DRESSINGS
Addressing is any protective cover for the wound. It is usually a cotton material.
Uses of dressings
- It helps to control bleeding.
- To prevent infections.
- To absorb any discharge.
- Prevents further injury to the wound.
Points to note:
- All dressings should be at least 2.5cm (inch) bigger than the wound.
- Dressings should, if possible be sterile so as not to put pathogenic micro-organisms onto the wound.
- Dressings should be absorbent so that sweat does not make the skin around the wound to get moistened or to absorb any discharge.
- Dressings should be airative to allow fresh air to the wound.
TYPES OF DRESSINGS
- Adhesive dressing (plasters): These are cloth materials which are embedded with gum or glue to assist in strapping onto the skin around the wound is dry and clean. Does not touch on to the wound with dirty hands after. Cleaning it or any part which is to be in direct contact with the wound.
- Sterile dressings: These are the best first aid dressing for large wounds. They are sealed in protective wrappers and should not be used if the wrapping has been torn or broken.
HOW TO USE STERILE DRESSINGS
- Remove both the outer and inner wrapping.
- Hold the folded dressing and its special bandage.
- Hold the bandage with the dressing over the wound and open out the folded dressing. Make sure you do not touch the wound inside which goes to the wound then place it on the wound.
- Wind the short piece of bandage once round the limb and then bandage firmly but gently with a long piece like a normal roller bandage.
3. Gauze dressings: these are used where you need a light covering e.g. gun shot. If there is no sterile dressing then you should use gauze dressing. It can be used together with pad of cotton wool. Secure it with a bandage or adhesive dressing. If there is no actual dressing available, then use any clean soft absorbent material which must be held in place firmly.
GENERAL RULES OF APPLYING DRESSINGS.
- If possible wash your hands thoroughly before applying dressing and thereafter.
- If the wound is not too large and bleeding is under control, clean it and surrounding skin before applying dressing.
- Avoid touching the wound or any part of the dressing which will be in contact with the wound.
- Never talk or cough over a wound or dressings.
- If necessary cover non adhesive dressings with cotton wool pads and bandage to control bleeding and absorb discharge.
- When cleaning the wound a swab soaked in antiseptic or disinfectant should be used once.
- If the dressing slips over a wound before you fix it in place, discard it and use a fresh one because the first one may have picked up germs from surrounding skin.
- Always place dressings directly onto the wound. Never slide it from the side.
BANDAGING
A bandaging is a piece of gauze or cloth material used for any of the purposes to support, hold or to immobilize any part of the body. Bandaging is a technique of application of specific roller bandages to different parts of the body.
PURPOSES OF BANDAGING
- To control bleeding
- To immobilize sprained or fractured limbs.
- To secure splints incase of fractures.
- To protect open wounds from contaminants.
- To provide support and aid in case of varicose veins or impaired circulation.
- To reduce swelling.
TYPES OF BANDAGING
There are three types of bandages;
- Triangular bandages.
- Roller bandages.
- Tubular bandages.
- TRIANGULAR BANDAGES
- They are made of cloth.
- They are usually used as slings
- They are used to secure dressings and immobilize injured limbs.
- When open, they can be used as scalp bandages.
Triangular bandages can be modified into;
- Broad fold bandage.
- Narrow fold bandages are used to immobilize the feet and ankles.
- They can also secure dressings on wounds (limbs)
- ROLLER BANDAGES
They are made of cotton gauze or linen. These are secured by pins, clips, tapes or tying knots
USES
- To secure dressing in position
- To apply pressure so as to control bleeding.
- To give support to sprain and strains in order to reduce pain.
THERE ARE THREE TYPES OF ROLLER BANDAGES
- CREPE BANDAGES
- These give firm support to injured joints.
- They give firm support to dressings applied over a wound.
- They provide good ventilation.
2. OPEN WEAVE BANDAGES
- They are used to hold light dressings in place
- They also allow ventilation because of their loose weave.
However they can not apply pressure on wounds or support to joints
3. COMFORTING BANDAGE
- These also secure dressings used to secure dressings on digits.
- They provide support to joints of digits
- Tubular bandage:
These bandages are rolls of seamless, tubular fabric. Elasticized bandages are used to support joints such as elbow or ankle. Tubular gauze bandage is used with a special applicator that is supplied with the bandage. It is suitable for holding dressings in a finger or toe, but not to control bleeding.
Method
- Cut a piece of tubular gauze about two-and-a-half times the length of the casualty’s injured finger. Push the all length of the tubular gauze on to the applicator, and then gently slide the applicator over the finger and dressing.
- Holding the end of the gauze on the finger, pull the applicator slightly beyond the finger tip, leaving a layer of gauze bandage on the finger. Twist the applicator twice to seal the bandage over the end of the finger.
- While still holding the gauze at the base of the finger, gently push the applicator back over the finger to apply a second layer of gauze. Once the gauze has been applied, remove the applicator from the finger.
- Secure the gauze at the base of the finger with adhesive tape that does not encircle the finger. Check the circulation to the finger then again every ten minutes. Ask the casualty if the finger feels cold or tingly. If necessary, remove the gauze and apply it more loosely.
CHARACTERISTICS OF AN IDEAL BANDAGE
- It should be elastic (but not too elastic).
- It should be well perforated to ensure adequate ventilation of the wound.
- It should be cotton made for easy absorption.
- It should be long enough to enable adequate support of the dressing or immobilization of the limbs.
- It should be non – adhesive in nature.
NOTE: Bandages are not for application on a wound but for application over a dressing on a wound.
GENERAL PRINCIPLES OF BANDAGING
- Use a tightly rolled bandage of suitable with and maintain one.
- Face the patient when bandaging an arm or leg except when bandaging the head.
- Hold the head of the bandage upper most
- Hold the bandage in the right hand when bandaging the left limb and vice versa.
- Bandage the limb from inside out wards and from bellow upwards keeping the even through out
- Begin the bandage with a secure turn and allow each turn to cover 2/3 of the proceeding one.
- Ensure that the bandage is neither too tight nor to lose.
- Finish off the bandage with a straight turn, fold in the end and secure a voiding joints and the site of injury.
- Fasten with safety pins or with the fasters provided with some bandages.
- A tape is always used in mentally handicapped or pediatric patients instead of pins or other sharp appliances.
GENERAL RULES OF BANDAGING
Before applying a bandage
- a) Keep reassuring and explain the procedure to the patient or casualty.
- b) Make the patient comfortably for example by lying or sitting him on the floor and the position should be convenient for the nurse or first aider.
- c) Keep the injured part well supported and elevated if necessary.
When applying a bandage
- a) Always stand in front of the casualty while bandaging except in scalp or head bandaging.
- b) If the casualty is lying down, pass bandages under the body’s natural hollows. For example the ankles, knees, neck etc.
- c) Apply bandages firmly enough to control any bleeding and hold dressings in place but not so tightly as to impair blood circulation.
- d) Leave fingers and toes on a bandage limb exposed to check for circulation
- e) Use reef knots to tie a bandage but do not tie on the injured part or over bony areas
When bandaging to immobilize a limb:
- a) Strictly pad between the limbs and the body or between the legs with cloth or folded cotton or towels
- b) Tie knots in front of the body and to the injured site or the middle of the body if the sites are injured.
After bandaging:
- a) Check the circulation of the injured part after every 10 minutes to ensure that blood flow is not impaired.
- b) Ask the casualty if there is any serious discomfort caused by bandaging.
NOTE: Always ensure infection prevention and control as much as possible.
SIGNS OF IMPAIRED CIRCULATION
- The extremities look pale, cold and later bluish appearance to the skin.
- Tingling and numbness of the part.
- Inability to move the affected limb.
- Swelling
HOW DO YOU CHECK FOR CIRCULATION.
Press one of the finger or toe nails or the skin on the foot or hand until its pale. Release the pressure. A pink color should return quickly if it remains pale, the bandage is too tight therefore loosen it by unrolling enough turns until the pink color is retuned and the warmth is felt.
BANDAGING TECHNIQUES/ PATTERNS USED IN BANDAGING
- CIRCULAR METHOD:
The bandage is applied in such a way that each turn encircles the previous one completely covering it. This technique is used to ankle bandaging or dressings.
- SPIRAL METHOD:
Each turn particularly overlaps the previous one. It is applied along straight body parts or parts with increasing circumferences. It can also be used to bandage the ear.
- SPIRAL REVERSE:
The bandaging is anchored and then applied in reverse direction half way through each spiral turn. This method is used to accommodate increasing circumferences of the body parts. Used for upper arm and upper leg.
- FIGURE OF EIGHT (8):
The bandage is anchored below the joint and then alternating in ascending and descending turns to form a figure of eight (8). This technique is used around joints.
- RECURRENT METHOD:
This technique includes a combination of recurrent and circular turns. Hold the bandage as you make each recurrent turn and then use circular turns as the final anchor. This technique is used for bandaging the scalp and a stump.
- TRIANGULAR BANDAGING:
Triangular bandage is used on the shoulder when it is injured and to give support to a fractured clavicle. It can be used as arm sling but in emergencies, the bandage can be used at all body parts.
a) ARM SLING
An arm sling holds the fore arm in a slightly raised or horizontal position. It provides support for injured upper arm, wrist or fore arm on a casualty whose elbow can be bent. Or: to immobilize the arm for a rib fracture.
PROCEDURE:
- Ensure that the injured arm is supported with the hand slightly higher than the elbow.
- Fold the base of the bandage under to form ahem (enclose).
- Place the bandage with the base parallel to the casualty’s body.
- Slide the upper end under the injured arm and pull it around the neck to the opposite shoulder.
- Fold the lower end of the bandage over the fore arm and bring it to meet the upper end at the shoulder.
- Tie a reef knot on the injured site at the hollow above the casualty’s collar bone and tuck both free ends of the bandaging under the knot to pad it.
- Hold the paint of bandage beyond the elbow and twist it until the fabric fits the elbow, then tuck it in. Alternatively, if you have a safety pin, fold the fabric and fasten it to the front.
- Check the circulation in the fingers as soon as you have finished. Re – check every 10 minutes.
b) ELEVATION SLING
This form of sling supports the fore arm and hand in raised position with the finger tips touching the casualty’s shoulders. It helps to control bleeding from wounds on the fore arm and also minimize swelling. It can also be used to support the arm in case of injured hand.
MANAGEMENT
- Ask the casualty to put his hand across his chest with the fingers resting on the opposite shoulder.
- Place the bandage over his body with one end over the shoulder on the injured side.
- Hold the point just beyond his elbow.
- Ask the casualty to extend off the injured arm from the chest while you took the bandage up diagonally across his back to meet the other end at his shoulder.
- Tie the ends to make a reef knot at the hollow above the casualty’s collar bone and took the ends under the knot pad it.
- Twist the point until the bandage fits closely around the casualty’s elbow. Tuck the point in just above his elbow and secure it.
- Check circulation, loosen and re – apply if necessary.
HAEMORRHAGE
This is loss of a blood from vessel. It can be internal or external. It can be mild or severe.
- Mild hemorrhage comes from injured capillaries. This bleeding flows in a stream.
- Severe hemorrhage comes from an artery or vein. And this blood tends to come with great force. This is because most large arteries transport blood at high pressure.
CLASSIFICATIONS:
It can be classified in 3 ways;
- Time of occurrence.
- Vessel injured (source)
- Site of the injury.
- CLASSIFICATION BY SITE
It can be external or internal.
External is visible or can be seen while internal means the bleeding is hidden or concealed. If bleeding is hidden in the abdomen, peritoneal, this is very dangerous because it’s hard to stop this kind of bleeding sometimes. It becomes visible, for instance if blood is in the lungs the casualty will cough it up, which is known as haemoptysis. In case bleeding is in the stomach, the patient or casualty vomits the blood, which is known as haematemesis.
The color of the vomits depends on the time; it also depends on the site which has been affected. It is dark red like coffee ground; it is an indication of a bleeding stomach ulcer.
People who have peptic ulcers as they progress they start bleeding such. Sometimes kidneys are injured or bladder and here blood is passed in urine which is called haematuria. In this case urine is smoky, blood stained.
Sometimes blood is passed on the stools, a condition known melaena. This makes the stools to be dark in appearance. This means the bleeding is from the upper intestine. Sometimes blood passed with the stools in fresh and bright red colored. It means bleeding is in the lower part of the bowel.
Bleeding from the vagina is normally due to miscarriage, menstruation or injury to those parts.
As a first aider always suspect internal bleeding after a severe injury or if the patient has signs of shock without obvious blood loss you must suspect that the patient may have sustained internal bleeding.
There are special sites of hemorrhage;
- Hemorrhage from the nose.
- Hemorrhage from the lungs
- Hemorrhage from the urinary bladder.
- b) Haemorrhage classification according to vessel (source)
- Arterial hemorrhage: Arteries are vessels which carry blood from heart to the rest of the body. This blood is fully oxygenated; it is bright red in color. Because it’s coming from the heart, it comes with pressure. It spurts out blood.
- Venous haemorrhage: This blood contains less oxygen and its color purplish red because it does not contain much oxygen.
- Capillary bleeding: Capillaries are the smallest vessels. In this case blood just oozes all over the wound. Its color is dark red and is the most common color.
c). Haemorrhage classification according to time.
- Primary haemorrhage: This occurs at the time of injury.
- Reactionary haemorrhage: This may occur any time within 24 hours of injury. It occurs due to recovery from shock which means the casualty is improving.
- Secondary haemorrhage: This occurs after 48 hours and is usually due to infection or sepsis.
CLOTTING MECHANISM
The human body has certain mechanisms which help to stop bleeding naturally.
When bleeding occurs, platelets collect together at the site of the injury and help to plug the wound, clotting factors are released, and there is a protein present in blood known as fibrinogen is converted to fibrin. The fibrin forms a mesh across the cut skin vessel. It traps the platelets and the blood cells from escaping. Then the mesh shrinks as serum oozes out leaving a solid clot which covers the wound.
GENERAL MANAGEMENT OF HAMORRHAGE
The aim of this management is to stop bleeding immediately and get medical aid as quick as possible.
- Put the patient in a suitable position. Preferably sitting or lying according to the type /site of injury.
- Elevate the bleeding part and support if not fractured.
- Expose the wound but removing small clothing as possible.
- Do not disturb any formed clot.
- Remove any foreign body which is visible and easy to remove.
- Apply and maintain pressure
- Apply a dressing or bandage.
- Immobilize the injured part.
- Transfer to hospital as soon as possible.
CONTROLLING HAEMORRHAGE
The principle of controlling blood loss is to restrict blood flow to the wound and encourage clotting. This is done in two ways that is by applying pressure and elevation of injured part.
DIRECT AND INDIRECT PRESSURE
- Direct pressure
- Direct pressure is put directly on the wound while indirect pressure is put on the vessel supplying blood to the wound.
- We always start with direct pressure
- In order to stop bleeding without interfering with the rest of the circulation by applying direct pressure on the wound.
- In case there is a foreign body or projecting bone, put the pressure around it and then maintain for 5 – 15 minutes.
- In case the wound is getting, cover the wound with a clean cloth.
- Put the casualty in a suitable comfortable position. If the bleeding continues, add on more clothing/ dressing/ padding without removing the first one.
- Secure the dressing with a bandage not firmly but able to cut off hemorrhage.
- Immobilize the injured part.
- Indirect pressure
- If bleeding cannot be controlled by direct pressure or if not possible, you apply indirect pressure at an appropriate pressure point between the heart and wound. For instance it can be used to control arterial bleeding within the limb.
- But as you compress this for a long time, then the limb will die off because of oxygen cut off.
The two pressure points for controlling severe bleeding are;
- Bronchial artery in the upper limb (arm).
- Femoral artery in lower limb.
INTERNAL BLEEDING
This may occur after an injury such as a fracture
- It could be a crash injury such as car injury.
- It can also occur due to a periodical condition
- It can also occur due to penetrating injury.
- The spleen can get ruptured.
- Internal bleeding is more severe/ dangerous than external bleeding.
- Much as this blood is not from the body but lost from circulation and hence not reaching vital organs.
- When this blood collects in different arteries, it may cause pressure on vital structures. For instance, if bleeding is within the skull and the person may become unconscious.
- If bleeding is inside the chest, it may prevent expansion of the lungs hence causing difficulty in breathing.
SIGNS AND SYMPTOMS
They vary according to the amount of hemorrhage and the rate of flow.
- There is always history of sufficient injury sometimes the history of the medical condition.
- There is pain and tenderness on the affected site and sometimes actual swelling.
- Patients may also have signs of shock. One of the signs of shock is pallor or paleness of the mucous membrane.
- The pulse rate is weak and rapid.
- Breathing also becomes shallow.
- The casualty becomes restless.
- If he/she is conscious, he/she will complain of the thirst.
- The temperature is below normal.
- Sometimes there is vomiting.
- Cold extremities.
- Blood may appear either from the mouth and eventually the patient may become un conscious
THE AIM OF TREATMENT
Is to arrange urgent remove to the hospital.
- Mean while lay the casualty down with the head lower than the rest of the body.
- Also ensure complete rest.
- Loosen any tight clothing around the neck, chest and waist for better circulation
- Re assure the patient to rest.
- Protect the patient from cold.
- Check for any other injury and manage accordingly.
- Carefully watch the breathing and pulse rate and record.
- Save and specimen be it of urine, vomitus for examination.
- If the casualty becomes unconscious, make sure the air way is clear and this is done by positioning the patient.
- Arrange transport to hospital as quickly as possible, quietly and knowledgeably.
- Do not give any thing by mouth because you are not sure if the patient is going to the theatre.
ARRESTING HAMMORRHAGE FROM SPECIALITIES
SCALP WOUND
- These usually occur due to accidents or falling down or during fighting. These wounds tend to bleed profusely.
- This is because of the reach blood supply and the skin on the scalp is straight.
- Sometimes these wounds are associated with a fracture.
SIGNS AND SYMPTOMS
- There is pain, tenderness and bleeding.
- There is swelling around the wound.
- There might be signs of fracture on the skull and that is bleeding from the nose.
- The casualty may become unconscious.
THE AIM OF TREATMENT
Is to control bleeding as soon as possible and transport to hospital for the director to rule out head injury.
- Control bleeding using direct pressure.
- Cover the wound with a sterile or clean piece of cloth and put a bandage to make sure bleeding stops.
- If the patient is unconscious, lay him down with the head slightly raised.
- Check breathing, check the pulse, level of response.
- If the casualty becomes unconscious, secure a clear air way by positioning.
- Arrange urgent removal to hospital as you maintain the treatment position
EPISTAXIS (NOSE BLEEDING)
It is a condition where there is bleeding from the blood vessels of the nostrils. It may be due to a blow, sneezing, it may be a sign of a fractured skull.
- Nose bleeding can cause considerable blood loss.
- The casualty may swallow the blood or inhale.
- If inhaled it is going to cause breathing problems.
- This patient presents with flow of blood.
In case there is a skull fracture, blood may be mixed with a clear, watery cerebral spinal fluid.
THE AIM OF TREATMENT
- Is to safe guard breathing by preventing inhalation of blood.
- Make the casualty to sit with the head slightly forward.
- Loosen any tightening around neck.
- Advise him to breathe through mouth.
- Pinch the soft part of his nose.
- Patient should not speak, swallow, and cough.
- Allow blood to come out (dribble) do not plug control wool.
- Casualty should not raise the head.
- Clean around the nose using lukewarm water with a soaked clean cloth.
- When bleeding goes beyond 30 minutes or stop and comes back then seek medical advice.
BLEEDING FROM THE MOUTH
Cuts in the mouth or on the tongue vary from mild to severe. They may be caused by the casualties’ teeth.
- It can also occur after tooth extraction
- Laceration can also occur and are quite often associated with the fracture of the jaw.
SIGNS AND SYMPTOMS
- Patients can complain of bleeding around or in the mouth.
- Pain at the bleeding area.
AIMS OF TREATMENT
To safe guard the airway by preventing the inhalation of the blood and to control bleeding.
WHAT TO DO
- Ask the patient to sit down with the head tilted slightly to the affected side.
- Place a clean dressing over the wound and tell the casualty to apply direct pressure on it.
- If it is a tooth socket, get a thick pad of gauze and place it across the socket and tell the casualty to bite on it.
- This pressure should be maintained for 10 – 20 minutes to allow any blood to dribble out from the mouth because if swallowed can cause vomiting.
- If bleeding persists after a period of 10 – 20 minutes carefully remove the pad without disturbing the clot that might have formed and replace with a new one and continue with pressure for more ten minutes.
- The casualty should not wash or rinse the mouth because it may disturb the clot.
- He should not take anything hot (drinks) for 12 hours.
- If bleeding persists or if it re- occurs, then refer for medical aid or dentist.
CAUSES OF HAEMORRHAGE
- Trauma/ injury
> It may be direct injury to the blood vessel involving neighboring tissues could be due to accident, surgical operation resulting into wounds.
> It may be indirect injury e.g. fractures of the skull may cause injuries to the vessels.
- Labour
> Ruptured fallopian tube incase of ectopic pregnancy.
> An obstetric is where the fetus separates from the placenta bringing out excess bleeding.
- Abnormalities in blood vessels for example.
- Neoplasm. These are new growth or tumors. They are actually concern cells which have the ability to destroy blood vessels
- Hemorrhoids. They are found in the digestive system (alimentary tract) especially at the rectum.
- Atheroma. Is the thickening of the walls of the arteries which bring about their rapture.
- Aneurysm. Arterial dilatation due to blood pressure on the weak tissues leading to their rapture.
- Diseases of blood for example hemophilia. Hemophilia is a blood coagulation disorder which is genetically determined and characterized by repeated hemorrhage. This could be nasal bleeding which is (epistaxis), rectal bleeding, hamaturia (blood in urine).
- Menstruation: Is a monthly loss (discharge) of blood through the birth canal of the females between 12 – 45 years.
- Diseases of intestinal tracts e.g. peptic ulcers, typhoid fever, dysentery, ulcerative colitis, may lead to loss of blood.
- Hypertension. Blood pressure refers to the force exerted on the walls of the blood vessels once the blood pressure is high than normal, then we talk of hypertension. And this can easily be due to cerebral vascular accidents.
GENERAL SIGNS AND SYMPTOMS OF HAEMORRHAGE.
- The face and lips are pale.
- Skin is cold and clammy.
- There is dizziness and fainting.
- The pulse is rapid and weak.
- Breathing is shallow and accompanied by yawning.
- Blood pressure is also decreased
- Temperature is low
- There is blurred vision.
- Casualty feels thirsty and will always ask for water.
- Low blood volume.
- Sighing and yawning.
- Oliguria – low output of urine.
- Casualty complaints of not feeling well and is anxious.
SIGNS AND SYMPTOMS OF INTERNAL HAMORRHAGE
Bleeding from orifices
SITE | APPEARANCE | CAUSE | |
1. | MOUTH |
|
|
2. | EAR |
|
|
3. | ANUS |
|
|
4. | NOSE |
|
|
5. | URETHRA |
|
|
6. | VAGINA |
|
|
NATURAL MECHANISM OF ARRESTING HAEMORRHAGE:
There are three ways through which bleeding can be arrested and these are:
- Constriction of blood vessel ( peripheral)
- Lowering of blood pressure.
- Clotting mechanism.
CLOTTING MECHANISM
In the clotting mechanism, the damaged platelets and tissues release a substance called thrombokinase (thromboplastin) which is an enzyme. This enzyme activates the prothrombin to the thrombin. The thrombin combines with fibrinogen to form fibrin. The fibrin forms a mesh to arrest the bleeding by trapping the blood cells to form a clot.
COMPLICATIONS OF HAMORRHAGE:
- Paralysis may occur due to damage or disturbance of the nerves.
- Hypovolaemic.
- Anaemia.
- Asphyxia.
- Hypothermia.
- Unconsciousness.
DIABETES MELLITUS
This is a condition which can lead for 2 types of coma.
- Diabetic coma (hyperglycemia).
- Insulin coma (hypoglycemia)
- HYPERGLYCAEMIA (DIABETIC COMA)
It occurs when there is excessive increase of glucose and a cetone.
SIGNS AND SYMPTOMS
Sometimes, he/she may be known diabetic.
- The onset is gradual – with headache, restlessness and the patient feels drowsy.
- Abdominal pain.
- Respirations are deep and sighing.
- The skin is dry.
- The breath smells acetone.
TREATMENT
- If the patient is unconscious, treat accordingly.
- If she/he is a known diabetic, the only treatment would be insulin which may not be available but if available measure it appropriately and give it.
- Quickly make arrangements and sent patient to hospital.
- Continue monitoring the vital signs.
- Reassure the patient always.
- HYPOGLYCAEMIA (INSULIN COMA)
Insulin is a drug used for treatment of diabetics. It occurs if a patient takes insulin without eating or eating late, or having done excessive exercises than planned.
SIGNS AND SYMPTOMS
- Sudden onset/ where the patient feels dizzy, fainting, irritability and confusion.
- Respirations are shallow
- Headache
- The skin is moist.
- The patient is sweating.
- The hands and legs are shaking or tremors
- He appears like drunkard.
- The breath has no particular smell.
- Eventually the patient becomes unconscious.
TREATMENT
- Check the patient’s pockets – checking for card indicating whether he/she is a diabetic.
- Check if he/she has a lamb of sugar.
- Check if the patient has marks of previous injections
- If it’s recognized early, give two spoonful of sugar in a juice or fruity drink.
- Once patient is not cooperative at first, but you have to act quickly.
- The sugar can be repeated after 10 minutes and this patient will begin coming up.
- Patient should be advised to always carry something sweet such that if he feels signs of hypoglycaemia he/she can take it.
- If the patient is unconscious, send the patient to hospital.
COMPLICATIONS OF DIABETES MELLITUS
- Neuropathy: no motor or sensory sensation.
- Erectile dysfunction and frigidity in women
- Cataracts
- Hypertension
- Retinopathy
- Diabetic foot
- Still birth, abortions, delivering big babies.
PREVENTIVE MEASURES
- Early identification/ screening for diabetes mellitus
- Adequate exercise to burn out excessive fats and glucose
- Avoid prolonged use of steroid therapy
- Excessive consumption of alcohol should be avoided
- Early detection and treatment of infections that can pause danger to the pancreas
FITS AND CONVULSIONS (SEIZURES)
A seizure consists of involuntary contraction of body muscles. It’s due to disturbance in the electrical activity of the brain. This convulsion result in loss or impairment of consciousness. The commonest cause is epilepsy. But there are also other causes including;
- Head injury
- Brain damaging diseases
- Shortage of oxygen or glucose
- Certain poison
There are two main types of epilepsy;
- Petitmal (minor)
- Grandmal (major)
- Petitmal epilepsy: is characterized by a short period of unconsciousness which may not be noticed. The person appears pale for a short time with a blank expression.
- Grandma epilepsy: Its described into type i.e. – idiopathic, Symptomatic
- Idiopathic has no evidence of a serious disease. The fit start in child hood and adolescence.
- Symptomatic represents with recognizable pathological condition which may be held to be directly responsible or indirectly responsible. They include anything that compresses the brain (tumor), head injury.
SIGNS AND SYMPTOMS
They occur in phases.
Phase1
- Aura ( warning stage)
- This stage, it precedes loss of consciousness
- The person experiences a funny feeling in the stomach, funny taste, in the mouth, a funny smell which is not real its brief.
- Tonic stage.
- There is sudden loss of consciousness.
- The person falls to the ground and may get injured.
- Muscles become rigid and back is arched very stiff.
- The teeth are clenched.
- Breathing becomes very difficulty, it may be noisy and it may stop temporarily.
- The patient may make a funny cry.
- The face is cyanosed and puffy.
- The neck veins are engorged.
- This lasts for around 30 seconds.
- CLONIC STAGE
- In this stage, muscles relax and then start contracting very rapidly.
- The whole body goes into those contractions.
- The tongue may be badly bitten.
- Frothing at the mouth.
- Patient may have incontinence of urine and faces.
- The convulsions and twitching gradually become less violent and eventually stop.
- This stage last for 1 minute.
- COMA STAGE
- When the twitching stops, the patient goes into coma and eventually sleeps.
- During this period, muscles relax.
- Color of face returns to normal.
- Breathing becomes normal and quiet.
- This lasts for 30 minutes.
- On waking up;
- The patient may have a slight/ brief of mental confusion.
- The patient may vomit.
- The patient may complain of headache
- And he/she may be disoriented
- He/she may act in a strange way. And this is called post epileptic automatism
MANAGEMENT
- During the tonic stage.
- Create space around the patient.
- Remove any dangerous item.
- Protect him from injury.
- Position the casualty by laying him down on the back with head turned to one side.
- Put a soft pillow under the neck.
- Place a well padded article; put it between the teeth if possible. This helps to prevent biting the tongue. Do not force the article.
- Loosen any tight clothing around the neck.
- Note the time and duration of falling.
- During clonic stage.
- Don’t restrain the patient.
- Watch and prevent him from injury.
- Try to support and protect the head by providing a pillow until the fit is over.
- During coma stage
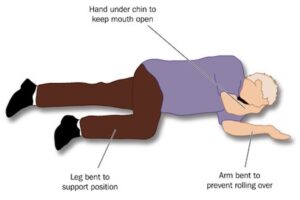
- Make the patient comfortable by putting in recovery position.
- Don’t wake the patient if sleeping
- Allow consciousness to return gradually.
- Let the patient quit after consciousness has turned.
- Give appropriate advice.
- OBSERVATION
- Observe the parts of the body which have been affected.
- Duration and frequency of the fits.
- Note presence of incontinence.
- Vital signs.
All these must be recorded and reported to the doctor.
CONVULSIONS IN CHILDREN
Convulsions commonly occur in young children, they are sometimes referred to as infantile convulsions. The symptoms are similar to those of epileptic fits but in children are more severe. They often occur as a result of high temperature; as it’s associated with infection of the throat, ear.
MANAGEMENT
- The child should be placed in bed and a pillow or something soft placed around the child so that the violent movements do not cause injury.
- Do not restrain the child when is convulsing
- Cool the child by removing extra clothing, ensure fresh air supply but do not expose to extreme coldness.
- Once the convulsions stop, maintain a clear air way by placing the child in recovery/ prone position
- Re – assure the parent of the child.
- Monitor the vital observation.
- Arrange transfer to hospital.
COMPLICATIONS OF EPILEPSY
- Status epileptic us
- Brain damage due to prolonged anoxia (lack of oxygen to the brain)
- Burns due to falling into fire
- Suicide as a result of stigmatization
- Unprovoked episodes of violence, anger
- Memory disturbance
- Isolation
- Lack of employment
- Sexual exploitation
- Low self-esteem
- Fear
- Depression
- Contractures- fibrosis causing permanent contractions.
- Psychotic behaviors e.g. hallucinations, delusions.
- Committing crimes in the state of post ictal phase
UNCONSCIOUSNESS (INSENSIBILITY)
Consciousness: is the state of awareness or alertness
It is due to interruption of the brain due to some interference with the nervous system. It’s an indication of injury or disease onto the brain but it can also be to other body parts. It’s a stage of unawareness.
LEVELS OR STAGES OF UNCONSCIOUSNESS STATE
- One can be fully awake or fully conscious.
- Disoriented but able to answer simple question.
- When the person is not able to answer questions but can obey orders.
- The person does not respond to any words but can respond to painful stimuli.
- Completely unresponsive.
TERMS USED TO DESCRIBE UNCONSCIOUSNESS
- Stupor (partial unconsciousness)
- Coma (stage of complete unconsciousness)
The degree of unconsciousness may be determined by the following.
- Speaking to the casualty.
- In the stupor state, the patient can be roused with difficulty in response. But in coma, there is no response at all.
- In stupor, the pt objects touching his/her eye lids and in coma, there’s no response at all.
- Reaction to light, in stupor, pupils of the eye react to light i.e. the pupils become smaller and in deam light or darkness to pupils becomes dilated. While in coma, there’s no reaction to light.
CAUSES OF UNCONSCIOUSNESS
- Shock
- Asphyxia
- Poisoning
- Head injury especially when associated with brain injury causing a condition known as concussion or compression.
- Epilepsy
- Hysteria
- Infantile convulsions
- Excessive heat
- Diabetes
- Fainting can also lead to unconsciousness.
- Heart attack
- Electric shock
- Brain attack
- Eclampsia
- Cerebral vascular accident (CVA) (Sroke)
SIGNS AND SYMPTOMS OF UNCONSCIOUSNESS
- Shallow breathing
- Face turns pale
- Skin cold and clammy
- Pulse is rapid and weak
- Dilated pupils and unequal
- No reflexes
- Restless in case of head injury
- Nausea and vomiting on recovery
- Loss of memory of event before and after accidents
FIRST AID MANAGEMENT OF UNCONSCIOUSNESS
- Remove the casualty from danger
- Ensure plenty of fresh air and if the casualty is near smoky area remove him or her from that place.
- Ensure an adequate supply of fresh air and check on the following:
- Look for any signs of injury like wounds, bleeding from any side of the body.
- Check the pulse rate.
- Respirations; check respiratory rate, chest movements and any noise.
- Check the skin, is it cyanosed, sweating, cold, dry, pale
- The pupils of the eye; are they dilated, constricted equal or unequal.
- Smell of the breath, could it be alcohol, disinfectant, acetone.
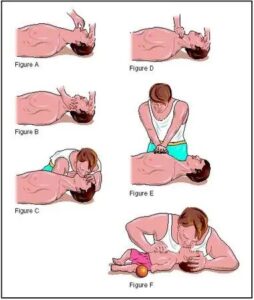
- Give artificial respiration or resuscitation.
- If there is any bleeding, control it, dress wound and immobilize fracture.
- Position the casualty in semi-prone (recovery) position with the head slightly lower than the level of legs.
- Establish the level of unconsciousness and record any changes in reaction to pupil.
- Reassure the casualty after gaining consciousness.
- Moisten her / his lips but nothing by mouth.
- If the casualty is restless, prevent him from hurting himself.
- Transport the casualty to the hospital.
- Reaching the hospital handover the casualty to in charge and report.
GENERAL RX
- Position the casualty appropriately.
- Ensure a clear airway.
- Remove dentures.
- Remove tight clothing around the neck, chest etc
- Keep away crowds.
- Give nothing by mouth.
- Keep the patient warm but do not over heat.
- If breathing has stopped, position the patient and start CPR (cardio pulmonary resuscitation).
- If breathing is quiet, lay the patient on the back with the head turned to one side.
- Elevate the lower part to encourage drainage of secretion from the lungs.
- Treat the cause of the unconsciousness.
- Remain with the casualty until she is handed over to a responsible person.
- Continuously watch carefully for any change in the casualty condition.
- Move the casualty to shelter.
- When the casualty gains consciousness, moisten the lips
- If there is no suspected to abdominal injury, sips of water can be given to drink.
COMPLICATIONS OF UNCONSCOUSNESS
- Respiratory tract infections: person may develop aspirated pneumonia due to mucus secretions
- Respiratory tract obstruction: the tongue may fall backwards and obstruct the airway
- Heart failure may result especially if the causes of the unconsciousness was cardiac arrest
- Renal or kidney failure may develop
- Damage to the brain cells due to lack of oxygen to the brain.
DIRECT INJURY TO THE BRAIN
- CONCUSSION
This is shaking of the brain. It occurs when there is wide spread disturbance of the brain as a result of injury to the head and sometimes the spine. It may be caused by a blow on the head or falling. It may not be associated with any change in the brain substance.
SIGNS ANND SYMPTOMS
- Brief period of impaired consciousness.
- Patient may have temporally confusion.
- There is dizziness, nausea and vomiting.
- Temporary loss of memory.
- Mild generalized headache.
TREATMENT
- Manage as unconscious patient.
- Monitor vital signs.
- Even after recovery, continue monitoring these patients for possible deterioration in the level of consciousness.
- Advice him to go to hospital if he/she develops any of the following.
- Headache
- Confusion
- Vomiting
- A patient who has been unconscious even for 1 minute or less shouldn’t be allowed to do anything before she/he has been checked by the doctor
- CEREBRAL COMPRESSION
This is a condition due to pressure on same part of the brain with the skull. It may be a blood clot, apiece of a bone in case of skull fracture it may be a tumor. Cerebral compression may lead to unconsciousness when is irreversible. Compression is a very serious condition. As so serious with in most cases it requires surgery.
SIGNS AND SYMPTOMS
- In the early stages, pt is irritable.
- He may have twitching of the limbs.
- Shouting.
- May get convulsion.
- When a patient is having an attack of convulsion, he should not be restrained, just protect him from getting injured.
- With unconsciousness, coma may be present.
- Breathing is noisy.
- Face is flushed.
- The pulse is slow but strong.
- Temperature may be raised.
- The pupils of the eye may be unequal in size or they may be dilated.
- The patient may get paralysis.
- The patient usually complains of severe headache.
TREATMENT
Apply the general rules of unconsciousness send the patient for medical treatment.
FOREIGN BODIES
A foreign body is an object that enters the body through different areas. It can enter through around in the skin like penetrating objects. It can enter through one of the natural openings of the body i.e. through mouth, nose, ears eyes, etc.
A penetrating foreign body can be only thing from a big or tiny object. It can be loose, whereby it can be removed without causing pain or injury. But sometimes it’s deeply embedded in which can lead it act as a plug to prevent blood loss.
A large embedded object may produce a deep wound. But a small one will cause minor lacerations.
The problem with penetrating foreign objects is that in most cases there not clean and if not clean there’s a risk of infection.
SPLINTERS
- These are small pieces of wood, glass, metal which may enter the skin.
- They are the commonest type of foreign bodies
- They can successfully be removed without any problem.
- If it is deep and difficult to remove, don’t interfere refer the patient to hospital.
TREATMENT
- Gently clean the area with soap and Ho2
- Get the pair of tweezers which should be sterile or as clean as possible and dry to handle of the object and pull it out.
- After pulling it out, squeeze around the wound such that same little fluid comes out.
- As it comes out, it may washout some of the remaining pieces remaining.
- Clean and cover the wound with a clean dressing. If the splinter does not come out easily, treat, it as an embedded body and refer the patient to hospital.
FOREIGN BODY IN THE EYE.
- Dust, grit (sand, small piece of stone), insects etc. can get into the eye
- These cause discomfort and if not removed quickly, they can cause serious trouble.
- You must not attempt to remove anything that sticks to the eyeball.
- Make sure you send the casualty to hospital quickly.
TREATMENT
- Make the patient sit.
- Gently separate the eye leads.
- Examine every part of the eye.
- You can ask the patient to blink the eyes rapidly. This may dislodge the foreign body
- If the foreign body is visible and loose, pour water from the inner corner such that it can drain up.
- Alternatively you can flood the eye in water
- If you think it is in the upper lid, try to pull it outwards and push it over the lower lid, this could also help to dislodge it.
- You can also use a corner of a handkerchief to remove it out.
- If all this fail, apply an antibiotic eye ointment, cover the eye and refer to hospital.
FOREIGN BODY IN THE EAR
- Children often push things like beans, tablets, etc into the ear.
- Insects can also enter the ear.
- When a foreign body gets lodged in the ear, it may cause temporally deafness by blocking the ear canal.
- It may also damage the ear drum.
TREATMENT
- If you’re sure that it’s an insect in the ear, floats and comes out with the fluid as you turn.
- For other foreign objects, just refer the patient to hospital as soon as possible.
FOREIGN BODY IN THE NOSE
Again children may push small objects in their noses. They can block the nose that can cause infection. If it’s sharp, it can cause damage to tissues in the nose and it can cause a sore.
TREATMENT OR MANAGEMENT
- Take quick history
- Calm down the patient by reassuring him/her.
- Examine the nose to see how deep the foreign body is.
- If it’s not very far, try to touch in the unaffected nostril which may induce the casualty to sneeze.
- If this fails, block the ears and try to tell the casualty to blow very hard. This may help to dislodge the foreign body.
- If all these fails, refer, meanwhile tell him to breathe through the mouth.
- Make sure, there is no disturbance with the nostril.
- If it’s a child, you tie the hands/ arms.