Table of Contents
ToggleTuberculosis
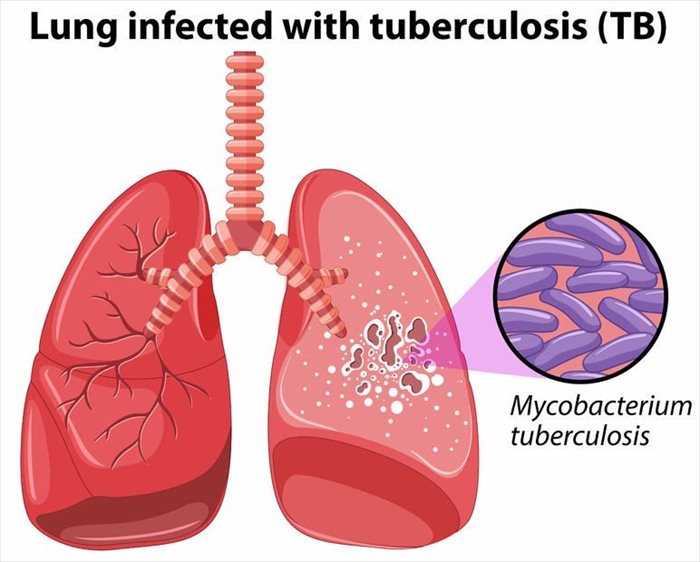
Tuberculosis, commonly known as TB (short for tubercle bacillus), is a widespread and often deadly infectious disease caused by various strains of mycobacteria.
While primarily affecting the lungs, it can also impact other parts of the body. Around one-third of the world’s population (1 in 3 or 3 out of 10 people) is affected by this condition. Individuals with HIV/AIDS have a higher risk of contracting tuberculosis.
Aetiology:
The disease is caused by mycobacterium tuberculosis, which is a small, aerobic, non-motile bacillus.
Mode of Spread
TB spreads through the air when individuals with an active infection cough, sneeze, or transmit respiratory fluids. Additionally, it can spread through the blood (haematogenous spread).
Types of Tuberculosis
- Pulmonary tuberculosis.
- Extra-pulmonary tuberculosis.
- Primary and Secondary tuberculosis.
Clinical Features:
Pulmonary TB:
- Fever and chills
- Night sweats
- Loss of appetite
- Weight loss
- Easy fatigability
- Persistent cough lasting more than 3 weeks, with or without haemoptysis (coughing up blood)
- Significant finger clubbing (abnormal swelling of the fingertips)
- Chest pain
- Productive cough or non-productive cough in smear-negative TB
- Lymphadenopathy (swollen lymph nodes)
Extrapulmonary TB:
In approximately 15-20% of active TB cases, the infection spreads beyond the lungs, resulting in various forms of extrapulmonary tuberculosis. This type is more common in individuals with weakened immune systems and young children. In people with HIV, extrapulmonary TB occurs in more than 50% of cases.
Notable sites of extrapulmonary infection include:
- The pleura, leading to tuberculous pleurisy.
- The central nervous system, causing tuberculous meningitis.
- The lymphatic system, resulting in TB lymph nodes.
- The genitourinary system, causing urogenital tuberculosis.
- The bones and joints, leading to Pott’s disease of the spine. When it affects the bones, it is known as “osseous tuberculosis,” a form of osteomyelitis.
- Sometimes, a tubercular abscess may burst through the skin, resulting in a tuberculous ulcer. Ulcers originating from infected lymph nodes nearby are typically painless.
- A potentially severe and widespread form of TB is “disseminated” TB, commonly known as miliary tuberculosis. Miliary TB accounts for about 10% of extrapulmonary cases.
Risk factors
Several factors increase the susceptibility of individuals to TB infections:
- HIV infection is a significant global risk factor, contributing to 13% of all TB cases.
- Tuberculosis is closely associated with overcrowding and malnutrition, making it a prevalent disease in impoverished communities.
- Inhabitants and employees of places where vulnerable individuals gather, such as prisons and homeless shelters, face higher risks.
- Medically underserved and resource-poor communities, as well as high-risk ethnic minorities, are more susceptible.
- Children in close contact with high-risk patients are at increased risk.
- Health care providers serving TB patients are also at higher risk.
- Chronic lung disease is another significant risk factor.
- Smokers have nearly double the risk of TB compared to nonsmokers.
- Other conditions like alcoholism and diabetes mellitus can also elevate the risk of developing tuberculosis.
Epidemiology:
- Approximately one-third of the world’s population is infected with tuberculosis.
- TB causes 25% of preventable adult deaths, and three-fourths of these affected individuals are in their productive age.
- South Eastern Asia has the highest number of TB cases.
- Africa has the world’s highest incidence rate, with an annual incidence rate of 345 cases per 100,000 people.
- The infection rate is higher in men than in women.
Primary Tuberculosis:
- It occurs in individuals who have never been exposed to tubercle bacilli before.
- Tubercle bacilli are inhaled and reach the lungs, where they multiply and can spread to the hilar lymph nodes through the lymphatic system and blood.
- Approximately six weeks after the primary infection, the body’s immune response kicks in, preventing further multiplication of the tubercle bacilli.
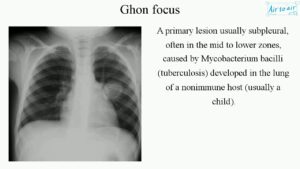
- Some bacilli may die, and the remaining ones are walled off by immune cells called epithelioid cells, forming a ghon focus. This ghon focus can persist for years in primary tuberculosis.
- The ghon focus and hilar lymphadenopathy together form a primary complex in primary tuberculosis.
- Only about 10% of those with primary infection progress to develop tuberculosis disease.
Secondary Tuberculosis:
- This type of tuberculosis can result from either the reactivation of tubercle bacilli acquired during primary infection or reinfection by tubercle bacilli in a person previously exposed to the organisms.
Pathogenesis:
- TB infection starts when mycobacteria reach the pulmonary alveoli and invade and replicate there.
- In addition to the lungs, tuberculosis can spread through the bloodstream, leading to infection in distant sites like peripheral lymph nodes, kidneys, brain, and bones.
- The infection triggers an inflammatory response, resulting in the formation of granulomas. Granulomas are collections of activated macrophages, T lymphocytes, B lymphocytes, and fibroblasts.
- The tubercle bacilli are surrounded by lymphocytes, forming a peripheral rim and creating a Ghon focus. (see image below)
- Inside the granulomas, the bacteria can become dormant, causing latent infection. Caseation, a type of abnormal cell death, occurs in the center of the tubercles.
- In severe cases, where TB bacteria enter the bloodstream from damaged tissue, multiple foci of infection can develop throughout the body, appearing as tiny white tubercles in the tissues. This condition is known as miliary tuberculosis and is more common in young children and individuals with HIV.
- Tissue destruction and necrosis are balanced by healing and fibrosis. Scarring and cavities filled with caseous necrotic material replace affected tissue.
Diagnosis (Investigations):
When tuberculosis is suspected, the following investigations can aid in confirming the diagnosis:
- Signs of lung disease or constitutional symptoms lasting longer than two weeks.
- Chest X-ray: Imaging the chest can reveal characteristic abnormalities, such as infiltrates, cavities, or nodules, which can indicate tuberculosis.
- Multiple sputum cultures for acid-fast bacilli (AFB): Sputum samples are collected at different times, typically spot samples and early morning samples, to increase the chances of detecting the tuberculosis bacteria.
- Tuberculin skin tests: Also known as the Mantoux or Heaf test, it is commonly used to assess TB infection in children and identify individuals at risk of developing tuberculosis.
- Haematological tests:
- Full blood cell count (FBC): This test helps evaluate any abnormalities in blood cell counts that may be indicative of an infection or inflammation.
- Erythrocyte Sedimentation Rate (ESR): An elevated ESR can raise suspicion of tuberculosis, as it indicates inflammation in the body.
- Tissue biopsy: In cases where tuberculosis affects extrapulmonary sites or when other tests are inconclusive, a biopsy of the affected tissue may be performed to examine the presence of tubercle bacilli.
Relationship between HIV and TB:
Effects of HIV on TB:
- Development of active TB: Individuals infected with HIV have a higher risk of developing active tuberculosis once exposed to the TB bacteria.
- High risk of re-infection: HIV-positive individuals are more susceptible to being infected with a second strain of TB after already having the infection.
- Increased incidence of TB: The overall incidence of tuberculosis increases due to the higher prevalence of HIV, which weakens the immune system and makes individuals more susceptible to TB.
- Changes in TB presentation: TB in HIV-positive individuals may present with clinical and bacteriological changes, such as a non-productive cough, absence of hemoptysis (coughing up blood), and a miliary pattern on imaging instead of cavitations.
- Quicker development of TB complications: HIV accelerates the progression of TB and its associated complications.
Effects of TB on HIV:
- Increased HIV replication: TB infection can enhance the replication of HIV, leading to a higher viral load and faster progression to AIDS.
- Common opportunistic infection: TB is one of the most common opportunistic infections in individuals living with HIV and is a leading cause of death in this population.
- Interference with ARV treatment: Some anti-TB medications, such as Rifampicin, can interfere with certain antiretroviral drugs (ARVs), like Nevirapine and protease inhibitors, necessitating adjustments in treatment.
Consequences of dual infection with HIV and TB:
- Increased morbidity and mortality.
- Higher recurrence rate of TB after completing treatment.
- Drug resistance leading to multidrug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB).
- Higher rates of treatment non-adherence due to overlapping medication regimens.
- Increased risk of drug toxicity from the combined treatment.
Management of HIV and TB co-infection:
- Prioritize TB treatment before starting ARVs.
- Start ARVs if CD4 count is below 350 cells/mm³, either after finishing TB treatment or during the intensive phase, depending on the clinical situation.
- Consider drug interactions between TB and HIV regimens when selecting medications.
- Use directly observed therapy (DOTs) for TB treatment and closely monitor patients for toxicity and adherence.
- Administer prophylaxis for opportunistic infections as indicated.
Complications of TB:
- Pleural effusion: Accumulation of fluid in the pleural space of the lungs.
- Pericardial effusion: Accumulation of fluid around the heart.
- Empyema: Pus-filled cavity in the pleural space.
- Pneumothorax: Presence of air or gas in the pleural cavity, causing lung collapse.
- Lung fibrosis: Scarring of lung tissue, leading to impaired lung function.
- Lung collapse: Collapse of a lung or part of a lung due to blockage or compression.
- Extra-pulmonary TB: TB affecting organs other than the lungs, such as TB meningitis.

Treatment of TB:
Aims of TB Treatment:
- To cure the patient of tuberculosis.
- To prevent complications and death from TB.
- To reduce the transmission of TB to others.
Case Definitions:
- New Case: A person who has never received TB treatment or has taken TB treatment for four weeks or less.
- Relapse: A patient who was previously diagnosed with TB, completed the course of anti-TB drugs, was declared cured, but has now become smear positive again.
- Failure: A person who continues to be smear positive at five months, despite adequately taking anti-TB drugs, or who was smear negative and becomes smear positive at two months.
- Defaulter: A patient who starts taking anti-TB drugs for more than four weeks but interrupts treatment (stops taking the drugs) for four weeks or more.
Drugs Used in TB Treatment:
- Rifampicin (R)
- Isoniazid (H or INH)
- Ethambutol (E)
- Pyrazinamide (Z)
- Streptomycin (S)
Standard TB Treatment Regimen:
The World Health Organization (WHO) recommends a standard six-month treatment regimen for drug-sensitive TB cases, which typically includes the following four drugs for the first two months:
- Rifampicin (R)
- Isoniazid (H)
- Pyrazinamide (Z)
- Ethambutol (E)
This initial phase is followed by a continuation phase for the next four months, during which the drugs used may vary depending on the patient’s response to treatment and drug sensitivity testing.
It’s important to note that TB treatment should be administered under direct observation (DOTs) whenever possible to ensure proper adherence and to prevent the development of drug-resistant TB strains. Check DOT below in details.
Treatment regimen
Short course TB treatment regimen
Patient category (type of TB) | Initial phase | Continuation phase |
1. New smear positive 2. New smear negative 3. Severe extra-pulmonary | 2EHRZ | 6EH |
4. Previously treated smear POSITIVE: – Relapse – Failure to respond – Return after interruption | 2SEHRZ/1EHRZ | 5EHR |
5. Any form of TB in children 6. Adult non-severe extra pulmonary | 2HRZ | 4HR |
Non-anti-TB Drugs Used in TB:
Pyridoxine (Vitamin B₆): Administered to prevent or treat peripheral neuropathy, a side effect of Isoniazid (H) used in TB treatment. Pyridoxine supplementation helps prevent nerve damage caused by Isoniazid.
Steroids: Used as adjunct therapy in specific forms of TB to reduce inflammation and improve outcomes. Steroids are commonly used in the treatment of:
- TB Meningitis
- TB Pericarditis
- TB of Adrenals
DOTS (Directly Observed Therapy Short course):
How it works:
- DOTS is a community-based TB care approach adopted by countries to improve TB treatment outcomes.
- Trained workers or treatment supporters ensure that patients take their daily treatment doses and record the administration on the TB card.
- DOTS is the standard of care for all TB cases and suspects.
- It helps decrease relapse, defaulter rates, and the development of acquired drug resistance.
- When combined with other measures, DOTS promotes treatment adherence.
- After diagnosing TB and initiating treatment, the diagnostic center records the information in the health unit’s TB register.
- The sub-county health worker transfers this information to the sub-county health worker register and identifies a treatment supporter in the patient’s village.
- The treatment supporter is trained to observe the patient taking their treatment, record it on the TB card, keep the drugs, and remind the patient of follow-up assessments at the health unit at 2 months, 5 months, and 8 months.
- The sub-county health worker collects medication from the health unit and delivers it to the treatment supporter.
Prevention of TB:
- Early detection and proper management of TB cases.
- Early case findings to identify and treat TB cases promptly.
- Health education to raise awareness about TB transmission and prevention.
- Training of all health workers to recognize early signs of TB.
- Vaccination of children with the Bacille Calmette-Guérin (BCG) vaccine to protect against severe forms of TB in childhood.
- Prophylaxis with Isoniazid for individuals at high risk of developing TB, such as those with latent TB infection or individuals with HIV.
- Prevention and management of medical conditions like HIV, which increase the risk of TB.
- Implementation of the DOTS program to improve treatment adherence and outcomes.

Test Questions
Question: Which bacterium is responsible for causing tuberculosis?
a) Streptococcus pneumoniae
b) Mycobacterium tuberculosis
c) Escherichia coli
d) Staphylococcus aureus
Answer: b) Mycobacterium tuberculosis
Explanation: Mycobacterium tuberculosis is the specific bacterium that causes tuberculosis.
Question: What is the most common site of TB infection in the human body?
a) Liver
b) Lungs
c) Heart
d) Kidneys
Answer: b) Lungs
Explanation: Pulmonary tuberculosis is the most common form of TB, affecting the lungs.
Question: In HIV-positive individuals, the risk of developing active tuberculosis:
a) Decreases
b) Stays the same
c) Increases
d) Remains unaffected
Answer: c) Increases
Explanation: HIV weakens the immune system, making individuals more susceptible to developing active tuberculosis once infected with Mycobacterium tuberculosis.
Question: Which of the following is NOT a clinical feature of pulmonary tuberculosis?
a) Fever and chills
b) Night sweats
c) Loss of appetite
d) Severe abdominal pain
Answer: d) Severe abdominal pain
Explanation: Severe abdominal pain is not a typical clinical feature of pulmonary tuberculosis.
Question: What is the standard duration of treatment for drug-sensitive tuberculosis?
a) 3 months
b) 6 months
c) 9 months
d) 12 months
Answer: b) 6 months
Explanation: The standard treatment regimen for drug-sensitive TB lasts for 6 months.
Question: In which form of TB, patients may present with a non-productive cough and a miliary pattern on imaging?
a) Drug-resistant TB
b) Extrapulmonary TB
c) Latent TB
d) Multidrug-resistant TB
Answer: b) Extrapulmonary TB
Explanation: Extrapulmonary TB can present with atypical symptoms like a non-productive cough and a miliary pattern on imaging.
Question: What is the main purpose of the DOTS program in TB management?
a) To prevent TB transmission
b) To promote TB vaccination
c) To monitor drug resistance
d) To improve treatment adherence
Answer: d) To improve treatment adherence
Explanation: The main aim of the DOTS program is to ensure that patients adhere to their TB treatment, which leads to better outcomes and reduced relapse rates.
Question: Which non-anti-TB drug is used to prevent or treat peripheral neuropathy, a side effect of Isoniazid?
a) Vitamin C
b) Vitamin D
c) Pyridoxine (Vitamin B₆)
d) Folic acid
Answer: c) Pyridoxine (Vitamin B₆)
Explanation: Pyridoxine is used to prevent or treat peripheral neuropathy caused by Isoniazid.
Question: TB Meningitis is best managed with the addition of which adjunct therapy?
a) Antibiotics
b) Antifungals
c) Antivirals
d) Steroids
Answer: d) Steroids
Explanation: TB Meningitis is often treated with the addition of steroids to reduce inflammation and improve outcomes.
Question: What is the primary aim of TB prevention?
a) Eradicate Mycobacterium tuberculosis from the environment
b) Reduce the incidence of drug-resistant TB
c) Prevent the transmission of TB from person to person
d) Increase vaccination coverage in high-risk populations
Answer: c) Prevent the transmission of TB from person to person
Explanation: The primary aim of TB prevention is to break the chain of transmission by preventing the spread of Mycobacterium tuberculosis from infected individuals to others.

Thanks for the assistance it’s great
The notes are so helpful for revision
Complex topics made easier to understand, thank you very much.
Thank you for the revision notes.
Very good notes and easy to understand