Table of Contents
ToggleNormal second stage of labour
The second stage of labor commences when the cervix is fully dilated and concludes with the delivery of the baby.
SIGNS OF SECOND STAGE
Premonitory signs
- Expulsive uterine contractions: Expulsive uterine contractions may occur when the mother is not fully dilated, particularly in occipital posterior position or with a full rectum.
- Rapture of fore waters: Rupture of fore waters can occur at any time during labor.
- Dilatation and gaping of the anus: Dilatation and gaping of the anus may happen due to deep engagement of the presenting part and premature maternal effort in the later part of the first stage.
- Appearance of presenting part: Appearance of the presenting part becomes evident. Excessive molding may lead to the formation of a large caput succedaneum, which can protrude through the cervix before full dilatation. In breech presentation, the presenting part may be visible when the cervix is only 7-8 cm dilated.
- Show: Show should be distinguished from bleeding caused by partial separation of the placenta, stretched cervix, or vaginal mucosa when the presenting part descends.
- Congestion of the vulva: Congestion of the vulva is due to enthusiastic premature pushing.
- Bulging of the perineum.
Confirmatory sign:
- No cervix is felt on VE (full dilatation – 10cm).
Stages:
Passive:
- The cervix is fully dilated, but there are no involuntary expulsive contractions. Labour that is progressing well may take one hour.
Active:
- The cervix is fully dilated, there are involuntary expulsive contractions, and the baby is visible. The doctor should be informed if the baby has not been delivered after 2 hours in primigravida and 1 hour in multigravida.
Phases:
Propulsive phase:
- It starts from full dilatation up to the descent of the presenting part to the pelvic floor.
Expulsive phase:
- It is distinguished by maternal bearing down efforts and ends with the delivery of the baby.
PHYSIOLOGY OF SECOND STAGE
Descent:
- Descent of the presenting part, which began during the first stage of labour and reaches its maximum speed towards the end of the first stage, continues its rapid pace through the second stage until it reaches the pelvic floor.
Uterine action:
- The contractions become stronger and longer but can be less frequent, allowing a mother and a fetus a recovery period during the resting phase. The recovery period may last for one hour and is longer in primigravidas than in multigravidas. They are of strong intensity and expulsive in nature.
- Membranes often rupture spontaneously at the onset of the second stage, so the drainage of liquor allows the hard round fetal head to be directly applied to the vaginal tissue, aiding distention.
- Fetal axis pressure increases flexion of the head, resulting in smaller presenting diameters, more rapid progress, and fewer traumas to both mother and fetus.
- Contractions become expulsive and as the fetus descends further into the vagina, pressure from the presenting part stimulates the nerve receptors in the pelvic floor, and the mother feels the need to push.
- Contractions become increasingly expulsive and overwhelming, and the mother responds by contracting abdominal muscles and the diaphragm.
Soft tissue displacement:
As the fetal head descends, the soft tissue of the pelvis becomes displaced.
- Anteriorly, the bladder is pushed upwards into the abdomen where it is at less risk of injury during the descent of the fetus. This results in stretching and thinning of the urethra, reducing its lumen.
- Posteriorly, the rectum becomes flattened in the sacral curve, and the advancing head expels any residual fecal matter.
- The levator ani muscles dilate, thin out, and are displaced laterally.
- The perineal body is flattened, stretched, and thinned.
- The fetal head is seen at the vulva advancing with each contraction and recoiling during the resting phase until crowning takes place.
- The head is born, and the shoulders and body follow with the next contraction, accompanied by a gush of amniotic fluid and sometimes blood.
MECHANISM OF NORMAL LABOUR
These are series of movements made by the fetus as it passes through the birth canal in order to be born.
OR: These are series of passive movements made by the fetus as it negotiates the curves and diameters of the pelvis in order to be born. There is a mechanism for every presentation and position which can be delivered vaginally.
Principles common to all mechanisms:
- Descent takes place throughout.
- Whichever part that leads and first meets the resistance of the pelvic floor will rotate forward until it comes under the symphysis pubis.
- The part that escapes under the symphysis pubis will pivot around the pubic bone.
- The fetus turns slightly to take advantage of the widest space in each plane of the pelvis, i.e., transverse at the brim and anteroposterior at the outlet.
TERMS USED
Attitude: This refers to the relationship of the fetal head and limbs to its trunk. The ideal attitude should be one of complete flexion. Flexion of the fetal head enables the smallest diameters to present to the pelvis, resulting in an easier labor.
Presentation: This indicates the part of the fetus that lies in the lower pole of the uterus. The normal presentation is vertex, where the head presents first.
Lie: This denotes the relationship between the long axis of the fetus and the long axis of the uterus. In normal labor, the lie should be longitudinal, which occurs in 99.5% of cases.
Position: This describes the relationship between the denominator of the presentation and specific points on the pelvic brim. Various positions are used in different presentations.
Right occipitoanterior:
- The occiput points to the right iliopectineal eminence.
- The sinciput points to the left sacroiliac joint.
- The sagittal suture is in the left oblique diameter of the maternal pelvis.
Left occipitoanterior:
- The occiput points to the left iliopectineal eminence.
- The sinciput points to the right sacroiliac joint.
- The sagittal suture is in the right oblique diameter of the maternal pelvis.
Right occipitoposterior:
- The occiput points to the right sacroiliac joint.
- The sagittal suture is in the right oblique diameter of the pelvis.
Left occipitoposterior:
- The occiput points to the left sacroiliac joint.
- The sagittal suture is in the left oblique diameter of the pelvis.
Right occipitolateral:
- The occiput points to the right iliopectineal line, midway between the iliopectineal eminence and the sacroiliac joint.
- The sagittal suture is in the transverse diameter of the pelvis.
Left occipitolateral:
- The occiput points to the left iliopectineal line, midway between the iliopectineal eminence and sacroiliac joint.
- The sagittal suture is in the transverse diameter of the pelvis.
Presenting part: This is the part of the presentation that lies over the internal os of the cervix.
Denominator: This is the name of the part of the presentation that is used when referring to the fetal position. Each presentation has a different denominator, which includes:
- In vertex presentation: occiput
- In breech presentation: sacrum
- In face presentation: mentum
In the mechanism of normal labor:
- Attitude is one of complete flexion.
- Lie is longitudinal.
- The presentation is cephalic.
- Position can be either right or left occipitoanterior.
- The denominator is the occiput.
- Presenting diameters are the biparietal and occipitofrontal.
- Engaging diameters are the biparietal (transverse) and suboccipitofrontal (anteroposterior).
MAIN MOVEMENTS
Engagement: Engagement occurs when the biparietal and suboccipitofrontal diameters pass through the pelvic brim. In primigravidas, engagement often happens before the onset of labor, while in most multigravidas, it occurs in the late first stage.
Descent: Throughout the first stage of labor, uterine muscle contractions and retraction reduce the space in the uterus, exerting pressure on the fetus to descend. After the rupture of the fore waters and with maternal effort, descent speeds up, culminating in the complete expulsion of the fetus. Factors facilitating descent include uterine contraction and retraction, bearing down efforts, and straightening of the fetus after the rupture of membranes.
Flexion: At the beginning of labor, with the position being right occipitoanterior (ROA) or left occipitoanterior (LOA), the fetus is in the attitude of complete flexion. At the onset of labor, the suboccipitofrontal diameter of 10cm presents. With greater flexion, the suboccipitobregmatic diameter of 9.5cm presents, and the occiput becomes the leading part. Resistance from the lower segment, pelvic walls, unfolding cervix, and pelvic floor promotes full flexion of the fetal head.
Internal Rotation of the Head: During a contraction, the presenting part is pushed downward onto the pelvic floor. It first meets resistance with the pelvic floor muscles and then rotates 1/8 of a circle forward, bringing the occiput under the symphysis pubis.
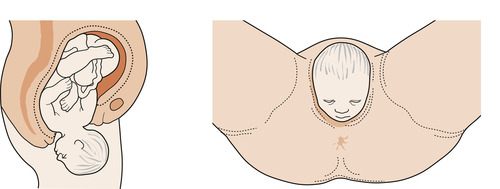
Crowning: With strong uterine contractions, crowning takes place as the occipital eminence escapes under the symphysis pubis and no longer recedes back during contractions. The widest diameter (biparietal) is born. If flexion is maintained, the suboccipitobregmatic diameter of 9.5cm distends the vaginal orifice.
Extension of the Head: After crowning, the fetal head can extend by pivoting on the suboccipital region around the pubic bone. This movement realizes the sinciput, face, and chin, which sweep the perineum and are born by extension.
Restitution: This is the movement of the head after delivery to correct the twist in the neck. The occiput rotates back 1/8 of a circle towards the side where it began.
Internal Rotation of the Shoulders: The shoulders enter the oblique diameter of the pelvic cavity. The anterior shoulder reaches the pelvic floor first and rotates 1/8 of a circle forward, bringing the shoulders in the anteroposterior (AP) diameter of the outlet to lie under the symphysis pubis. The movement can be clearly seen as the head turns at the same time (external rotation of the head). It occurs in the same direction as restitution, and the occiput of the fetal head now lies laterally.
External Rotation of the Head: It occurs at the same time as the internal rotation of the shoulders.
Lateral Flexion: The anterior shoulder escapes under the symphysis pubis, and the posterior shoulder sweeps the perineum. The whole body is born by lateral flexion towards the mother’s abdomen.
Factors Influencing the Length of the 2nd Stage:
- Maternal parity
- Fetal size
- Force of uterine contractions
- Presentation
- Position
- Pelvic size
- Method of anesthesia
- Magnitude of maternal expulsive effort
MANAGEMENT OF SECOND STAGE OF LABOUR
The woman should be reassured and provided with psychological support to encourage cooperation during the second stage of labor.
- Ensure the woman is not left alone and transfer her to the delivery room in a timely manner without rushing.
- Prepare the delivery room, necessary equipment, and a cot for the baby well in advance.
- Ensure a clean and decontaminated environment, with adequate lighting in the delivery room.
- Properly prepare oneself and any assisting personnel by wearing protective gear, washing hands thoroughly with clean water and soap, and wearing sterile gloves.
- Before conducting delivery, scrubbing and wearing protective gear should be done.
- Position the mother in a dorsal position for delivery.
NURSING CARE
- Care of the bladder: Encourage the mother to empty her bladder at the beginning of the second stage. A full bladder may delay the descent of the presenting part, and the bladder may be at risk of injury during the descent of the fetal head.
- Hygiene and comfort: Swab the vulva whenever necessary and provide a sterile pad to cover it between contractions. In case of leg cramps, massage, extend, and flex the leg to provide relief.
- Emotional support: Offer constant praise and keep the woman informed of her progress. Create a calm and quiet environment with privacy to reduce anxiety. Avoid unnecessary interruptions by other caregivers.
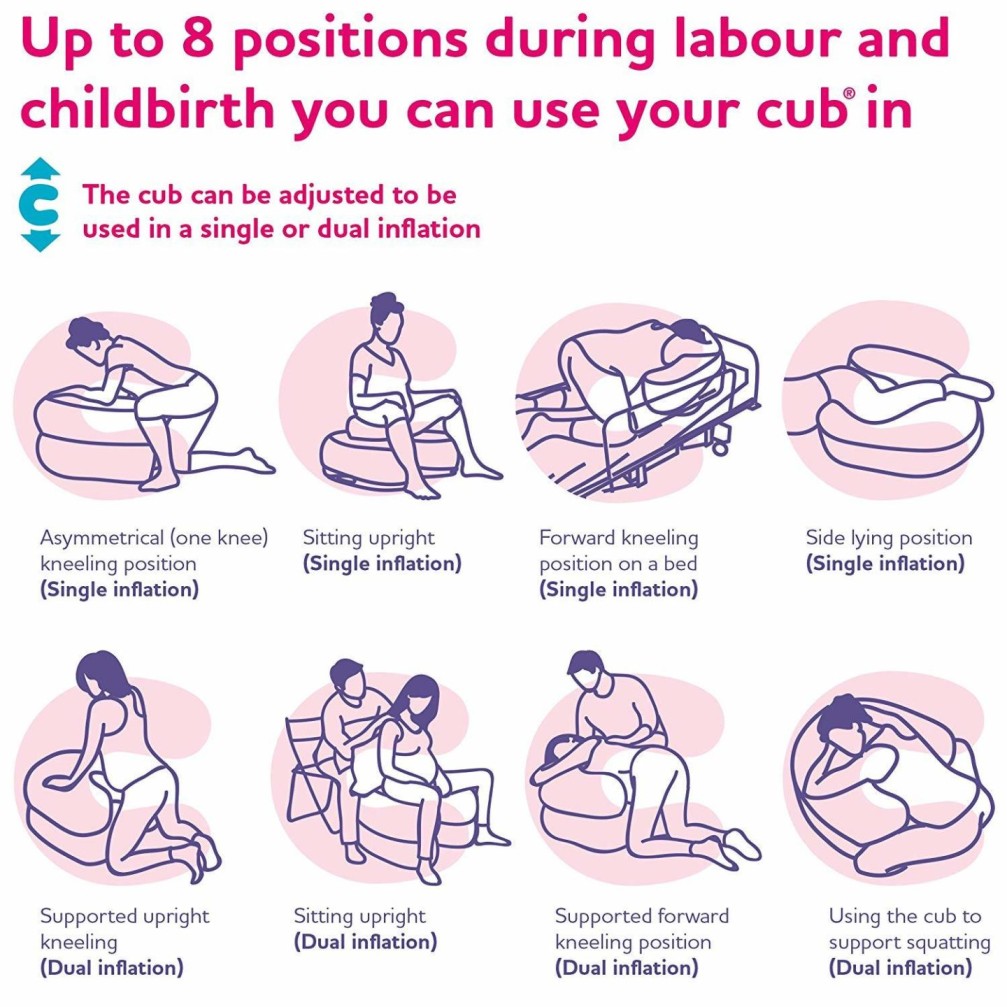
- Position: Consider using positions like squatting, kneeling, all fours, standing, left lateral position, or dorsal position during the second stage. These positions may improve the effectiveness of contractions and facilitate the process.
- Observations: Monitor the strength, length, and frequency of contractions. Observe the descent of the presenting part, fetal condition (e.g., fetal heart rate, color of amniotic fluid, molding, and state of membranes), and maternal condition (e.g., emotional coping ability, pulse every 30 minutes, and blood pressure hourly).
CONDUCTING 2ND STAGE ( ACTIVE MANAGEMENT)
Requirements
A trolley with;-
| Top Shelf | Bottom Shelf | Beside |
|---|---|---|
| Sterile delivery pack containing: | Vial of lignocaine | A warm cot and baby’s clothing |
| – 6 delivery swabs | Amp of oxytocin | Resuscitation equipment |
| – 2 cord clamps | Measuring jar | Gum boots |
| – 1 pair of cord scissors | Apron | 2 buckets (one for used gloves, swabs, etc., and one with disinfectant) |
| – 1 pair of episiotomy scissors | 2 pairs of sterile gloves | Hamper |
| – 2 gallipots for swabs and lotion | Episiotomy pack | Drip stand |
| – 2 receivers | Disinfectant | |
| – Bulb syringe (mucus extractor) | Syringe and needles | |
| – 2 syringes | Mackintosh and towel | |
| – Perineal pad | Clean pads | |
| – Four delivery towels | Safety box | |
| – Cord ligatures | ||
| – Sterile gloves | ||
| – 4 delivery towels |
Responsibilities of Assistant During 2nd Stage
Reassure the mother: Provide constant reassurance and emotional support to the mother throughout the second stage of labor to help her remain calm and focused.
Position the mother: Assist the mother in assuming the most comfortable and effective position for delivery, whether it’s dorsal, squatting, kneeling, all fours, standing, or left lateral position.
Instruct mother when to push: Guide the mother and provide clear instructions on when to push during contractions to facilitate the descent and delivery of the baby.
Listen to fetal heart: Monitor the fetal heart rate regularly, especially after each contraction, to assess the well-being of the baby during the delivery process.
Give oxytocin after delivery: Administer oxytocin to the mother within one minute after the baby’s delivery to help prevent excessive bleeding and facilitate uterine contractions.
Show the sex of the baby: After delivery, if requested, reveal the sex of the baby to the mother and her partner, respecting their preferences and cultural beliefs.
Score the baby: Perform the Apgar scoring at 1 minute and 5 minutes after birth to assess the baby’s overall health and well-being.
Ensure baby care: After delivery, ensure the baby is promptly dried, kept warm, and placed on the mother’s breast for skin-to-skin contact and initiating breastfeeding.
Procedure:
Explain the Procedure to the Mother: Communicate the entire delivery process to the mother, ensuring she understands what will happen during the second stage of labor. Address any questions or concerns she may have.
Put on Gum Boots, Gown, and Mask: Prior to conducting the delivery, don gum boots, wear a sterile gown, and put on a mask to maintain a hygienic environment and prevent the spread of infections.
Position the Mother: Assist the mother in assuming a comfortable position for delivery, such as dorsal, squatting, kneeling, all fours, standing, or left lateral position, depending on her preference and the progress of labor.
Scrub Hands before Conducting Delivery: Thoroughly scrub and clean your hands with soap and water to ensure they are free from any potential contaminants.
Put on Two Pairs of Sterile Gloves: Wear two pairs of sterile gloves to maintain a sterile field during the delivery process.
Swab the Perineum and Drape with Sterile Towels: Prepare the perineal area by swabbing it with an antiseptic solution to maintain cleanliness. Then, drape the delivery area and perineum with sterile towels to create a sterile field.
Place a Sterile Pad on the Anus: To prevent contamination from fecal matter, place a sterile pad over the anus, ensuring the delivery field remains clean and sterile.
Confirm 2nd Stage of Labor: Before proceeding, confirm that the mother has entered the second stage of labor, with full dilatation of the cervix and the presenting part of the baby ready for delivery.
Delivery of the Head:
- As the fetal head descends at the vulva, keep it flexed by applying pressure with two fingers of the left hand on the vertex, pointing towards the anterior fontanel.
- Use the right hand to place a small rectal pad to control fecal matter and maintain the sterile delivery field.
- Monitor the descent of the head with your fingers to prevent expulsive crowning and potential perineal laceration.
- The head should advance with each contraction. At crowning, ask the mother to stop pushing and pant to maintain pressure on the head and control the birth.
- Deliver the head slowly by extending it, bringing the occiput towards the symphysis pubis. Wipe the baby’s face, swab the eyes inside outwards, and clear the airway as soon as the head is born.
- During the resting phase, check for the umbilical cord around the baby’s neck. If it’s loose, slip it over. If tight, clamp it with two artery cord clamps and cut between them.
- Hold gauze over the incised area to reduce the risk of being sprayed with blood during the procedure.
Delivery of the Shoulders:
- Ensure restitution and external rotation of the head to safely deliver the shoulders and avoid perineal lacerations.
- External rotation of the head indicates that the shoulders are rotating into the anterior-posterior diameter of the pelvic outlet, ready to be delivered.
- Deliver one shoulder at a time to prevent overstretching of the perineum.
- Place a hand on each side of the baby’s head over the ears and deliver the anterior shoulder with a downward movement and the posterior shoulder with an upward movement, sweeping the perineum.
- Deliver the rest of the body towards the mother’s breast.
- Note the time of delivery and perform the Apgar score at 1 minute. Congratulate the mother and palpate the abdomen to rule out a second baby.
Immediate Care of the Newborn After Birth (Within the First Hour):
- Clamp and cut the cord.
- Clear secretions from the baby’s mouth and nostrils.
- Tightly ligature the cord.
- Warm the newborn and wrap it in a sterile warm towel.
- Place the baby on the mother’s breast if in good condition and not contraindicated.
- Perform the Apgar score at 5 minutes.
- Show the baby’s face and sex to the mother.
- Provide warmth to the mother.
- Put an identification tag on the baby with the mother’s name, time of delivery, sex, birth weight, and date of delivery.
- Note that the baby should have a strong and lusty cry, which helps the lungs expand.
Points to Consider While Conducting Delivery:
- Ensure all necessary equipment, including newborn resuscitation equipment, is available and the delivery area is clean and warm.
- Make sure the mother’s bladder is empty before delivery.
- Assist the woman in assuming a comfortable position of her choice.
- Stay with the mother and provide emotional and physical support throughout the process.
- Allow the mother to push as she wishes and avoid urging her to push.
- Decontaminate the delivery trolley and set up sterile equipment.
- Prepare the delivery environment, decontaminate the bed, and ensure adequate lighting.
- Put on protective gear such as a plastic apron and gum boots.
- Wear sterile gloves for the delivery procedure.
- Ensure controlled delivery of the baby’s head to prevent complications.
Factors Influencing the Length of the 2nd Stage of Labour:
- Maternal parity (number of previous pregnancies).
- Fetal size.
- Uterine contractile force and strength of contractions.
- Presentation of the baby (e.g., vertex or breech).
- Position of the baby during delivery (e.g., occipitoanterior or occipitoposterior).
- Size and shape of the maternal pelvis.
- Method of anesthesia used during labour, if any.
- The magnitude of maternal expulsive force.
Possible Complications of 2nd Stage of Labour:
- Deep transverse arrest (failure of the baby’s head to rotate and descend properly).
- Obstetrical shock (resulting from severe bleeding or other complications).
- Uterine inertia (weak or ineffective uterine contractions).
- Maternal distress (emotional or physical strain during labour).
- Shoulder dystocia (difficulty delivering the baby’s shoulders after the head is born).
- 3rd-degree tear (severe tear involving the perineum and anal sphincter).
- Amniotic embolism (rare but serious condition where amniotic fluid enters the mother’s bloodstream).
- Ruptured uterus (tearing of the uterine wall during labour).
- Fetal distress (abnormalities in the baby’s heart rate or well-being).

Interesting
work well done