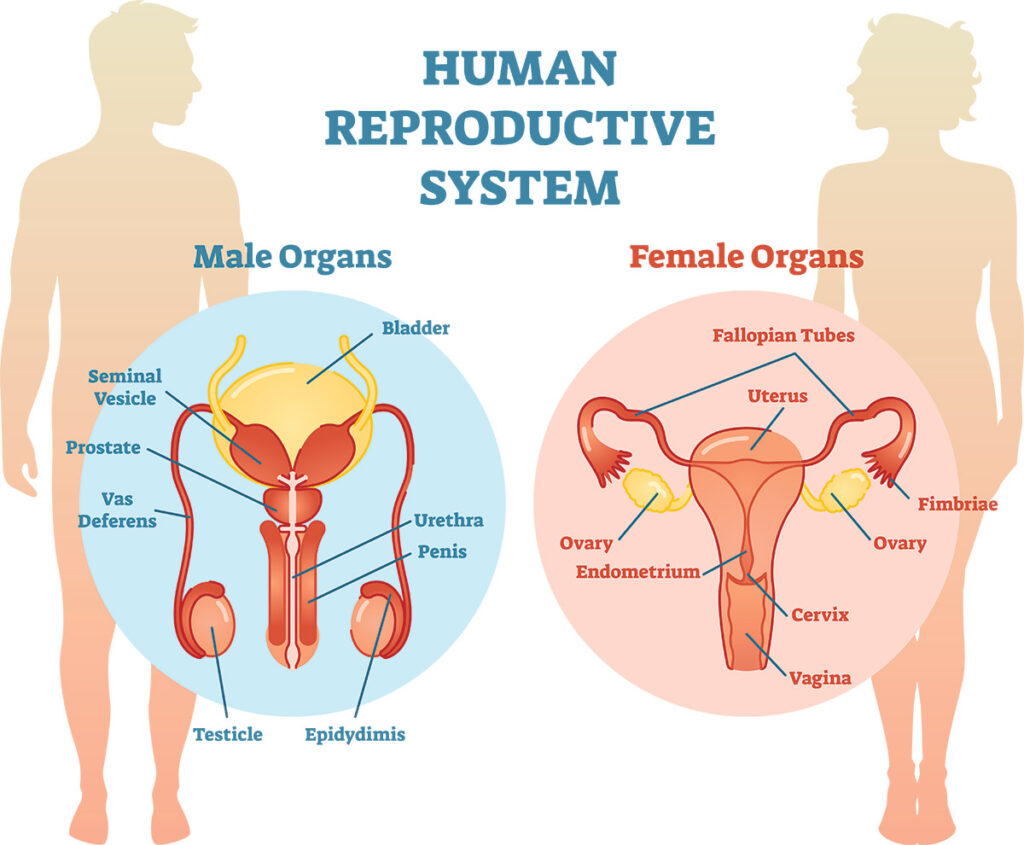
Reproductive System
Reproductive system, also known as the genital system or the reproductive system, is a collection of organs and structures in the human body responsible for sexual reproduction.
Its primary function is to produce, store, and deliver gametes (reproductive cells) and facilitate the union of sperm and egg for the purpose of fertilization, leading to the creation of new life.
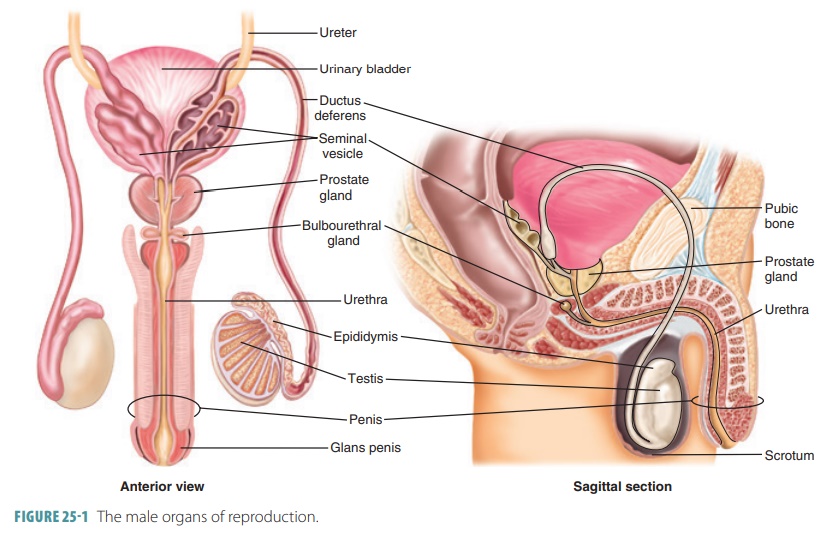
The Male Reproductive System
External genital organs
External male reproductive organs are those outside and can be seen. They comprise of the;
- Scrotum.
- Testis.
- Penis.
The penis
It is an organ that carries the semen with the sperm into the vagina. During sexual arousal, blood is pumped into the muscles of the penis making it stiff/erect so it can easily enter the vagina. The penis additionally serves as the urethral duct. Although both semen and urine pass through the urethra in the penis, at the time of ejaculation the opening from the bladder is closed so that only semen comes out of the penis. After ejaculation, the blood quickly drains away into the body and the penis returns to the normal state.
∙ The penis is enclosed by a foreskin (prepuce) that protects the glans penis. Usually the penis produces a white creamy substance called smegma, which helps the foreskin to slide back smoothly. When smegma accumulates under the foreskin, it causes a bad smell or even infection. Therefore for men who are uncircumcised need to pull back the foreskin and gently wash underneath it with clean water everyday
The scrotum
It is a sac of skin containing two egg-shaped organs called the testes, found in front of and between the thighs. It protects the testes from physical damage and helps to regulate the temperature of the sperm.
The testes
They are two sex glands that produce sperm and the male hormones, which are responsible for the development of secondary sexual characteristics in men.
The male internal reproductive organs
- Epididymis.
- Deferent ducts (vas deferens).
- Seminal vesicles.
- Ejaculatory ducts.
- Prostate gland
- Urethra-bulbous glands.(bulbourethral glands)
Vas deferens
- Prostate gland.
- Urethra-bulbous glands.(bulbourethral glands)
They are tubes through which the sperm passes from the testicles and penis.
Epididymis
- They are cord-like structures coiled on top of the testes, it stores sperm.
- When sperm matures, it is allowed to pass into the vas deferens before being released during ejaculation.
Seminal vesicles
- They are glands where the white fluid, semen is produced.
- Semen is fluid that is released through the penis during ejaculation.
- It provides nourishment for the sperms and helps their movement.
- The seminal vesicles do not store sperm cells.
- They secrete a thick alkaline fluid that mixes with the sperm cells as they pass into the ejaculatory ducts and then the urethra.
- These secretions provide most of the volume of the semen.
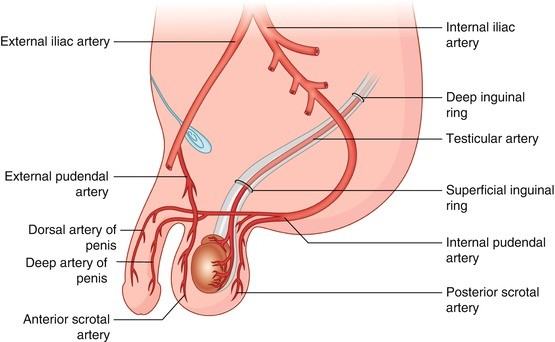
Arterial supply, venous drainage and nervous supply
- The arteries are derived from the inferior vesical and middle rectal arteries.
- The veins accompany the arteries.
- Nervous supply is by sympathetic and parasympathetic nerve fibers.
Prostate gland
- This is the largest accessory gland of the male reproductive system.
- It is situated below the bladder.
- The prostate is partly glandular and partly fibromuscular.
- The prostate produces fluid that makes up part of the semen; it helps create a good environment for the sperm in the penile urethra and vagina
- Enables movement of sperm and provides nutrients for the sperm.
Cowper’s gland
- It comprises two small glands situated below the prostate with ducts opening into the urethra.
- Its function is to produce some fluids, which helps create a good environment for the sperm in the penile.
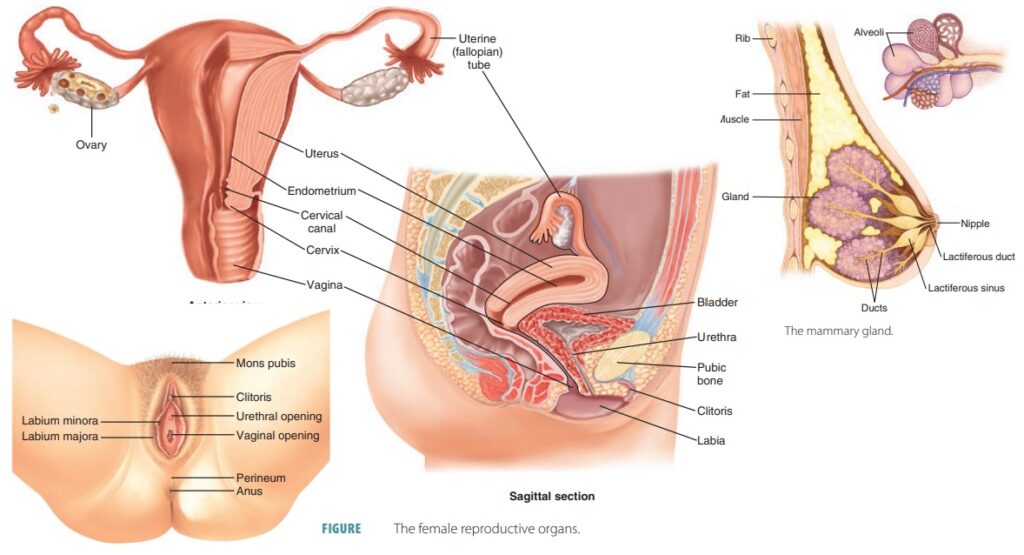
The Female Reproductive System
The female external genital organs
- The Mons Pubis
- The Labia Majora
- The labia minora.
- The vestibule of the vagina.
- The External Urethral Orifice
- The Vaginal Orifice
- The Greater Vestibular Glands
- The Lesser Vestibular Glands
- The Clitoris
- The Bulbs of the Vestibule
The mons pubis
- The mons pubis is a rounded fatty elevation located anterior to the pubic symphysis and lower pubic region.
- It consists mainly of a pad of fatty connective tissue deep to the skin.
- The amount of fat increases during puberty and decreases after menopause.
- The mons pubis becomes covered with coarse pubic hairs during puberty, which also decrease after menopause.
- The typical female distribution of pubic hair has a horizontal superior limit across the pubic region.
The labia majora
- The labia are two symmetrical folds of skin, which provide protection for the urethral and vaginal orifices.
- These open into the vestibule of the vagina.
- Each labium majus, largely filled with subcutaneous fat, passes posteriorly from the mons pubis to about 2.5 cm from the anus.
- They are situated on each side of the pudendal cleft, which is the slit between the labia majora into which the vestibule of the vagina opens.
- The labia majora meet anteriorly at the anterior labial commissure.
- They do not join posteriorly but a transverse bridge of skin called the posterior labial commissure passes between them.
The labia minora
- The labia minora are thin, delicate folds of fat-free hairless skin.
- They are located between the labia majora.
- The labia minora contains a core of spongy tissue with many small blood vessels but no fat.
- The internal surface of each labium minus consists of thin skin and has the typical pink color of a mucous membrane.
- It contains many sensory nerve endings.
- Sebaceous and sweat glands open on both of their surfaces.
- The labia minora enclose the vestibule of the vagina and lie on each side of the orifices of the urethra and vagina.
- They meet just superior to the clitoris to form a fold of skin called the prepuce (clitoral hood).
- In young females the labia minora are usually united posteriorly by a small fold of the skin, the frenulum of the labia minora.
The Vestibule of the Vagina
- The vestibule is the space between the labia minora.
- The urethra, vagina, and ducts of the greater vestibular glands open into the vestibule.
The external urethral orifice
- This median aperture is located 2 to 3 cm posterior to the clitoris and immediately anterior to the vaginal orifice.
- On each side of this orifice are the openings of the ducts of the paraurethral glands (Skene’s glands).
- These glands are homologous to the prostate in the male.
The Vaginal Orifice
- This large opening is located inferior and posterior to the much smaller external urethral orifice.
- The size and appearance of the vaginal orifice varies with the condition of the hymen, a thin fold of mucous membrane that surrounds the vaginal orifice.
The greater vestibular glands
- These glands are about 0.5 cm in diameter.
- They are located on each side of the vestibule of the vagina, posterolateral to the vaginal orifice.
- They are round or oval in shape and the bulbs of the vestibule partly overlap them posteriorly.
- From the anterior parts of the glands, slender ducts pass deep to the bulbs of the vestibule and open into the vestibule of the vagina on each side of the vaginal orifice.
- These glands secrete a small amount of lubricating mucus into the vestibule of the vagina during sexual arousal.
- The greater vestibular glands (Bartholin’s glands) are homologous with the bulbourethral glands in the male
The clitoris
- The clitoris is 2 to 3 cm in length.
- It is homologous with the penis and is an erectile organ.
- Unlike the penis, the clitoris is not traversed by the urethra; therefore it has no corpus spongiosum.
- The clitoris is located posterior to the anterior labial commissure, where the labia majora meet.
- It is usually hidden by the labia when it is flaccid.
- The clitoris consists of a root and a body that are composed of two crura, two corpora cavernosa, and a glans.
- It is suspended by a suspensory ligament.
- The parts of the labia minora passing anterior to the clitoris form the prepuce of the clitoris (homologous with the male prepuce).
- The parts of the labia passing posterior to the clitoris form the frenulum of the clitoris, which is homologous with the frenulum of the penile prepuce.
- The clitoris, like the penis, will enlarge upon tactile stimulation, but it does not lengthen significantly.
- It is highly sensitive and very important in the sexual arousal of a female.
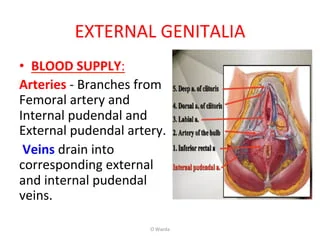
Arterial supply of female external genitalia
- The rich arterial supply to the vulva is from two external pudendal arteries and one internal pudendal artery on each side.
- The internal pudendal artery supplies the skin, sex organs, and the perineal muscles.
- The labial arteries are branches of the internal pudendal artery, as are the dorsal and deep arteries of the clitoris.
Venous drainage
- The labial veins are tributaries of the internal pudendal veins and venae comitantes of the internal pudendal artery.
Lymph drainage of the female external genitalia
- The vulva contains a very rich network of lymphatic channels.
- Most lymph vessels pass to the superficial inguinal lymph nodes and deep inguinal nodes.
reproductive system Read More »