FOR SHOCK
It is important to treat primary shock promptly in order to avoid secondary shock.
AIMS OF TREATMENT
- Is to improve blood supply to the brain, heart, lungs refer the patient as soon as possible.
- Let the patient lie down with the head lower than the rest of the body. This helps to send blood to the vital organs.
- The head should be turned to one side.
- The casualty should be moved as little as possible and should not be handled unnecessarily.
- Keep the casualty warm but not over heated.
- Stop any bleeding if there.
- Immobilize any fracture if present
- Treat any injuries.
- Loosen any tight clothing around the neck, waist.
- Check the breathing, the pulse and level of responsiveness every 10 minutes.
- If breathing becomes difficult or this patient like vomit put him/her in recovery position.
- If the casualty becomes unconscious, ensure an open airway, check breathing.
- Take/ arrange for transfer of casualty to hospital maintaining the treatment position.
- Re-assure the casualty if conscious or the relatives.
- If the patient is not in severe shock and is conscious, give fluids to drink.
- If the cause of the shock is not established, just give sips of clear water.
- If oral fluids are contra – indicated, patient is put on intravenous fluids, I.V fluids should be given with care to avoid over loading the heart. When a patient is on intravenous, watch the pulse rate carefully.
- Relief of pain in case of a fracture, it should temporarily be splinted.
- In case of burns, cover with smooth and clean cloth.
- Give analgesics (pain killer) e.g. morphine. Morphine should not be given if the patient has a respiratory problem, because it depresses the respiratory center which is found in the brain.
- You continuously re-assure the casualty and attendants or relatives.
ASPHYXIA
Asphyxia is a fatal condition which occurs if there insufficient oxygen to the tissues of the body.
The deficiency may be due to insufficient amounts of oxygen in the breathed in. It may also due to interference or injury to the respiration system. Without adequate supply of oxygen, the tissues deteriorate very rapidly. So the vital structures will lack enough oxygen leading to loss of conscious or even death.
CAUSES OF ASPHYXIA
Many conditions can lead to asphyxia. And these are conditions which affect the air way and the lungs i.e.
- Fluids in the air passages. For example, drowning
- Obstruction to the air way. This may be caused by; the tongue falling back in case of an unconscious casualty can also be caused by food, vomit, it could be foreign body.
- Swelling and edema of the tissue with in the throat. This may be due to severe burns of face and neck, it may be due to a sting (wasp or bee), and blood can also cause a blockage, swelling.
- Compression of the wind pipe. This may due to strangulation or compression of the chest.
- It may be due injury to lungs.
- Fits can also disturb the respiratory passage.
- Conditions which may affect the brain (respiratory centre) e.g. electrical injury (shock), poisoning, stroke by lightning , paralysis (which may be due to injury of spinal code)
- Inhalation of harmful gases or fumes in the air, passages, e.g. coal gas, motor exhaust fume, smoke sewage gas and ammonia affect the level of oxygen in blood.Note: some gases affect the respiratory centre in addition.
- Suffocation is also a possible cause of suffocation is a condition in which air is prevented from reaching the air passage by external prevention.
SIGNS AND SYMPTOMS OF ASPHYXIA
- The patient feels dizzy and weak.
- Difficulty in breathing.
- Later the breathing may become noisy.
- The pulse is rapid but as the condition worsens, it becomes slow and irregular.
- The neck veins might swell.
- Cyanosis (bluish discoloration of the skin, nailed, membrane) may be present (patient may be semi conscious)
Aim
- To restore adequate breathing and transfer.
MANAGEMENT
- Immediately remove obstruction or remove the casualty
- Ensure free passage for air especially for unconscious patients protecting the tongue obstructing the air way
- If the casualty is conscious re – assure as you wait for transport.
- If unconscious just keep a clear air way as you keep an eye on breathing.
- Seek medical advice if you have doubt about the medical condition.
- If there is frothing at the mouth.
- If there is cyanosis.
- If there is confusion.
- If the level of responsiveness is getting low.
- And if there is a change in breathing.
MANAGEMENT OF ASPHYXIA DEPENDING ON THE CAUSE
- Drowning: while artificial respiration is being performed, instruct by standers to remove wet clothing as far as practicable and wrap the casualty in dry blanket or other dry clothing.
- Choking: to dislodge the obstruction, bend the casualty’s head and shoulder forward or in case of a small child, hold him upside down and thump his back hard between the shoulder blades. If this is not successful encourage vomiting by passing two fingers right to the back of the casualty’s throat.
- Swelling of the tissues within the throat: If breathing has not ceased or when it has been restored, or give ice to sock or failing, ice cold water to sip. Butter, olive oil or medicinal paraffin may also be given.
- Suffocation by smoke: Protect yourself by tying a towel, hand kerchief or cloth, preferable wet, over your mouth and nose. Keep low and remove the casualty as quickly as possible.
- Suffocation by poisonous gas: Before entering any closed space known or suspected to contain poisonous gas of any kind, take a deep breath and hold it. Ensure a free circulation of air by opening or if necessary by breaking doors or windows.
- Hanging, strangling and throttling:
- Hanging: This involves suspension of the body. Grasp the lower limbs and raise the body. Free the neck by loosening or cutting the rope. Do not wait for a police man.
- Strangling: This is cutting off the air supply by constricting the neck. Cut and remove the band constricting the throat.
- Throttling: This is cutting off air supply by squeezing a person’s throat.
SIGNS AND SYMPTOMS
- For the case of hanging, the body might be still hanging
- If the person has not died, the pulse rate is high/ rapid, breathing is rapid, cyanosis, conscious is impaired, congestion of the face.
- Neck veins are prominent (large or protruding)
- There might be marks to indicate where the rope passed.
- Sometimes constriction (squeeze) may still be visible around neck, e.g. a scarf or it may be hidden in the folds of the skin e.g. wire.
AIM OF TREATMENT
- Restore adequate breathing and arrange moving to hospital.
MANAGEMENT
- Remove the constriction immediately, supporting the weight of the body if hanging.
- If there is knot, cut below it (a knot is difficult to cut and it may be useful evidence).
- If the casualty is unconscious, open the air way and check breathing. Complete ABC of resuscitation if required and place the casualty in the recovery position.
- Arrange for shifting to hospital.
Note: seek medical aid even if recovery seems complete.
SUFFOCATION
Suffocation results when air is prevented from reaching the air passages by external obstruction such as a plastic bag, soft pillow or a fall on sand. A baby may be suffocated through lying face down on a pillow or cushion.
GENERAL SIGNS AND SYMPTOMS:
- Difficulty in breathing. The rate and depth of breathing increases.
- Breathing may become noisy with snoring or gurgling. (low bubbling sound)
AIM
- Restore supply of air to the casualty and seek medical aid.
MANAGEMENT
- Immediately remove any obstruction or move the casualty to fresh air.
- If the casualty is conscious and breathing, reassure and observe.
- If the casualty is unconscious, open air way and check breathing. Complete the ABC of resuscitation if required and place the casualty in recovery position.
- Seek medical aid, if in doubt about the condition, arrange moving to hospital.
- Possible frothing at the mouth.
- Blueness of face, lips and finger nails (cyanosis)
- Confusion
- Lowering of level of responsiveness
- Possible unconsciousness.
- Breathing may stop.
CARDIAC ARREST
Cardiac arrest is a sudden stoppage of the heart resulting in adequate cerebral circulation, which leads to coma within one minute but recovery would be complete if the oxygen deficiency is relieved within 3 minutes.
If oxygen deficiency exceeds more than 4 – 6 minutes severe and permanent brain damage will occur.
CAUSES OF CARDIAC ARREST
- Heart attack and myocardial infarction
- Obstruction in the cardiac (heart) circulation.
- Injury to the heart.
- Electrolytes imbalances.
- Lack of oxygen to the heart.
- Severe drug reaction.
- Electric shock
- Due to anesthetic drugs.
- Severe bleeding.
SIGNS AND SYMPTOMS OF CARDIAC ARREST
- Absence of pulse in the major arteries like carotid or femoral arteries
- The patient will be unconscious
- The skin color will turn into blue (cyanosis)
- Respiration will stop.
- Pupils are widely dilated.
- If the operation is in progress there will be no bleeding or if there is bleeding it will stop.
FIRST AID MANAGEMENT
AIMS
- To save life.
- To preserve life.
MANAGEMENT OF CARDIAC ARREST
- First confirm the diagnosis (unconscious, death like appearance, no pulse and no respiration)
- Call for help e.g. passersby and an ambulance.
- Remove tight clothes around the neck, chest, waist, etc which may interfere with circulation.
- Place the casualty on spine position on a firm ground or a hard board.
- Do not waste time and start cardiopulmonary resuscitation(CPR)
- Follow ABC of resuscitation.
- A – Form airway clearance, i.e. remove vomits, secretions or any dentures.
- B – For breathing, i.e. assist breathing by artificial means.
- C – For circulation i.e. chest circulation by chest compression.
- Continue chest compressions and mouth to mouth respiration at the rate of 5:1.
- Hyperextend the neck by tilting. It back ward as far as possible and start artificial respiration (mouth to mouth respiration) with chest compressions.
- Monitor vital signs such as level of response, pulse, check papillary reaction which indicated successful efforts.
- Continue basic life support and transport the patient to hospital.
POISOINING
Poison is any substance which when taken into the body in sufficient quantities it can cause injury to health or it can completely destroy life. It is taken either accidently or intentionally.
HOW POISONS ENTER THE BODY
Poisons enter using different ways;
- They can be ingested (swallowed). This is by eating or drinking a poisonous substance. When eaten, they enter the circulatory system through the walls of intestines.
- Inhalation: Of fumes/ gases or even smoke from poisonous substance.
- Injection. What is intravenously introduced into the body may be poisonous.
- By contact. For example if a strong acid or spray comes into contact with the skin.
EFFECTS OF THE POISONS TO OUR BODIES
When poisons reach inside the body, they act in the ways:
- Once in the blood stream, they can affect the central nervous system whereby they prevent some vital activities like breathing.
- They may affect action of the heart and even other vital organs.
- They can also disturb oxygen distribution.
- When poisons reach the brain, the person may have convulsion or may be delirious.
- A poison which is swallowed, it affects the food passages directly causing vomiting, pain and sometimes diarrhea.
- If a person has taken a corrosive poison, it will burn the lips, mouth and the whole of the food passage.
- Inhaled poisons will cause severe respiratory distress.
- An over load of poisons will damage the body’s poison filter, i.e. kidney and liver.
- Poison in the digestive system can cause vomiting, abdominal pain and diarrhea.
- Poison in the blood may interfere with the red blood cells and if these red blood cells are disturbed, they may not carry adequate oxygen to the tissues.
TYPES OF POISON
- Food poisoning
- Drug poisoning
- Alcohol poisoning
- Industrial poisoning
AIMS OF FIRST AID:
- To maintain the airway, breathing and circulation.
- To identify the type of poison.
- To obtain medical aid.
- Aim at removing any contaminated clothing or article.
- Remove the casualty from danger.
GENERAL TREATMENT FOR POISON
- Seek for medical aid as soon as possible because the case may become medical legal
- Save the container
- Do not throw away the vomits in case of vomiting.
- If the casualty is unconscious put in prone position with the head turned to one side.
- You can also lay the patient in lateral position if the patient is vomiting.
- And continue watching the breathing
- Start artificial respiration if necessary.
- If the patient is conscious, you can give salty water or warm water to induce vomiting and also dilute the poison.
FOOD POISONING
Food poisoning, also known as foodborne illness, refers to the illness caused by consuming contaminated food or beverages.
Contamination can occur due to the presence of harmful microorganisms such as bacteria, viruses, parasites, or toxins produced by certain bacteria or molds. When ingested, these contaminants can cause adverse reactions in the body, resulting in food poisoning.
Common Causes of Food Poisoning
Food poisoning can be caused by various factors, including:
1. Bacterial Contamination Bacterial contamination is a leading cause of food poisoning. Bacteria such as Salmonella, Escherichia coli (E. coli), Campylobacter, and Listeria monocytogenes can contaminate food during production, processing, handling, or storage. Improper cooking, inadequate refrigeration, and poor hygiene practices can contribute to bacterial growth and subsequent foodborne illness.
2. Viral Contamination Viruses such as rotavirus, and hepatitis A can contaminate food and cause food poisoning. Viral contamination often occurs through improper hand hygiene by food handlers or exposure to fecal matter during food preparation.
3. Parasitic Contamination Parasites such as Giardia, Cryptosporidium, and Toxoplasma can contaminate food and water sources. Consuming raw or undercooked contaminated meat, seafood, fruits, or vegetables can lead to parasitic infections and subsequent food poisoning.
4. Toxins and Chemicals Toxins produced by certain bacteria, such as Staphylococcus aureus and Clostridium botulinum, can contaminate food and cause food poisoning. Chemical contaminants, including pesticides, heavy metals, and cleaning agents, can also lead to foodborne illness if present in unsafe levels
MANAGEMENT
It is caused by eating contaminated food (by bacteria).
THE PERSON MAY PRESENT WITH;
- Gastrointestinal Symptoms Gastrointestinal symptoms are predominant in food poisoning and may include nausea, vomiting, abdominal pain, diarrhea, and sometimes bloody stools.
- Systemic Symptoms In some cases, food poisoning can also cause systemic symptoms such as fever, headache, muscle aches, fatigue, and weakness. (Some times may go into shock)
TREATMENT
- Give plenty of fluids to prevent dehydration.
- If the poison was corrosive, do not induce vomiting.
- Collect and keep any vomitus for examination.
- For corrosive substances give milk or water to dilute.
- For example if one has taken an acid, you can give an alkaline like sodium bicarbonate to counteract.
- And if it was a strong alkaline, you give a weak acid. A weak acid could be lime juice (2 spoons full in a pile of water).
- You give soothing drinks, while egg, rice water. And still arrange to transfer the casualty.
Prevention of Food Poisoning
Prevention is key in reducing the risk of food poisoning. Effective preventive measures include:
1. Safe Food Handling Practicing proper hand hygiene, using clean utensils and surfaces, and preventing cross-contamination between raw and cooked foods are essential for safe food handling.
2. Proper Cooking and Storage Cooking foods thoroughly and maintaining proper storage temperatures to prevent bacterial growth are vital in reducing the risk of food poisoning.
3. Hygiene Practices Maintaining personal hygiene, such as regular handwashing, especially before food preparation, can help prevent foodborne illness.
4. Avoiding Cross-Contamination Separating raw and cooked foods and using different utensils and cutting boards for each can prevent cross-contamination and reduce the risk of food poisoning.
ALCOHOL POISONING
Alcohol poisoning refers to a severe and potentially fatal condition that occurs when an individual’s blood alcohol concentration rises to toxic levels.
It happens when a person consumes a large amount of alcohol within a short period. Alcohol is a depressant that affects the central nervous system, and when consumed excessively, it can lead to significant impairment of vital functions.
Signs and Symptoms of Alcohol Poisoning
Common signs and symptoms include:
1. Mental and Behavioral Symptoms
- Confusion and disorientation
- Agitation or aggression
- Delirium or unconsciousness
- Slow or irregular breathing
- Seizures
2. Physical Symptoms
- Pale or bluish skin
- Vomiting or retching
- Hypothermia (low body temperature)
- Slow heart rate
- In severe cases, respiratory failure or cardiac arrest
Immediate First Aid for Alcohol Poisoning
When encountering a person with alcohol poisoning, it is essential to take immediate action while waiting for emergency medical assistance. Follow these steps:
- Call for Help / Emergency Assistance Contact emergency services and provide them with accurate information about the person’s condition and the amount of alcohol they have consumed.
- Stay with the Person Do not leave the individual alone, especially if they are unconscious or experiencing severe symptoms. Stay with them to monitor their condition and provide reassurance.
- Monitor and Support Breathing Check the person’s breathing and make sure they are lying on their side in the recovery position to prevent choking on vomit. If breathing becomes irregular or stops, be prepared to perform CPR if you are trained to do so.
- Do Not Leave the Person Alone Continue to monitor the person’s vital signs, mental status, and breathing until medical professionals arrive.
Complications
Alcohol poisoning can have severe consequences and potential long-term effects, including:
- Brain damage due to lack of oxygen
- Liver damage or alcoholic hepatitis
- Damage to the gastrointestinal system
- Increased risk of accidents or injuries
- Worsening of existing health conditions
Prevention of Alcohol Poisoning
Preventing alcohol poisoning involves responsible drinking practices and promoting a safe drinking environment,
- Responsible Drinking Drink alcohol in moderation and know your limits. Pace yourself, alternate alcoholic beverages with non-alcoholic ones, and avoid drinking games or excessive peer pressure.
- Know Your Limits Understand your tolerance for alcohol and know when to stop drinking. Avoid trying to keep up with others or exceeding your personal limits.
- Avoid Peer Pressure Resist peer pressure to drink excessively or engage in risky behaviors. Surround yourself with supportive friends who respect your choices.
- Education and Awareness Promote education and awareness about the risks of alcohol poisoning. Encourage open conversations about responsible drinking and the importance of looking out for one another.
DRUG POISONING
Drug poisoning refers to the harmful effects caused by the ingestion, inhalation, or exposure to excessive amounts of medication or drugs.
It can occur due to accidental overdoses, intentional self-harm attempts, adverse reactions to medications, or interactions between different drugs.
TYPES OF DRUG POISONING
- Accidental Overdose Accidental overdose happens when a person unintentionally takes an excessive amount of a medication or drug, either due to misreading labels, miscalculations, or improper dosing.
- Intentional Overdose Intentional overdose occurs when an individual purposely takes an excessive amount of a medication or drug with the intent to harm oneself or commit suicide.
- Adverse Reactions Adverse drug reactions can lead to drug poisoning. Some individuals may have a hypersensitivity or allergic reaction to certain medications, resulting in severe and potentially life-threatening symptoms.
- Drug Interactions Drug interactions can occur when two or more medications or drugs interact with one another, leading to unexpected side effects or toxicity.
Signs and Symptoms of Drug Poisoning
The signs and symptoms of drug poisoning can vary depending on the type of drug involved and individual factors. Common manifestations include:
1. Central Nervous System Symptoms
- Confusion or disorientation
- Agitation or restlessness
- Drowsiness or coma
- Seizures or convulsions
- Hallucinations or delirium
2. Cardiovascular Symptoms
- Rapid or irregular heartbeat
- High blood pressure
- Chest pain or tightness
- Palpitations or arrhythmias
3. Respiratory Symptoms
- Shallow or labored breathing
- Slow or irregular breathing
- Respiratory distress or failure
TREATMENT.
- If the casualty is conscious, help him to be in a comfortable position and ask him what he has taken.
- Monitor and record the vital signs and if necessary transport or refer.
Prevention of Drug Poisoning
- Proper Medication Use Follow prescribed dosages, administration instructions, and recommended durations when taking medications. Avoid self-medicating or altering dosages without medical advice.
- Awareness of Drug Interactions Be aware of potential drug interactions between prescribed medications, over-the-counter drugs, and herbal supplements.
- Storage and Disposal of Medications Store medications securely and out of reach of children or individuals who may misuse them. Dispose of expired or unused medications properly to prevent accidental ingestion.
- Seeking Professional Help If struggling with substance abuse or mental health issues, seek professional help. Proper treatment and support can reduce the risk of drug poisoning and promote overall well-being.
INDUSTRIAL POISOINING
Industrial poisoning occurs when individuals are exposed to hazardous substances present in industrial environments.
These substances can enter the body through inhalation, ingestion, or skin contact. Industrial poisons can be in the form of chemicals, heavy metals, or biological agents, and their toxic effects can range from acute to chronic.
Common Types of Industrial Poisons
- Chemical Poisons Chemical poisons are substances that have toxic properties and can cause harm to humans upon exposure. Examples include solvents, pesticides, acids, alkalis, and industrial gases, Carbon monoxide (toxic), irritant gases like ammonia and many others.
- Heavy Metal Poisons Heavy metal poisons, such as lead, mercury, cadmium, and arsenic, are metallic elements that can accumulate in the body over time, leading to chronic poisoning and organ damage.
- Biological Poisons Biological poisons are toxic substances produced by living organisms, such as bacteria, fungi, or plants. They can cause various diseases and health problems when individuals are exposed to them in industrial settings.
Signs and Symptoms of Industrial Poisoning
The signs and symptoms of industrial poisoning can vary depending on the specific toxic substance involved, the duration and intensity of exposure, and individual factors. Some common manifestations include:
1. Acute Symptoms
- Difficulty breathing or shortness of breath
- Nausea, vomiting, or abdominal pain
- Dizziness or lightheadedness
- Skin rashes or irritation
- Headaches or migraines
2. Chronic Symptoms
- Fatigue or weakness
- Memory loss or cognitive difficulties
- Chronic respiratory problems
- Organ dysfunction or failure
- Development of cancers or other long-term health conditions
GENERAL ROLES FOR TREATMENT OF SWOLLOWED POISONS
- Get medical aid as soon as possible.
- Keep only container which you think might help to identify the poison.
- Check for any signs of burning on the lips. And if the mouth is okay, you can induce vomiting.
- If the casualty is conscious, give fluids to dilute the poison.
- Where possible give an anti – dot.
- Give soothing drinks.
- Treat shock if necessary.
- Keep the casualty warm.
- Loosen any tight, clothing.
- If unconscious, put in a semi prone position, watch.
- Breathing and give artificial respiration if necessary.
PREVENTION OF POISONING
- All medicine bottles and pockets should be labeled containers with unlabeled medicines should not be used.
- For toxic medicines, indicated the word poison on the container to enable any person that it’s dangerous.
- And put them under lock.
- Never take medicine where the label isn’t clear.
- Always read the label 3 times.
- Label substances used for specific purposes.
- And all poisonous substances should be kept out reach of children.
- For these cases , as a first aider, always make sure you obey safety regulations so that you don’t become the second victim.
- For most of these poisons, you should neutralize so that they are not very harmful.
- In some cases, stomach wash out is done.
Question: What is done for a person who has taken?
- Acid
- Alkali
- Mercury poisoning
- Opium
Acid Poisoning:
- Immediately call emergency services or poison control for assistance.
- While waiting for help, carefully remove any contaminated clothing and rinse the affected areas with copious amounts of water for at least 20 minutes.
- Do not induce vomiting unless specifically advised to do so by medical professionals.
- Keep the person calm and reassured until medical help arrives.
Alkali Poisoning:
- Contact emergency services or poison control immediately.
- Rinse the affected areas with large amounts of water for at least 20 minutes to dilute the alkali.
- If the substance was ingested, give the person small sips of water or milk, unless they are unconscious or experiencing convulsions.
- Do not induce vomiting.
- Stay with the person until medical assistance arrives.
Mercury Poisoning:
- In cases of elemental mercury exposure (liquid mercury), avoid direct contact and prevent further spread by isolating the area.
- If mercury is present on the skin or clothing, do not touch it with bare hands. Use gloves or a barrier to remove the mercury if possible.
- Ventilate the area by opening windows and doors to allow the mercury vapor to disperse.
- Contact emergency services or poison control for guidance on proper disposal and cleanup of the mercury.
- Seek medical attention to assess the extent of exposure and receive appropriate treatment.
Opium Poisoning:
- If someone has ingested opium and is unconscious or having difficulty breathing, call emergency services immediately.
- Do not induce vomiting unless advised to do so by medical professionals.
- Keep the person lying on their side to prevent choking on vomit.
- Monitor their breathing and provide first aid, such as CPR, if necessary.
- Provide all relevant information about the substance and its ingestion to medical professionals.


Good information
Thanks for the good and arranged notes🙏👍