MINOR DISORDERS OF PREGNANCY
Minor disorders of pregnancy are a series of commonly experienced symptoms related to the effects of pregnancy hormones and the consequences of enlargement of the uterus as the fetus grows during pregnancy.
These are referred to as minor because they are not life threatening.
The causes can be;-
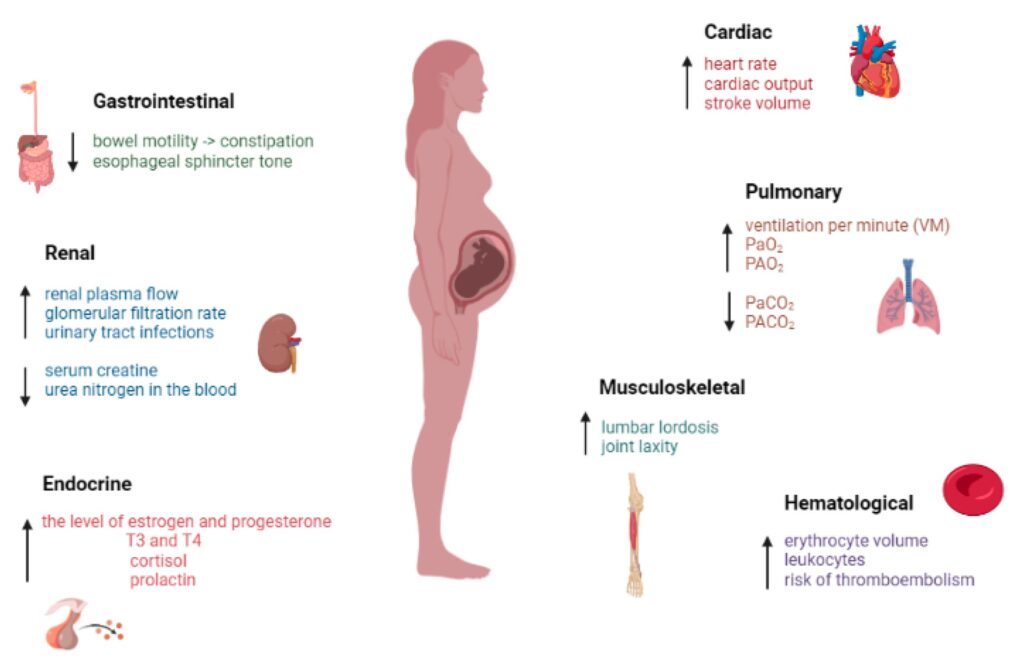
- Hormonal changes
- Accommodation changes
- Metabolic changes and
- Postural changes
I. Digestive System Disorders:
A. Nausea and Vomiting (Morning Sickness):
- Causes: Primarily attributed to hormonal surges, specifically elevated levels of human chorionic gonadotropin (hCG), oestrogen, and progesterone during early pregnancy (weeks 4-16).
These hormones affect the gastrointestinal tract’s sensitivity and motility. The exact mechanism remains unclear but likely involves alterations in brain neurotransmitters and gastrointestinal hormone levels.
Decreases as the placenta takes over hormone production. - Symptoms: Range from mild to severe vomiting (hyperemesis gravidarum, a severe form requiring medical attention).
Symptoms often peak in the morning but can occur throughout the day. - Management:
- Dietary Modifications: Small, frequent meals; consuming bland foods like crackers, toast, or rice; avoiding strong smells or triggers; consuming carbohydrates.
- Lifestyle Changes: Getting out of bed slowly, staying hydrated, eating before getting out of bed, regular, gentle exercise.
- Pharmacological Interventions: In cases of severe nausea and vomiting, antiemetics (medications to control nausea and vomiting) may be prescribed by a healthcare provider. Vitamin B6 supplements are sometimes recommended.
- Acupressure: Wristbands with pressure points can sometimes help alleviate nausea.
B. Heartburn (Pyrosis):
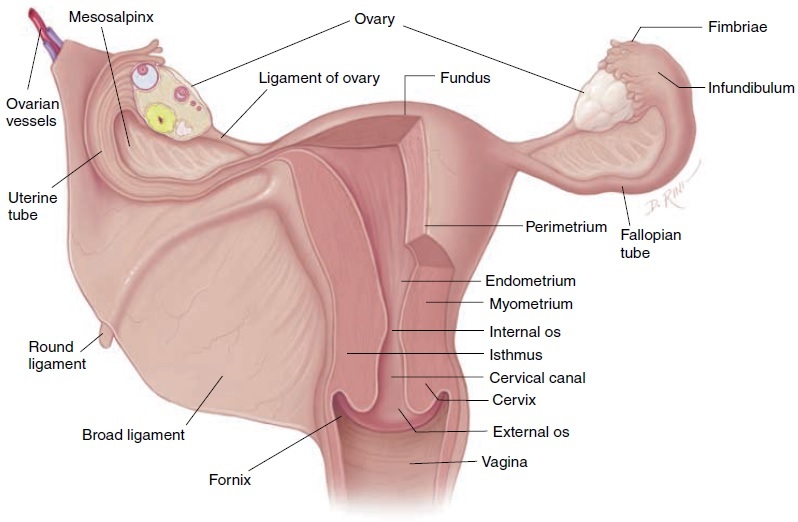
- Causes: Relaxation of the lower esophageal sphincter (LES) due to progesterone, allowing stomach acid to reflux into the esophagus. Increased intra-abdominal pressure from the growing uterus further exacerbates this. Most troublesome between 30-40 weeks gestation.
- Symptoms: Burning sensation in the chest, often radiating upwards. Can be worsened by lying down, bending over, or consuming certain foods.
- Management:
- Dietary Modifications: Small, frequent meals; avoiding fatty, spicy, or acidic foods; avoiding eating before bed.
- Lifestyle Changes: Elevating the head of the bed with extra pillows, avoiding tight clothing, maintaining an upright posture after meals.
- Pharmacological Interventions: Antacids (e.g., magnesium trisilicate, calcium carbonate) can neutralize stomach acid, providing temporary relief. H2 blockers or proton pump inhibitors (PPIs) may be prescribed for more severe cases.
C. Excessive Salivation (Ptyalism):
- Causes: Likely hormonal influences, although the exact mechanism is unclear. Often associated with nausea and vomiting. It may also be caused by anxiety or psychological factors.
- Symptoms: Excessive production of saliva.
- Management: Rinsing the mouth frequently, sucking on ice chips or hard candies, avoiding trigger foods. Counseling may be helpful to address underlying anxiety.
D. Constipation:
- Causes: Progesterone’s relaxing effect on the smooth muscles of the intestines, leading to slowed bowel movements (decreased peristalsis). Iron supplementation can also contribute. Decreased physical activity may play a role.
- Symptoms: Infrequent bowel movements, hard stools, straining during bowel movements.
- Management:
- Dietary Modifications: Increased intake of fiber (fruits, vegetables, whole grains), fluids (water), and gentle exercise. Bulk-forming laxatives (psyllium) may be used under medical supervision.
- Lifestyle Changes: Regular exercise, particularly walking, can stimulate bowel movements.
- Pharmacological Interventions: Stool softeners or mild laxatives should be used cautiously and only when dietary changes and exercise are insufficient, under the guidance of a healthcare professional.
E. Pica:
- Causes: Unknown. Possible links to nutritional deficiencies (iron, zinc), psychological factors, or hormonal imbalances.
- Symptoms: Craving and consumption of non-nutritive substances (e.g., clay, ice, starch). This can lead to serious health consequences.
- Management: Addressing any underlying nutritional deficiencies through dietary changes and supplementation under medical supervision. Psychological counseling may also be beneficial.
II. Musculoskeletal System Disorders:
A. Leg Cramps:
- Causes: Exact cause is unknown but various factors have been suggested, including:
- Changes in electrolyte balance: Decreased calcium or magnesium levels can make muscles prone to cramping.
- Compression of nerves: The growing uterus may compress nerves, affecting muscle function.
- Reduced blood circulation: Restricted blood flow can lead to cramping.
- Increased weight: Added weight puts pressure on the muscles.
Symptoms: Sudden, sharp pain in the calf muscles, often at night.
Management:
- Stretching exercises: Regular stretching of calf muscles.
- Hydration: Adequate fluid intake.
- Dietary changes: Addressing any potential electrolyte imbalances through diet or supplementation (calcium, magnesium, potassium). A balanced diet is key.
- Foot elevation: Raising legs above heart level. Dorsiflexion (pulling toes towards shin) can also provide relief.
B. Backache:
- Causes: Shifting center of gravity due to the growing uterus, relaxation of ligaments and joints due to relaxin hormone, and changes in posture.
- Symptoms: Aching or pain in the lower back, often radiating to the buttocks or legs.
- Management:
- Postural adjustments: Maintaining good posture, avoiding high heels, using supportive footwear.
- Exercise: Low-impact exercises such as walking, swimming, or prenatal yoga.
- Rest: Regular periods of rest throughout the day.
- Supportive measures: Using a maternity support belt, applying heat or ice packs, pelvic floor exercises.
- Pelvic floor exercises: Strengthening pelvic floor muscles can help improve support and reduce back pain.
III. Circulatory System Disorders:
A. Fainting (Syncope):
- Causes: In early pregnancy, vasodilation from progesterone can cause a temporary drop in blood pressure before the body compensates by increasing blood volume. Orthostatic hypotension (a sudden drop in blood pressure when standing up) can also occur. Dehydration can contribute.
- Symptoms: Dizziness, lightheadedness, loss of consciousness.
- Management: Avoiding prolonged standing, changing positions slowly, lying down immediately if feeling faint, staying well-hydrated. Avoiding lying on the back, except during necessary medical examinations.
B. Varicose Veins:
- Causes: Progesterone relaxes the smooth muscles in the veins, leading to reduced blood flow and pooling of blood. Increased blood volume and pressure from the growing uterus also contribute. They may occur in legs, vulva, and anus.
- Symptoms: Enlarged, twisted veins; aching, heavy, or swollen legs; pain or cramping in the legs.
- Management:
- Compression stockings: Wearing compression stockings to improve circulation.
- Elevation: Elevating legs regularly.
- Exercise: Regular exercise to promote circulation.
- Avoiding prolonged standing or sitting: Frequent movement to improve blood flow.
- Managing constipation: Preventing constipation helps reduce pressure on the veins.
- Medical intervention: In severe cases, a doctor may recommend other treatments.
C. Hemorrhoids:
- Causes: Increased pressure on the pelvic veins due to constipation and the growing uterus.
- Symptoms: Painful, swollen, and inflamed veins in the rectum or anus.
- Management: High-fiber diet to prevent constipation; topical treatments (e.g., creams, ointments); warm sitz baths; stool softeners (as advised by a healthcare provider).
D. Heart Palpitations:
- Causes: Increased cardiac output to supply the growing fetus with blood and nutrients. Hormonal changes also affect heart rate and rhythm. Anxiety and stress can also exacerbate palpitations.
- Symptoms: Feeling of a racing heart, fluttering, or pounding in the chest. Can be associated with shortness of breath or dizziness.
- Management: Identifying and managing underlying anxiety or stress. Regular exercise, maintaining a healthy weight, and avoiding caffeine and nicotine can help regulate heart rate. In cases of persistent or concerning symptoms, medical evaluation is necessary to rule out other causes.
IV. Urinary System Disorders:
A. Urinary Tract Infections (UTIs):
- Causes: The changing hormonal environment of pregnancy can make women more susceptible to UTIs. The expanding uterus can also compress the ureters, slowing urine flow and increasing the risk of bacterial growth.
- Symptoms: Frequent urination, burning sensation during urination, urgency, pain in the lower abdomen or back. Fever and chills may indicate a more serious infection.
- Management: Prompt medical attention is crucial for UTIs in pregnancy. Treatment usually involves antibiotics.
B. Frequency of Micturition:
- Causes: In early pregnancy, hormonal changes increase blood flow to the kidneys, leading to increased urine production. In later pregnancy, the enlarging uterus compresses the bladder, reducing its capacity and leading to more frequent urination.
- Symptoms: Increased urge to urinate, often with small amounts of urine being passed.
- Management: Regular voiding to prevent bladder distension, drinking plenty of fluids throughout the day but avoiding excess fluid close to bedtime. Kegel exercises to strengthen pelvic floor muscles may help improve bladder control.
C. Stress Incontinence:
- Causes: Weakening of pelvic floor muscles due to hormonal changes and the pressure exerted by the growing uterus.
- Symptoms: Leakage of urine during coughing, sneezing, laughing, or physical exertion.
- Management: Pelvic floor exercises (Kegel exercises) to strengthen the pelvic floor muscles. Avoiding activities that increase intra-abdominal pressure. In some cases, medical intervention may be necessary.
V. Integumentary System Disorders:
A. Itching of the Skin (Pruritis):
- Causes: Stretching of the skin due to weight gain, hormonal changes, and cholestasis of pregnancy (a liver condition that can cause intense itching). Poor hygiene, heat rash, or minor skin rashes also contribute. Stretch marks (striae gravidarum) can also be itchy.
- Symptoms: Itching, particularly on the abdomen, breasts, thighs, and buttocks. The degree of itchiness can range from mild to severe.
- Management: Keeping the skin moisturized, cool baths or showers, wearing loose-fitting clothing made of breathable fabrics, topical creams or lotions (as advised by a physician). Medical attention is required if itching is severe or persistent or if it is accompanied by other symptoms (jaundice, dark urine, pale stools).
B. Stretch Marks (Striae Gravidarum):
- Causes: Rapid stretching and thinning of the skin due to weight gain during pregnancy. Genetic predisposition plays a role.
- Symptoms: Red or purple streaks on the abdomen, breasts, thighs, and buttocks. They eventually fade to silvery white.
- Management: Keeping the skin well-hydrated with lotions or creams may help minimize the appearance of stretch marks. There is no known cure.
C. Melasma (Chloasma):
- Causes: Hormonal changes during pregnancy stimulate increased melanin production, resulting in hyperpigmentation. Exposure to sunlight exacerbates the condition.
- Symptoms: Dark brown patches, usually on the face. Often seen on cheeks, forehead, and upper lip.
- Management: Sunscreen protection is crucial to prevent further darkening. Topical treatments may be recommended. The discoloration usually fades after delivery.
VI. Other Disorders:
A. Emotional Instability:
- Causes: The physiological changes, lifestyle adjustments, anxieties and fears associated with pregnancy can significantly impact emotional well-being. Hormonal shifts play a crucial role.
- Symptoms: Mood swings, irritability, anxiety, depression, tearfulness.
- Management: Support from family and friends, stress management techniques (yoga, meditation, etc.), prenatal yoga, counseling or therapy, if needed. Open communication with a healthcare provider is vital.
VII. Disorders Requiring Immediate Medical Attention:
The following symptoms warrant immediate medical attention as they could indicate serious complications:
- Vaginal Bleeding: Could indicate placenta previa, placental abruption, or other serious complications.
- Reduced Fetal Movements: May signify fetal distress.
- Severe or Persistent Headache (especially frontal or recurrent): Can be a sign of preeclampsia or eclampsia.
- Sudden Swelling or Edema (especially in face or hands): A possible symptom of preeclampsia.
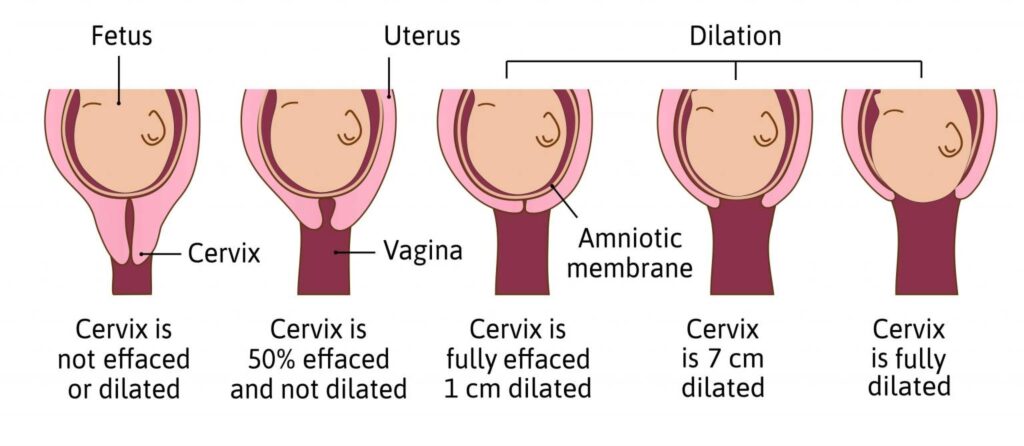
- Early Rupture of Membranes (PROM): Increased risk of infection and premature delivery.
- Premature Onset of Contractions: Risk of preterm labor.
- Maternal Exhaustion (to any extent): Can indicate underlying health issues.
- Fits or Seizures: Potentially indicative of eclampsia.
- Excessive Nausea and Vomiting (Hyperemesis Gravidarum): Severe dehydration and electrolyte imbalance.
- Epigastric Pain: Can be a symptom of preeclampsia.
MINOR DISORDERS OF PREGNANCY Read More »