Table of Contents
ToggleNormal Third Stage of Labour
The third stage of labor is a critical phase that involves the separation, descent, and expulsion of the placenta and membranes, as well as the prevention of hemorrhage.
Physiology of the Third Stage of Labour:
- Contraction and Retraction:
- The placental separation is initiated by the contraction and retraction of the uterine muscles. These contractions thicken the uterine wall, reducing the capacity of the upper uterine segment and decreasing the area of the placental site.
- Separation starts from the center of the placenta. As the blood sinuses tear, a retroplacental clot forms, aiding in further placental separation.
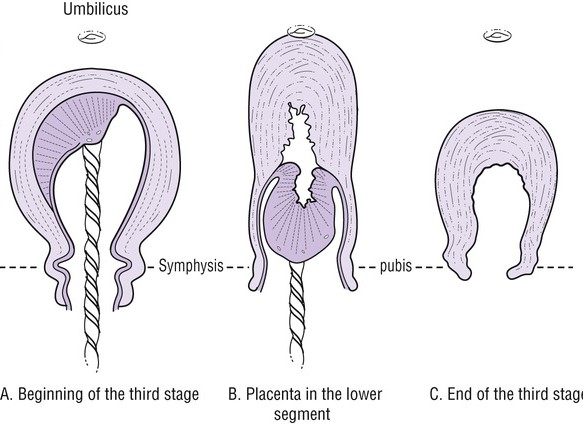
- Descent of the Placenta:
- The placenta descends due to the force of gravity acting like a piston on the clot. This propels the placenta from the upper uterine segment into the lower uterine segment.
- Separation of Membranes:
- The membranes become separated as the weight of the placenta peels them off the decidua. However, the membranes may remain adherent around the cervix until the placenta is expelled from the vagina.
- Haemostasis (Preventing Hemorrhage):
- At placental separation, swift control of blood flow is crucial to prevent serious hemorrhage. Several physiological processes play a role in achieving haemostasis:
a. Retraction of oblique uterine muscle fibers leads to the thickening of the uterine muscles, acting as a clamp and securing a ligature action on the torn vessels.
b. Vigorous uterine action after separation brings the uterine walls into opposition, exerting further pressure on the placental site.
c. A fibrin mesh rapidly covers the placental site after separation, utilizing 5-10% of the circulating fibrinogen to aid in clot formation and control bleeding.
d. Breastfeeding stimulates the release of oxytocin, which enhances uterine contractions, contributing to haemostasis.
Separation of the Placenta:
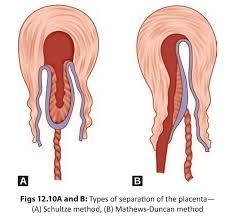
The separation of the placenta during the third stage of labor can occur in two ways, known as the Schultze method and the Mathew Dancan method.
- Separation usually starts centrally, resulting in the formation of a retroplacental clot. This clot exerts pressure at the midpoint of the placental attachment, aiding in the separation process and helping to strip the placenta’s adherent lateral borders.
- The increased weight of the placenta also assists in peeling the membranes off the uterine wall, creating a membranous bag enclosing the clot. As the placenta descends, the fetal surface comes out first.
- This method is associated with more complete shearing of both the placenta and membranes, leading to less fluid blood loss. It is a quick and clean method.
- Placental separation begins from the sides, and blood escapes from the sides during the process, without the assistance of a retroplacental clot.
- The placenta descends slipping sideways, with the maternal surface coming out first.
- This method takes longer and is associated with ragged and incomplete expulsion of membranes, leading to a higher fluid blood loss.
After separation, the uterus contracts strongly, forcing the placenta and membranes to fall into the lower uterine segment and eventually into the vagina.
Signs of Placenta Separation:
- The uterus becomes hard, round, and mobile.
- The fundus rises to or above the umbilicus.
- The cord lengthens or elongates.
- There may be a gush of blood.
- The placenta can be felt on vaginal examination (VE).
- Presence of the placenta at the vulva.
- If suprapubic pressure is applied, the cord does not recede into the vagina.
Mechanism of Placental Separation:
- Placental separation is facilitated by a combination of uterine contractions and involution.
- After the delivery of the fetus, the uterus continues to contract approximately every 3-4 minutes. These contractions, along with the process of involution (the shrinkage of the uterus), lead to the site of implantation of the placenta undergoing shrinkage as well.
- Within 10-15 minutes after the baby’s delivery, most of the placenta detaches from the uterine wall. This results in an increase in vaginal bleeding from the exposed implantation site, which signals the impending delivery of the placenta.
- As the placenta is delivered, the uterus continues to contract, closing the spiral arterioles and reducing bleeding. The ongoing contraction of the uterus helps in preventing excessive blood loss.
N.B: It is important to note that the average blood loss from a vaginal delivery is approximately 250-300mls.
Management of the Third Stage of Labour:
Methods of Delivering the Placenta:
- Controlled cord traction. (active)
- Maternal efforts(passive management).
Active Management (Controlled Cord Traction):
- Palpate the abdomen to exclude undiagnosed twin pregnancies.
- Administer oxytocin 10 IU intramuscularly to enhance uterine contractions.
- Extend the cord clamp slightly to the vulva to get a good grip. Place the left hand over the fundus of the uterus.
- During the first contraction, turn the palm of the left hand facing the fundus and apply counter traction above the pubic bone.
- The right hand grasps the cord clamp and applies steady downward and outward traction until the placenta is visible at the vulva, then applies upward traction to receive the placenta in a cupped hand.
- Take care to roll the membranes to prevent them from breaking.
- Deliver the membranes in upward and downward movements.
- Note the time of placenta and membranes delivery.
- Rub the fundus to promote further uterine contractions.
- Quickly examine the placenta for completeness and place it in a receiver.
- Clean the vulva to remove any blood, and examine the cervix and vagina for lacerations or an extension of an episiotomy.
- Repair any lacerations or tears.
- Place a clean pad and ensure the mother is comfortable.
Passive Management (Maternal Efforts):
- This method is only used when the placenta has already separated from the uterine wall.
- Wait for signs of placental separation.
- Once the placenta has separated, ask the mother to push during contractions.
- Place a flat palm over the mother’s abdomen to provide resistance for her to push against.
- Receive the placenta in both hands and deliver it complete.
- Administer oxytocin 10 IU intramuscularly.
Note: It is essential to keep the mother warm as she has undergone strenuous physical exercise during the first and second stages of labor, leading to significant heat loss from her body.

AM SO HAPPY THIS WAS HELPFUL THANKS ONCE AGAIN