Table of Contents
ToggleEPISIOTOMY
An episiotomy is a surgical procedure that involves making an incision on the perineum to widen the vaginal opening before childbirth.
Indications for Episiotomy:
To qicken delivery in the following situations:
a. Pre-eclampsia and eclampsia.
b. Cardiac diseases, to reduce strain on the mother.
c. Maternal distress, to minimize strain during delivery.
d. Fetal distress, aiming to prevent fetal death.
e. Cord prolapse in the second stage of labor, while the baby is still alive.
To prevent excessive trauma in the following cases:
a. Rigid perineum.
b. Forceps delivery.
c. Face to pubis delivery.
To reduce the risk of cerebral damage in the following circumstances:
a. Premature births.
b. Postmaturity.
c. After the baby’s head emerges in breech deliveries.
d. In cases of a narrow subpubic arch.
e. After previous third-degree tears.
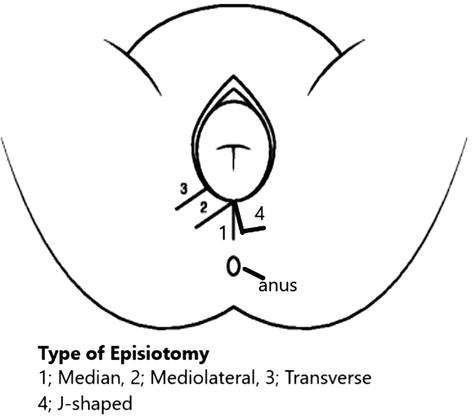
TYPES OF EPISIOTOMY:
Lateral Incision:
- This incision is made laterally across the labia majora and can be challenging to repair.
Disadvantages:
- May lead to excessive bleeding.
- Risk of damaging the Bartholin’s glands.
- Causes discomfort to the mother.
- Takes longer to heal.
Medial Lateral:
- This is the most common and recommended type, particularly for midwives.
- The incision starts from the fourchette and extends in the medial lateral direction of the perineum, typically 2-3cm.
Advantages:
- Usually heals well.
- Easier for a midwife to perform and repair.
- Minimizes damage to blood vessels.
- Reduces the risk of excessive perineal tear.
- Shortens the duration of the second stage of labor.
- Helps avoid injuries to the Bartholin’s glands and the anal sphincter.
Medial or Central or Midline:
- This incision begins at the center of the fourchette and proceeds in the midline towards the anus.
Advantages:
- Results in less bleeding.
- Provides greater comfort to the mother.
- Simple to perform and easy to repair.
Disadvantages:
- May extend to involve the anal sphincter.
- Poor repair could lead to Rectovaginal fistula (RVF).
J-shaped:
- Performed by a doctor, this incision starts from the center of the fourchette and curves away from the anal sphincter at a distance of 2.5cm.
Bilateral:
- Similar to the lateral incision but done on both sides.
- It starts from the fourchette to the lateral wall.
Note: Bilateral episiotomy is discouraged due to the potential risk of injury to the Bartholin’s glands.
Precautions when giving episiotomy:
Timing: Avoid performing the episiotomy too early or too late during labor.
Presentation: In cephalic presentation, the head should be stretching the perineum, and in breech presentation, the anterior shoulder should be stretching the perineum before performing the episiotomy.
Contraction Height: Give the episiotomy during a contraction to ensure better control and precision.
Basic principles prior to repairing the perineum:
Timely Repair: Perform the repair as soon as possible to minimize the risk of bleeding and perineal edema.
Aseptic Technique: Ensure that the repair is done using proper aseptic techniques to reduce the risk of infection.
Equipment Check: Verify that all necessary equipment is in place and count swabs and needles before and after the procedure to avoid leaving any foreign objects inside.
Anesthesia: Make sure the wound is adequately anesthetized before starting the repair to minimize discomfort to the patient.
Basic principles after repair:
Hemostasis: Ensure complete hemostasis to prevent excessive bleeding.
Post-repair Examination: Perform rectal and vaginal examinations to confirm the adequacy of the repair, ensuring no other tears have been missed, and verify that rectal mucosa has not been inadvertently repaired.
Removal of Swabs: Double-check to ensure that all tampons or swabs used during the procedure have been removed.
Detailed Documentation: Make detailed notes of the findings and the repair procedure for accurate medical records.
Post-repair Care: Inform the woman about the use of appropriate analgesia (pain relief), hygiene practices, maintaining a good diet, and performing pelvic floor exercises to aid in recovery.
Method of Infiltration and Method of Performing:
Requirements:
- A sterile episiotomy pack containing:
- Pair of episiotomy scissors.
- Needle and cut gut.
- Needle holder.
- Sterile gauze and cotton swabs.
- Sterile gloves.
- Syringe.
- Lignocaine.
- Hibicet.
Method of Infiltration:
- Ensure the procedure is performed under sterile conditions.
- Explain the procedure to the mother to keep her informed.
- Draw the required amount of lignocaine or local anesthesia (10mls of 0.5% and 5-7mls of 1%).
- Swab the vulva to maintain cleanliness.
- During a contraction, when the head or presenting part is distending the vulva, place two fingers of the left hand between the fetal head and the perineum to ensure that the drug is injected into the fetal scalp to avoid potential harm to the baby.
- Introduce the needle into the perineum and withdraw the piston to check for any blood aspiration. If blood is aspirated, reposition the needle and repeat the procedure until no blood is withdrawn.
- Insert two fingers into the vagina and position the blades at the peak of a contraction. Make a single clean cut approximately 3cm in length in a medial lateral direction.
- Control hemorrhage by pressing a sterile swab on the area.
Repair Technique:
Before the midwife starts to repair the episiotomy:
Ensure the proper setting:
- Place the mother comfortably.
- Remove any soiled linen from under the genitalia.
- Adjust the light source to have a clear view inside the vagina.
Communicate with the mother, explain the repair procedure, and provide reassurance.
Put on fresh sterile gloves.
Check whether the previously administered local anesthesia is still effective. If the mother feels pain, administer more anesthesia before the repair.
Remove all clots from the birth canal.
Assess the extent of damage to the vagina and locate the apex of the episiotomy.
Insert a roll of vaginal pack and secure the end with artery forceps.
Start suturing the episiotomy from the apex.
Suture the vaginal mucosa using the continuous stitch technique. Pass the needle through the vaginal mucosa from behind and bring it out on the perineum wound.
Continue using the continuous suturing method all the way to the bottom of the wound to close the deep muscle layer. The same technique can be used on the skin.
Remove the vaginal pack, inspect the vagina, and insert a finger in the rectum to ensure closure and exclude involvement of the rectum.
Clean the mother after completing the repair.
Provide a pad for the mother’s comfort.
Advise the mother on caring for the episiotomy and provide necessary instructions.
Clear away and properly dispose of used materials.
Note: The typical healing time for an episiotomy is around 4-6 weeks, depending on the size of the incision and the type of suture material used to close the wound.
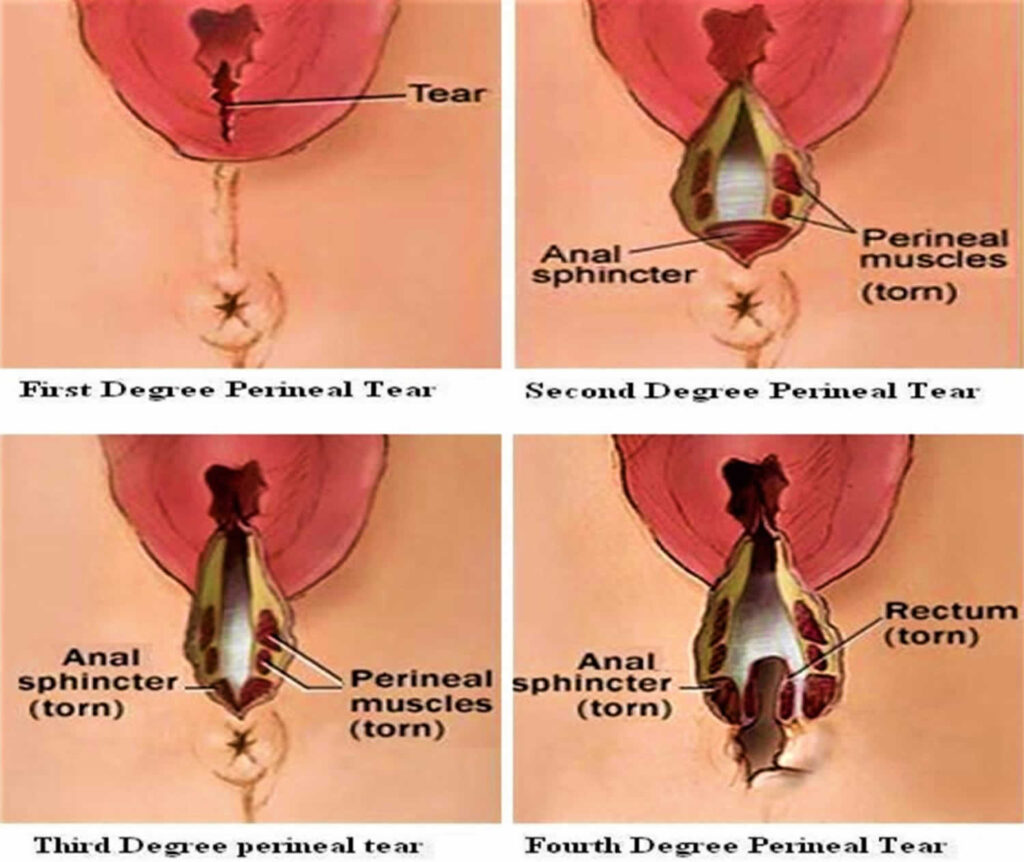
Classification of Perineal Trauma:
First Degree Tear:
- Injury to the perineal skin only.
Second Degree Tear:
- Injury to the perineum involving perineal muscles but not the anal sphincter.
Third Degree Tear:
- Injury to the perineum involving the anal sphincter.
Fourth Degree Tear:
- Injury to the perineum involving the anal sphincter complex and anal epithelium.
Isolated Buttonhole Injury of the Rectum:
- Injury to the rectal mucosa without injury to the anal sphincters.
Complications of Perineal Trauma:
- May become a 3rd degree tear.
- Bleeding.
- Infections.
- Swelling.
- Defect in wound closure.
- Local pain and a short-term possibility of sexual dysfunction.

I got the best understanding of episiotomy procedure ever
Thank you so much, this has been helpful to me and other colleagues
wonderful
👍👌
This should continue always