Table of Contents
ToggleTYPHOID FEVER(Enteric fever)
Typhoid fever is an acute bacterial infection characterized by fever and is primarily spread through contaminated food and water.
Causes
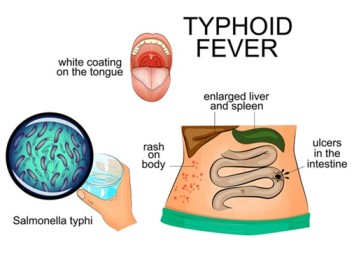
Typhoid fever is caused by Salmonella typhi and Salmonella paratyphi A and B.
- Enteric fever: A febrile inflammatory reaction due to the presence of bacteria in the intestines. Typhoid fever is a specific type of enteric fever caused by Salmonella Typhi.
- Salmonellosis: A general term for infections caused by bacteria of the genus Salmonella. Typhoid fever is a specific type of salmonellosis caused by Salmonella Typhi.
- Typhoid fever: A systemic infectious fever characterized by high fever, malaise, enteritis (inflammation of the intestines), rose-spot rash, and involvement of the lymphoid tissues (like the spleen). It is caused by the bacterium Salmonella Typhi.
Salmonella Typhi:
Classification: Salmonella Typhi belongs to the Enterobacteriaceae family, a group of bacteria commonly found in the intestines of mammals. They are flagellated (have hair-like structures for movement).
Characteristics:
- Gram-negative: They stain pink when subjected to a Gram stain, a common diagnostic tool for bacteria.
- Aerobic or facultatively aerobic: They can survive with or without oxygen.
- Metabolism: They typically thrive at 37°C and utilize glucose and mannose for energy.
- Antigens: Salmonella Typhi possess both cell wall antigens (O) and flagella antigens (H), which help them invade host cells.
Serological Testing: The serum (blood fluid) of infected patients can be used in agglutination tests, where the serum is mixed with specific antisera (antibodies) to detect the presence of O or H antigens.
Commensalism: Salmonella species are common commensals in the gastrointestinal tract (GIT) of poultry, domestic pets, birds, and humans. However, Salmonella Typhi is unique in that it only affects humans.
Predisposing Factors/Causes:
- Inadequate hygiene: Poor handwashing after defecation/urination, especially in areas with inadequate sanitation, can lead to the spread of the bacteria.
- Vectors: Flies, which can carry the bacteria on their bodies, can spread the infection.
- Poor environmental hygiene: Lack of clean water, overcrowding, inadequate excreta disposal (lack of latrines) all contribute to the spread of typhoid fever.
- Poor nutrition and poverty: Malnourished individuals and those living in poverty are more susceptible to infections, including typhoid fever.
- Achlorhydria: Lack of stomach acid (HCl) can decrease the ability to kill the bacteria.
- Schistosomiasis: This parasitic infection can compromise intestinal integrity, making it easier for bacteria to invade.
- Homogenous sickle cell disease patients: Individuals with this genetic condition are more susceptible to infections.
Incidence:
- Age group: Typhoid fever can affect individuals of any age, but the peak incidence is between 10 to 25 years. It is more common in women.
- Dose of organisms:
- A dose of 100,000 organisms can cause disease in 25% of individuals.
- A dose of 1,000,000,000 organisms results in disease in 95% of cases.
- Increasing the dose of bacteria generally leads to a shorter incubation period.
- Gastric acidity (pH) plays a role in killing ingested bacteria, with low pH levels (more acidic) being more effective.
Incubation Period:
- The incubation period for typhoid fever is usually 2 to 3 weeks.
Transmission
- Typhoid fever is contracted by the ingestion of the bacteria in contaminated food or water.
- Patients with acute illness can contaminate the surrounding water supply through stool, which contains a high concentration of the bacteria.
- About 3-5% of patients become carriers of the bacteria after the acute illness. Some patients suffer a very mild illness that goes unrecognized, and these patients can become long-term carriers of the bacteria.
- The bacteria multiply in the gallbladder, bile ducts, or liver and pass into the bowel.
- The bacteria can survive for weeks in water or dried sewage.
- The chronic carriers may have no symptoms and can be the source of new outbreaks of typhoid fever for many years.
Transmission Routes:
- Contact with formites: Contact with objects contaminated with feces or urine from patients or carriers.
- Flies: Flies can carry the bacteria and spread it through contact with food or surfaces.
- Ingestion: The most common route of transmission is through ingestion of contaminated food or water.
- Ano-oral transmission: Direct transmission from feces to mouth, especially prevalent in settings with high carrier rates, like prisons.
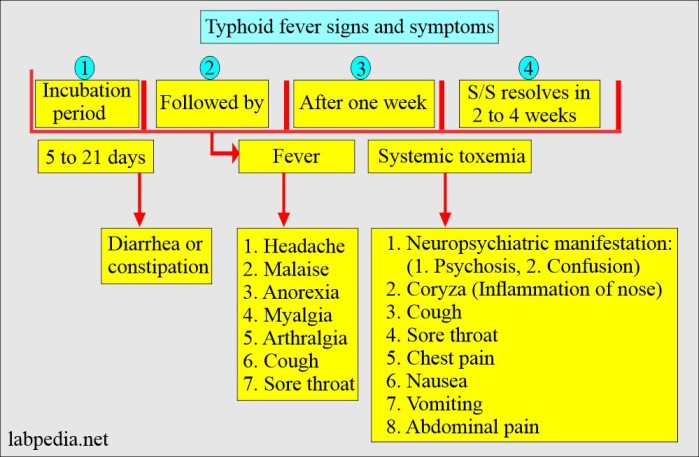
Signs and Symptoms of Typhoid Fever
Classically, the course of untreated typhoid fever is divided into four stages, each lasting approximately one week.
First week:
- In the first week, there is a gradual rise in temperature (step-ladder fashion) accompanied by bradycardia, malaise, headache, generalized body aching, restlessness, and cough.
- Epistaxis (nosebleeds) is observed in about a quarter of cases.
- Abdominal pain may also be present.
- Leukopenia, eosinopenia, and relative lymphocytosis are evident in blood tests.
- The classic Widal test, used to detect antibodies against Salmonella, is negative in the first week, but blood culture reveals the presence of Salmonella typhi.
- The payer patches of the distal end of the ileum are invaded by the bacillus and become inflamed, resulting in various manifestations such as slow pulse rate, severe persistent frontal headache, general malaise, anorexia, nausea, vomiting, intestinal upset (diarrhea and constipation), and depression of bone marrow.
Second week:
- The payer patches form a slough (a layer of dead skin).
- In the second week of the infection, the patient becomes severely ill with high fever, often reaching around 40°C (104°F), and bradycardia.
- Delirium is common, characterized by a state of calmness or, at times, agitation.

- Rose spots, which are pink spots, appear on the lower chest and abdomen in about one-third of patients.
- The abdomen becomes distended and painful, especially in the right lower quadrant.
- Diarrhea may occur, with stool appearing green and having a characteristic smell resembling pea soup. However, constipation can also be frequent.
- The spleen and liver enlarge (hepatosplenomegaly) and become tender.
- The Widal reaction shows strong positivity with anti-O and anti-H antibodies, while blood cultures may still be positive at this stage.
- The tongue is coated with a brownish fur, and sordes indicate severe toxemia.
- Dehydration becomes evident.
Third week:
- In the third week of typhoid fever, several complications may arise:
- The slough separates, leaving deep ulcers in the intestines.
- Ulcers may erode blood vessels, leading to hemorrhage, or perforate the ileum, causing leakage of intestinal contents into the peritoneal cavity.
- The patient becomes extremely ill and toxic.
- Temperature remains very high and intermittent.
- Pulse becomes feeble.
- The patient lapses into a typhoid state, experiencing delirium and confusion.
- Twitching of limbs may occur due to loss of calcium in the diarrhea state.
- Carforragic picking may lead to clotting issues and blood-stained clothes.
- Tough dries and flurried lips are observed due to severe dehydration from profuse diarrhea.
- Signs of congestive cardiac failure (CCF) due to weakened myocardium may be present.
- The patient may experience coma every eight hours.
- Peritonitis, inflammation of the peritoneum, may occur.
- By the end of the third week, the patient becomes emaciated, fever starts to subside, abdominal symptoms become more pronounced, and mental disturbances become prominent.
Fourth week:
- The ulcers begin to heal through granulation.
- At the beginning of the fourth week, the fever begins to decline, and the other symptoms gradually reduce as the patient’s temperature returns to normal.
- Recovery is slow during this stage, and relapses are common.
- If left untreated, typhoid fever can prove fatal in up to 25% of all cases.
To summarize;
Clinical Presentation:
Week 1 (Week of Onset):
- Gradual onset: Symptoms typically develop gradually, but a sudden onset, especially with shivering and rigors (intense shaking chills), can occur in “paralytic typhoid.”
- Progressive symptoms: Symptoms increase in severity over 3 to 4 days, often leading to bed rest.
- Headache: A severe headache is common, accompanied by malaise, anorexia, limb pain, insomnia, and epistaxis (nosebleed).
- Nausea and vomiting: The patient feels unwell, with nausea and vomiting.
- Abdominal pain: Pain in the abdomen, often diffuse, with normal bowel movements or sounds initially. The abdomen may become distended with gas.
- Constipation or diarrhea: Both constipation and diarrhea can occur.
- Chest pain and cough: Chest pain and cough due to bronchitis are common.
- Fever: The temperature rises steadily and remittently (fluctuates but does not return to normal) in a “step ladder” pattern, reaching 40-41°C within 24 to 48 hours. After a period of sustained fever, it starts to remit (decrease) at night and eventually resolves by lysis (gradual decrease).
- Bradycardia: A slow pulse rate (70-90 bpm) is a classic sign of typhoid fever.
- Splenomegaly and hepatomegaly: Enlargement of the spleen and liver.
- Nerve deafness: Common in the first week.
Week 2 (Infective Week):
- Ulceration and sloughing: Peyer’s patches ulcerate and slough off, and blood and necrotic tissue may be passed in the stool.
- Sustained fever: The temperature remains high.
- Increased pulse rate: The pulse rate increases while the volume decreases.
- Abdominal distention and tenderness: The abdomen continues to distend and become tender, especially in the right iliac fossa (lower end of the ileum).
- Offensive stool: The stool is foul-smelling and yellow, often described as having a “pea-soup” color.
- Muscle aches: Muscle pain is prominent.
- Rose spots: “Red-rose” spots appear on the chest and abdomen, usually starting around the 7th day and disappearing after 3 days.
Week 3 (Complications Week):
- Increased toxaemia: Severe cases are marked by complications arising from increased toxaemia (toxins in the bloodstream), which spreads to various organs and systems.
- Severe illness: The patient becomes very ill, confused, hallucinatory, and mentally apathetic, exhibiting carphologia (picking at the bedclothes).
- Delirium: The patient develops moderate delirium.
- Temperature falls by lysis: The temperature falls gradually.
- Weak and rapid pulse: The pulse is weak and rapid, and the patient is anemic.
- Dry mouth: The mouth is dry, the tongue turns brown, and halitosis (bad breath) is present.
- Mouth ulcers: Ulcers develop on the gums and mouth.
- Hot, dry, and jaundiced skin: The skin is hot, dry, and jaundiced.
- Semiconsciousness: The patient may become semiconscious and incontinent of urine and stool.
- Death: Death can occur in severe cases.
Week 4 (Recovery Week):
- Convalescence: This is a period of gradual recovery.
- Ulcer healing: The ulcers gradually granulate and heal between the 3rd and 5th week, usually without scar formation.
- Improvement: The patient gradually improves, temperature returns to normal by lysis, and other symptoms subside.
Investigations for Typhoid Fever:
Stool Culture: Stool culture involves collecting a sample of the patient’s stool and incubating it under specific conditions to identify and isolate the causative bacteria, usually Salmonella typhi or Salmonella paratyphi. The presence of these bacteria in the stool confirms the diagnosis of typhoid fever.
Blood Culture: Blood sample is collected and cultured in a suitable medium to identify and isolate the bacteria causing typhoid fever. A blood culture is an effective method to confirm the diagnosis, especially in the early stages of the disease when stool cultures might be negative.
Widal Test: The Widal test is a serological test used to detect antibodies produced by the body in response to the infection by Salmonella typhi. The test measures the presence of specific antibodies, including anti-O and anti-H antibodies, in the patient’s blood. A positive Widal test suggests a recent or past infection with typhoid fever. However, it is important to note that the Widal test results should be interpreted cautiously, as false-positive results can occur due to cross-reactivity with other infections or previous vaccinations.
Additional Investigations (optional):
Polymerase Chain Reaction (PCR) Test: PCR is a molecular diagnostic test that can detect the genetic material (DNA or RNA) of the Salmonella bacteria directly from clinical samples, such as blood or stool. PCR is a highly sensitive and specific method, and it can provide rapid results, aiding in early detection and timely treatment of typhoid fever.
Typhoid Serology: Typhoid serology involves analyzing the patient’s blood for specific antibodies against Salmonella typhi. This test, similar to the Widal test, helps in confirming a recent or past infection, but it may have limitations in terms of sensitivity and specificity.
Complete Blood Count (CBC): A CBC is a routine blood test that provides information about the number and types of blood cells. In typhoid fever, the CBC may show leucopenia (low white blood cell count), eosinopenia (low eosinophil count), and relative lymphocytosis (increased lymphocyte percentage). These abnormalities can help in supporting the diagnosis of typhoid fever.
Liver Function Tests (LFTs): Liver function tests assess the health of the liver and its ability to function properly. In typhoid fever, liver involvement is common, and LFTs can reveal elevated liver enzymes and other liver-related abnormalities.
Urinalysis: Urinalysis may be performed to check for the presence of white blood cells or other indicators of kidney involvement, which can occur in severe cases of typhoid fever.
Complications of Typhoid Fever:
I. Gastrointestinal Complications:
A. Perforation: The ulcerated areas in the intestines can lead to perforation, causing leakage of intestinal contents into the abdominal cavity. This can result in severe abdominal pain and peritonitis.
B. Hemorrhage: The erosion of blood vessels by ulcers can cause gastrointestinal bleeding, leading to blood loss and anemia.
C. Peritonitis: Perforation of the intestine can lead to peritonitis, an inflammation of the peritoneum (the lining of the abdominal cavity), causing severe abdominal pain and tenderness.
II. Gallbladder Complications:
A. Cholecystitis: The infection can spread to the gallbladder, causing inflammation known as cholecystitis, which leads to abdominal pain, fever, and tenderness in the right upper abdomen.
III. Respiratory Complications:
A. Pneumonia: In severe cases, typhoid fever can lead to pneumonia, a lung infection characterized by fever, cough, and difficulty breathing.
IV. Cardiovascular Complications:
A. Heart Failure: Severe and untreated typhoid fever can put a strain on the heart, leading to congestive heart failure, a condition where the heart fails to pump blood effectively, resulting in fluid accumulation in the body.
V. Musculoskeletal Complications:
A. Osteomyelitis: In rare cases, typhoid fever bacteria can spread to the bones, causing osteomyelitis, which is an infection of the bone and bone marrow.
VI. Neurological Complications:
A. Encephalitis: Typhoid fever can lead to encephalitis, which is inflammation of the brain. This can cause symptoms such as headache, confusion, and altered mental state.
B. Meningitis: In some instances, the infection may also spread to the meninges, the protective membranes covering the brain and spinal cord, leading to meningitis.
C. Mental Confusion: During the advanced stages of the disease, mental confusion and delirium may occur due to the systemic effects of the infection on the central nervous system.
Management of Typhoid Fever
- Hospital Admission:
- In severe cases of typhoid fever, hospital admission is necessary to provide close monitoring and appropriate medical care.
- Isolation or Barrier Nursing:
- Patients with typhoid fever should be isolated or barrier nursed to prevent the spread of the infection to others.
- Investigations:
- Blood for Culture and Sensitivity (C/S) should be performed during the first week to identify the causative bacteria and determine its sensitivity to antibiotics.
- Full Blood Sample (FBS) analysis will reveal low Hemoglobin (Hb) levels, low White Blood Cell (WBC) count, and an increased Erythrocyte Sedimentation Rate (ESR).
- The Widal test can be done around 10/7 days after the onset of symptoms to detect antibodies against typhoid bacilli.
- Blood Smear (B/S) examination should be conducted to rule out malaria.
- Stool analysis and urinalysis are important to assess gastrointestinal and urinary involvement in typhoid fever.
- Drug Therapy:
- Antibiotic therapy is a cornerstone of typhoid fever management:
- Ciprofloxacin at a dose of 500-750 mg twice daily for 10/7 (10 days).
- Azithromycin at a dose of 10 mg/kg daily.
- Cotrimoxazole at a dose of 960 mg twice daily for 3/7 (3 days) or as per a weight-based calculation for 10/7 (10 days).
- Long-Term Carriers:
- After signs have passed, stool tests should be conducted to check if Salmonella typhi bacilli are still present. Patients may become potential long-term carriers of the bacteria, requiring a 28-day course of antibiotics to eliminate the bacteria until they are free from it.
- Fluid and Electrolyte Management:
- Monitor intravenous (IV) fluid administration for rehydration.
- Correct fluid and electrolyte imbalances with Normal Saline (N/S), Dextrose 5% (D5%) solutions, and oral fluids.
- Nutrition:
- Ensure adequate nutrition and provide a soft, easily digestible diet, unless the patient has abdominal complications or ileus.
- Antipyretics:
- Administer antipyretics like Paracetamol (PCM) to manage fever.
- Hygiene and Infection Control:
- Pay close attention to handwashing and limit close contact with individuals during the acute phase of the infection to prevent its spread.
- Encourage proper waste disposal, covering of food, and proper food preparation to reduce contamination risks.
- Encourage early screening and management to prevent the worsening of the disease.
- Proper Water Treatment and Storage:
- Educate patients on the proper treatment and storage of water to avoid waterborne transmission of the bacteria.
- Regular Follow-Up and Monitoring:
- Ensure regular follow-up and monitor for complications and clinical relapses.
- Management of Delirium:
- Encourage the use of Phenobarbital at a dose of 30-60 mg in case of delirium.
Treatment:
Antibiotic therapy:
- Hospitalized patients: For hospitalized patients, treatment typically involves intravenous antibiotics, such as ceftriaxone or ciprofloxacin.
- Hospitalized patients:
- Ceftriaxone: 1-2 grams IV daily for 10-14 days.
- Ciprofloxacin: 500-750mg IV twice daily for 10-14 days.
- Non-hospitalized patients: For non-hospitalized patients with mild to moderate symptoms, oral antibiotics, such as ciprofloxacin or azithromycin, are often prescribed.
- Non-hospitalized patients:
- Ciprofloxacin: 500-750mg orally twice daily for 5-14 days.
- Azithromycin: 500mg orally once daily for 3 days.
Supportive care: Provide supportive care, including:
- Fluid replacement: Intravenous fluids or oral rehydration solutions are essential to prevent dehydration.
- Pain management: Over-the-counter pain relievers can help manage pain and fever.
- Nutritional support: Encourage adequate nutrition to support recovery.
Chronic Carriers:
- Hospitalized patients: Hospitalized chronic carriers may require prolonged antibiotic therapy with medications like amoxicillin or ciprofloxacin.
- Amoxicillin: 250mg orally three times daily for 4-6 weeks.
- Ciprofloxacin: 500-750mg orally twice daily for 4-6 weeks.
- Non-hospitalized patients: Non-hospitalized carriers may require ongoing monitoring and may be advised to avoid working in food-handling positions.
Immediate Nursing Care:
- Rehydration: Provide intravenous fluids, nasogastric tube feeding, or oral rehydration solutions as needed to combat dehydration.
- Temperature control: Implement tepid sponging and other measures to cool the patient’s temperature.
- Hygiene: Maintain strict hygiene practices, including:
- Skin care: Keep the patient’s skin clean and dry.
- Mouth care: Provide oral hygiene to prevent mouth sores.
- Nail care: Keep the patient’s nails trimmed and clean.
- Perineal care: Keep the perineal area clean to prevent infection.
- Personal protective equipment (PPE): Wear gloves, aprons, and goggles when handling anything from the patient to minimize exposure to bacteria.
- Handwashing: Ensure frequent handwashing with soap and water and drying with clean towels.
- Safe water and food: Use only treated or boiled water for drinking and cooking.
- Disinfection: Dispose of wastes and excreta properly, disinfecting all contaminated items. Use disposable cups and plates whenever possible.
- Non-disposable items: Disinfect non-disposable articles with concentrated disinfectants, replacing them regularly.
- Linen treatment: Treat linens as infected material.
- Terminal disinfection: Carry out terminal disinfection after the patient’s discharge.
- Monitoring: Closely monitor the patient’s condition, particularly abdominal pain, diarrhea, constipation, and any signs of complications. Report any changes promptly.
- Diet: Initially, provide a fluid diet high in calories, followed by a balanced, nutritious, soft diet (6-8 small meals).
- Fluid and elimination: Monitor fluid intake and output, and assist with elimination as needed.
- Psychological support: Offer emotional support to the patient.
- Physiotherapy: Provide physiotherapy after the acute stage to help the patient regain strength and mobility.
Prevention:
- Maintain cleanliness in the premises and ensure proper disposal of rubbish.
- Keep hands clean and maintain trimmed fingernails.
- Wash hands thoroughly with soap and water before eating or handling food and after using the toilet or changing diapers.
- Drinking water should be free from microorganisms; it is preferable to boil water before consumption.
- Avoid high-risk foods, such as raw or semi-cooked food.
- During food preparation, wear clean, washable aprons, and caps.
- Clean and wash food thoroughly, including scrubbing and rinsing fruits in clean water.
- Store perishable food in the refrigerator, covering it properly.
- Cook food thoroughly before consumption.
- Consume food as soon as it is prepared.
- If necessary, refrigerate cooked leftover food and consume it promptly. Reheat it thoroughly before consumption.
- Exclude infected individuals and asymptomatic carriers from handling food and providing care to children.
- Consider immunization, especially for those traveling to high-risk areas, where vaccines are available in oral and injectable forms.
Test MCQ Questions
Question 1:
What is the primary mode of transmission for typhoid fever?
A) Mosquito bites
B) Contaminated food and water
C) Airborne droplets
D) Direct physical contact
Question 2:
Which bacterium is responsible for causing typhoid fever?
A) Escherichia coli
B) Salmonella typhi
C) Streptococcus pneumoniae
D) Staphylococcus aureus
Question 3:
Which of the following complications can occur in severe cases of typhoid fever?
A) Fractures
B) Renal failure
C) Dental caries
D) Cholecystitis
Question 4:
Which diagnostic test is used to identify the presence of Salmonella typhi in the blood?
A) Blood smear examination
B) Stool culture
C) Urinalysis
D) Blood culture
Question 5:
What is the recommended antibiotic therapy for treating typhoid fever?
A) Penicillin
B) Amoxicillin
C) Ciprofloxacin
D) Erythromycin
Question 6:
Why is hospital admission often recommended in severe cases of typhoid fever?
A) To provide psychological support to the patient
B) To administer vaccines for long-term immunity
C) To ensure isolation and prevent disease transmission
D) To allow close monitoring and provide appropriate medical care
Question 7:
What is the primary preventive measure to avoid typhoid fever transmission in the community?
A) Proper handwashing with soap and water
B) Mosquito net usage
C) Wearing masks in public places
D) Vaccination against other bacterial infections
Question 8:
Which gastrointestinal complication can occur due to typhoid fever?
A) Pneumonia
B) Peritonitis
C) Otitis media
D) Conjunctivitis
Question 9:
Which of the following is NOT a recommended step to prevent typhoid fever?
A) Drinking untreated water from natural sources
B) Cooking food thoroughly
C) Washing hands properly before eating
D) Proper waste disposal
Question 10:
Who should be excluded from handling food and providing care to children during a typhoid fever outbreak?
A) Asymptomatic carriers and infected individuals
B) Healthcare professionals only
C) Pregnant women
D) Children under 5 years of age
Answers:
- B – Contaminated food and water
- B – Salmonella typhi
- D – Cholecystitis
- D – Blood culture
- C – Ciprofloxacin
- D – To allow close monitoring and provide appropriate medical care
- A – Proper handwashing with soap and water
- B – Peritonitis
- A – Drinking untreated water from natural sources
- A – Asymptomatic carriers and infected individuals
Explanation:
- Typhoid fever is primarily spread through contaminated food and water, making option B the correct answer.
- Salmonella typhi is the bacterium responsible for causing typhoid fever, making option B the correct answer.
- Cholecystitis is one of the gastrointestinal complications associated with typhoid fever, making option D the correct answer.
- Blood culture is used to identify the presence of Salmonella typhi in the blood, making option D the correct answer.
- Ciprofloxacin is one of the recommended antibiotics for treating typhoid fever, making option C the correct answer.
- Hospital admission is recommended in severe cases of typhoid fever for close monitoring and appropriate medical care, making option D the correct answer.
- Proper handwashing with soap and water is the primary preventive measure to avoid typhoid fever transmission, making option A the correct answer.
- Peritonitis is a gastrointestinal complication that can occur due to typhoid fever, making option B the correct answer.
- Drinking untreated water from natural sources is NOT a recommended step to prevent typhoid fever, making option A the correct answer.
- Asymptomatic carriers and infected individuals should be excluded from handling food and providing care to children during a typhoid fever outbreak, making option A the correct answer.

amonginancy21@gmail.com
Thanks
Thanks for the good work may Allah reward you
Thanks alot