Table of Contents
TogglePELVIC INFLAMMATORY DISEASES (PID)
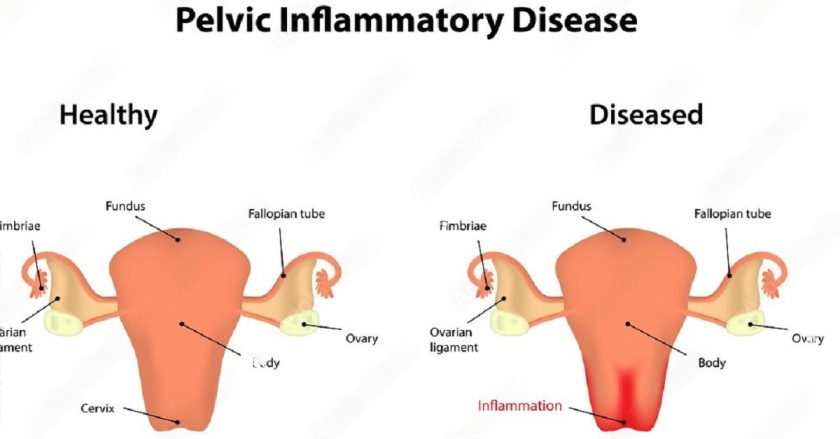
Pelvic Inflammatory Diseases (PID) refer to infections that affect the pelvic organs, pelvic peritoneum, and the pelvic vascular system.
The pelvic organs include the Fallopian tubes, Ovaries, Cervix, and Endometrium.
Causes of Pelvic Inflammatory Diseases
Ascending infections: These occur when bacteria from the vagina or cervix travel upwards into the reproductive organs, such as the Fallopian tubes and ovaries.
Haematogenous infections: Infections that are spread through the bloodstream to reach the pelvic organs.
Direct spread from infected neighboring organs: For example, an infected appendix can spread the infection to the pelvic region.
Causative Organisms
Several microorganisms can cause PID, including:
- Neisseria gonorrhoeae
- Chlamydia trachomatis
- Haemophilus influenzae
- Escherichia coli (E. coli)
Risk Factors
Certain factors increase the risk of developing PID, including:
- History of sexually transmitted infections (STIs), especially gonorrhea and Chlamydia.
- Bacterial vaginosis, an imbalance in vaginal bacteria.
- Having multiple sexual partners.
- Douching, which can disrupt the natural balance of vaginal flora.
- Previous history of PID, increasing the risk of recurrence.
- Use of intrauterine contraceptive devices (IUDs).
- Undergoing surgical procedures like dilation and curettage.
- Obstetric causes such as abortion, ectopic rupture, and puerperal sepsis.
Pathophysiology
PID is often caused by multiple microorganisms, with gonorrhea and Chlamydia being common culprits. The infection typically starts in the vagina and then ascends through the endocervical canal to reach the Fallopian tubes and ovaries. During menstruation, the endocervical canal is slightly dilated, facilitating the entry of bacteria into the uterus. Once inside the reproductive tracts, the bacteria rapidly multiply and can spread further to the fallopian tubes, ovaries, and even the peritoneum or other abdominal organs.
Clinical Manifestations
The clinical presentation of PID can vary, and common symptoms include:
On History Taking:
Severe Lower Abdominal Pain: Approximately 70% of individuals with PID experience intense pain in the lower abdomen. This pain can be localized or diffuse and may worsen during movement or sexual activity.
Acute Fever: Around 40% of PID cases present with a fever. The body’s elevated temperature is a response to the infection and inflammation.
Purulent Vaginal Discharge: About 90% of PID patients have purulent (pus-like) vaginal discharge. The discharge may have a foul odor and appear yellowish or greenish.
Menstrual Changes: PID can disrupt the normal menstrual cycle, leading to various menstrual irregularities. These changes may include dysmenorrhea (painful periods), menorrhagia (heavy or prolonged periods), or oligomenorrhea (infrequent or scanty periods).
On Examination:
During a physical examination, the following signs may be observed:
Signs of Inflammation: Inflammatory responses, such as redness, warmth, and swelling, may be evident in the pelvic region.
Peritoneal Signs: Abdominal examination may reveal signs of peritonitis, such as guarding (tensing of abdominal muscles), abdominal distension (swelling), and rebound tenderness (pain when pressure is released from the abdomen).
Vaginal Examination: A pelvic examination is crucial to assess the condition of the pelvic organs.
Vaginal Changes: The vaginal walls may appear red, inflamed, and dry due to the ongoing inflammation.
Tender Fornices: Palpation of the vaginal fornices (areas around the cervix) may reveal tenderness, especially in cases of pyosalpinx (accumulation of pus in the Fallopian tubes).
Purulent Discharge: A healthcare provider may notice the presence of purulent discharge during the examination.
CERVICITIS:
Cervicitis refers to the inflammation of the cervix, which is the lower part of the uterus that opens into the vagina. It is often caused by infections, most commonly sexually transmitted infections (STIs) like Chlamydia and Gonorrhea.
Signs and Symptoms of Cervicitis:
Redness of the Cervix: Inflammation may cause the cervix to appear red and swollen when examined by a healthcare provider.
Slight Bleeding on Intercourse: Cervicitis can lead to cervical friability, making the cervix more prone to bleeding, especially during sexual intercourse.
Itching and Burning: Some individuals with cervicitis may experience itching and a burning sensation around the vaginal area.
Vaginal Discharge (D/C): An abnormal vaginal discharge, which may be watery, yellowish, or greenish, can be present in cervicitis.
Pelvic Pain: Some individuals may experience mild pelvic discomfort or pain.
SALPINGITIS:
Salpingitis is the inflammation of one or both fallopian tubes. It often occurs as a result of infections ascending from the vagina and uterus. Common causes of salpingitis include untreated or inadequately treated STIs, particularly Chlamydia and Gonorrhea.
Signs and Symptoms of Salpingitis:
Abdominal or Back Pain: Salpingitis can cause lower abdominal or back pain, which may range from mild to severe.
Dyspareunia: Pain during sexual intercourse, known as dyspareunia, can be a symptom of salpingitis.
OOPHORITIS:
Oophoritis is the inflammation of one or both ovaries. It can occur independently or in conjunction with other pelvic infections, such as salpingitis.
Signs and Symptoms of Oophoritis:
Abdominal or Back Pain: Similar to salpingitis, oophoritis may cause abdominal or back pain.
Dyspareunia: Pain during sexual intercourse may also be present in cases of oophoritis.

ENDOMETRITIS:
Endometritis is the inflammation of the endometrium, which is the inner lining of the uterus.
It can be acute or chronic and is often caused by bacterial infections, most commonly occurring after childbirth, abortion, or the insertion of an intrauterine contraceptive device (IUD).
Signs and Symptoms of Endometritis:
Fever: The patient may have an elevated body temperature as a response to the infection.
Abdominal Pain: Pain or discomfort in the lower abdomen is a common symptom.
Enlargement of the Uterus: In some cases, the uterus may appear larger than usual upon examination.
Vaginal Discharge: Abnormal vaginal discharge may be present, which can be foul-smelling and may vary in color.
HOSPITAL MANAGEMENT:
AIMS:
- Prevent complications
- Relieve pain
- Prevent the disease from spreading
Admission:
- Admit the patient to a clean and well-ventilated gynecological ward for complete bed rest.
- Start an I.V. line immediately to prevent dehydration and encourage oral fluids.
Position:
- Place the patient in a comfortable position, especially semi-fowler’s, to aid discharge drainage.
Histories and Examination:
- Take patient histories and conduct a comprehensive general examination.
Observations:
- Monitor vital signs (TPR & BP).
- Observe and record color, amount, and smell of the discharge daily.
- Monitor the general condition of the patient.
Investigations:
- Conduct high vaginal swab for culture and sensitivity to identify the causative organism.
- Perform urinalysis for culture and sensitivity.
- Rule out malaria with a malaria slide.
- Take a blood sample for culture and sensitivity to check for a hematogenous source.
- Perform an ultrasound scan to rule out other causes of abdominal pain.
Diet:
- Advise the patient to take a highly nutritious diet with plenty of oral fluids.
Elimination:
- Provide a bedpan or urinal and advise the patient to urinate whenever needed.
- Observe and record the color, amount, and smell of the urine.
- Disinfect urine and feces with JIK before disposal.
Hygiene:
- Make the bed daily and remove wrinkles for cleanliness.
Exercise:
- Encourage the patient to do some physical exercise, such as walking around. Psychotherapy may be necessary.
Care of Mind:
- Reassure the patient and relatives.
- Provide newspapers, TV, radios, etc.
Medical Treatment:
- Start treatment immediately while waiting for culture and sensitivity results.
- Use broad-spectrum antibiotics (chloramphenicol 2 gm stat, then I gm 6 hourly for 5 days, gentamicin 160 mg OD for 5 days, ceftriaxone 2 gm daily for 5 days). If the discharge reduces, switch to oral antibiotics.
- Use other drugs based on sensitivity results (metronidazole 500 mg TDS i.v., azithromycin 1g as a single dose, ciprofloxacin, tetracycline, doxycycline, Septrin).
Analgesics:
- Use narcotics for severe pain. Other options include Panadol, ibuprofen, Diclofenac to reduce pain and inflammation.
Advice on Discharge:
- Reduce sexual partners, use condoms, avoid intrauterine contraceptive devices, seek early treatment for sexually transmitted infections, maintain hygiene, and follow prescribed drugs.
- Instruct the patient to return for review in case of any problems like pain, discharges, or itching.
Complications
Untreated or poorly managed endometritis can lead to several complications, including:
Pelvic Abscess: Accumulation of pus in the pelvic region.
Infertility: Inflammation and scarring can affect the fallopian tubes and reduce fertility.
Ectopic Pregnancy: An abnormal pregnancy outside the uterus, usually in the fallopian tubes.
Chronic Pelvic Pain: Persistent pelvic pain lasting for an extended period.
Pelvic Adhesions: Scar tissue formation that can cause organs to stick together.
Salpingitis: Inflammation of the fallopian tubes.
Peritonitis: Inflammation of the abdominal lining.
Tubal Ovarian Mass: Formation of masses involving the fallopian tubes and ovaries.
Intestinal Obstruction: Partial or complete blockage of the intestines.

Special thnxs 2 e initiation, bt some notes aren’t assessed n’t evn opening.
Thanks for helping , but some notes are not opening and seen THANKS 🙏