Table of Contents
ToggleTERMINOLOGIES
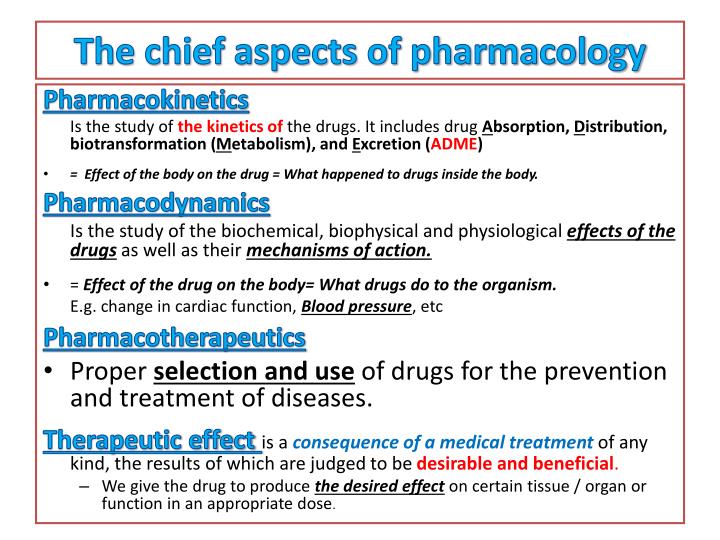
Pharmacology: The scientific study of drugs, their origins, chemical properties, actions, and uses in the treatment, diagnosis, and prevention of disease.
- Pharmacology is the scientific study of drugs and their use in medicine.
- This includes pharmacokinetics (what the body does to the drug) and pharmacodynamics (what the drug does to the body).
- In midwifery, pharmacology focuses on medications used during pregnancy, labor, delivery, and the postpartum period, considering the impact on both the mother and the fetus/newborn.
- The study of pharmacology helps a midwife to use the drugs appropriately while caring for the pregnant mother.
- Pharmacology is divided into two major branches namely;
- Pharmacokinetics and Pharmacodynamics.
Pharmacokinetics: The study of the movement of drugs within the body, including absorption, distribution, metabolism, and excretion (ADME). Understanding pharmacokinetics is vital in midwifery to determine appropriate dosage and timing of medications, considering changes in maternal physiology during pregnancy and lactation.
Pharmacodynamics: The study of the biochemical and physiological effects of drugs and their mechanisms of action. This includes drug receptor interactions and the relationship between drug concentration and effect. In midwifery, pharmacodynamics helps predict a drug’s efficacy and potential side effects in pregnant and breastfeeding women.
Drug: A substance intended for use in the diagnosis, cure, mitigation, treatment, or prevention of disease in humans or other animals.
- A drug is a chemical substance which alters the functioning of the body.
- Most drugs used in clinical practice are used to prevent, diagnose and treat diseases.
- A drug can have more than two names : chemical name, generic name and a brand name.
- The chemical names are normally used by chemists and are not used in
- clinical practice because they are usually very difficult to remember and write.
- This is a name given to a drug by an international body. Generic name of a drug is known worldwide. The Ministry of Health of Uganda recommends that all drug prescriptions should be written with generic names to avoid confusion. Examples include Oxytocin, Misoprostol.
- A brand name also called a trade name is a name given to a drug by a manufacturing company.
- All brand names begin with a capital letter and bear a symbol *. Example Amoxil*, Duramox*, Unixil*.
Medication: A drug administered for therapeutic purposes. This highlights the intentional use of a drug to achieve a specific clinical outcome.
Therapeutics: The branch of medicine concerned with the treatment of disease and the use of drugs in the prevention and treatment of disease.
- In midwifery, therapeutic interventions include pain management, infection control, and management of obstetrical complications.
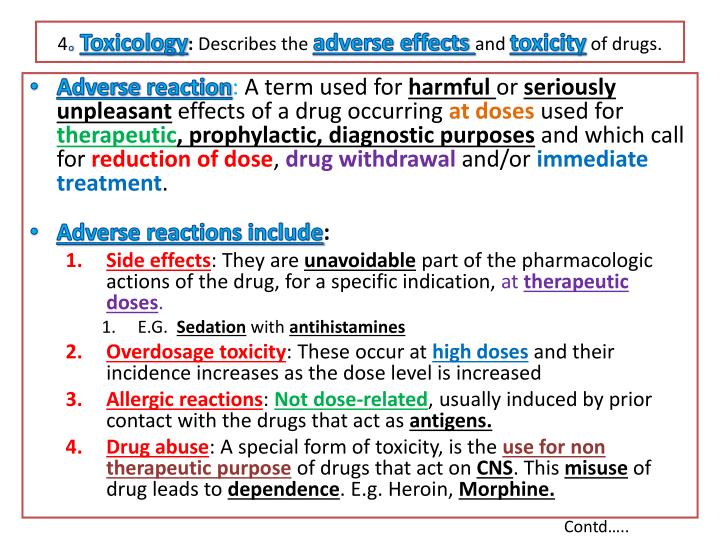
Toxicology: The study of poisons and the adverse effects of drugs and other chemicals on living organisms.
- In midwifery, toxicology is important for understanding the potential risks of medications to the mother and fetus, including teratogenicity (the ability to cause birth defects) and fetotoxicity (harm to the fetus).
Chemotherapy: The use of chemical agents (drugs) to treat diseases.
- In the context of midwifery, this might include the treatment of infections (e.g., with antibiotics) or the management of certain cancers. Specific consideration needs to be given to the potential effects on breastfeeding.
Teratogen: An agent that can cause birth defects. Many drugs are potential teratogens, and careful consideration is needed when prescribing medications during pregnancy.
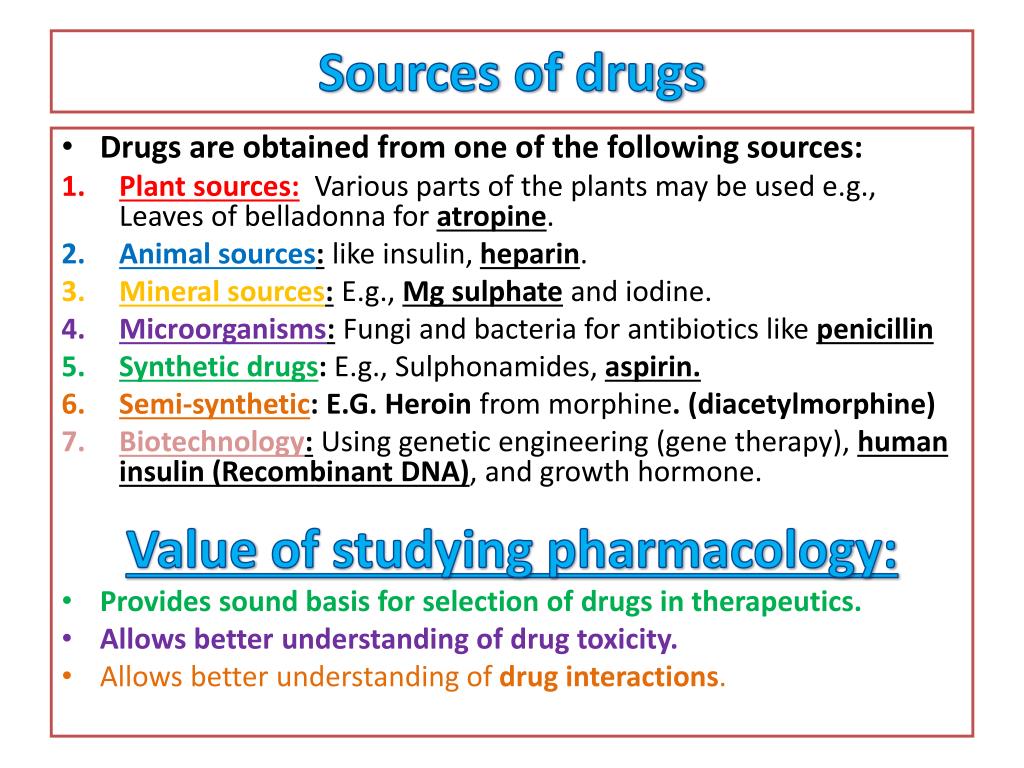
Sources of Drugs
Drugs, substances used to prevent, diagnose, treat, or cure diseases, originate from different sources. These sources can be broadly categorized as natural or synthetic.
1. Natural Sources: These sources utilize naturally occurring substances extracted or purified from living organisms or minerals.
- Plants: A rich source of medicinal compounds, plants have been used for centuries in traditional medicine. Many modern drugs are derived from or inspired by plant-based compounds. Examples include:
- Atropine: An anticholinergic alkaloid derived from plants like Atropa belladonna (deadly nightshade) used to treat certain types of poisoning and slow heart rate.
- Morphine: An opiate alkaloid extracted from the opium poppy (Papaver somniferum), a potent analgesic used to manage severe pain.
- Quinine: An antimalarial alkaloid obtained from the bark of the cinchona tree (Cinchona species).
- Digoxin: A cardiac glycoside extracted from the foxglove plant (Digitalis purpurea), used to treat heart failure and arrhythmias.
- Pilocarpine: A cholinergic alkaloid from Pilocarpus species, used to treat glaucoma and dry mouth.
- Physostigmine: A cholinesterase inhibitor from the Calabar bean (Physostigma venenosum), used to treat myasthenia gravis.
- Animals: Certain animal tissues and secretions yield valuable medicinal compounds. Examples include:
- Insulin: A hormone crucial for glucose metabolism, originally extracted from the pancreas of pigs and cattle, now primarily produced via recombinant DNA technology.
- Adrenaline (Epinephrine): A hormone and neurotransmitter vital in the “fight-or-flight” response, originally extracted from adrenal glands, now synthesized.
- Heparin: An anticoagulant extracted from animal tissues (e.g., pig intestines, cattle lungs), now also produced synthetically.
- Gonadotropins: Hormones regulating reproductive function, originally extracted from animal pituitary glands or pregnant women’s urine, now often produced via recombinant DNA technology.
- Antitoxic Sera: Preparations containing antibodies obtained from animals immunized against specific toxins.
- Minerals: Inorganic substances from the earth have also found therapeutic applications. Examples include:
- Magnesium Sulfate: Used as a laxative, anticonvulsant, and in other applications.
- Aluminum Hydroxide: An antacid used to neutralize stomach acid.
- Iron Salts: Used to treat iron deficiency anemia.
- Sulfur: Used in various topical treatments.
- Radioactive Isotopes: Used in nuclear medicine for diagnostic and therapeutic purposes (e.g., iodine-131 for thyroid cancer).
- Microorganisms: Bacteria and fungi are sources of several crucial antibiotics:
- Penicillin: A beta-lactam antibiotic produced by Penicillium fungi.
- Cephalosporins: A class of beta-lactam antibiotics derived from Cephalosporium fungi.
- Tetracyclines: A broad-spectrum antibiotic class obtained from Streptomyces bacteria.
- Humans: Certain human-derived substances have therapeutic applications:
- Immunoglobulins: Antibodies obtained from human blood plasma, used to provide passive immunity.
- Growth Hormone: A hormone regulating growth and development, originally extracted from human pituitary glands, now produced via recombinant DNA technology.
- Chorionic Gonadotropin: A hormone produced during pregnancy, originally extracted from pregnant women’s urine, now often produced synthetically.
2. Synthetic Sources: The majority of modern drugs are now produced synthetically, offering advantages such as precise control over purity, consistent quality, and scalability. These are chemically synthesized in laboratories, often mimicking or improving upon naturally occurring compounds. Examples include:
- Quinolones: A class of broad-spectrum antibiotics.
- Omeprazole: A proton pump inhibitor used to reduce stomach acid production.
- Sulfonamides: (Sulfa drugs): A class of antibiotics.
- Pancuronium: A neuromuscular blocking agent.
- Neostigmine: A cholinesterase inhibitor.
Sources and Examples of Drugs
Source | Example Drug(s) |
Plants | Atropine, Morphine, Quinine, Digoxin, Pilocarpine, Physostigmine |
Animals | Insulin, Adrenaline, Heparin |
Minerals | Magnesium Sulphate, Aluminum Hydroxide |
Microorganisms | Penicillin, Cephalosporins, Tetracyclines |
Humans | Immunoglobulins, Growth Hormone |
Synthetic | Quinolones, Omeprazole, Sulfonamides |
Pharmacokinetics
Pharmacokinetics involves the study of how drugs move through the body, focusing on four key processes: absorption, distribution, metabolism, and excretion. In brief, it is what the body does to the drug.
Absorption
Absorption refers to how a drug enters the bloodstream from its site of administration.
Factor Influencing Absorption | Description | Impact |
Route of administration | Method by which the drug is given (e.g., oral, IV) | Affects speed and efficiency of absorption |
Surface area | Area available for drug absorption (e.g., intestines have a large surface area) | Larger surface areas increase absorption rate |
Blood flow | Circulation at the absorption site | Higher blood flow enhances absorption |
Presence of food | Interaction of food with the drug in the GI tract | Can either enhance or delay absorption |
Drug formulation | Physical form of the drug (e.g., tablet, liquid) | Different forms have different absorption rates |
Distribution
Distribution is how the drug is transported from the bloodstream to various tissues and organs.
Factor Influencing Distribution | Description | Impact |
Protein binding | Degree to which a drug binds to plasma proteins | Only unbound drugs are active |
Lipid solubility | Ability to dissolve in fats | Lipophilic drugs easily cross cell membranes |
Blood circulation | Blood flow to different tissues | Organs with high blood flow receive drugs faster |
Blood-brain barrier | A selective barrier protecting the brain | Only certain drugs can cross into the CNS |
Bioavailability
Bioavailability is the proportion of a drug that reaches the systemic circulation and is available for therapeutic effect.
Route | Bioavailability | Notes |
Intravenous (IV) | 100% | Directly enters the bloodstream |
Oral (PO) | Varies (20-80%) | Affected by first-pass metabolism and GI absorption |
Subcutaneous (SC) | Moderate | Slower, sustained release into the bloodstream |
Metabolism
Metabolism involves the biochemical alteration of a drug, primarily in the liver, into an inactive or less active form.
Factor Influencing Metabolism | Description | Impact |
Age | Metabolic capacity varies with age | Neonates and elderly often metabolize drugs more slowly |
Enzyme activity | Presence of drug-metabolizing enzymes | Drugs can induce or inhibit enzyme activity, affecting metabolism |
Genetic factors | Individual genetic makeup | Variations can lead to differences in drug metabolism |
Disease states | Conditions affecting organs | Liver diseases can impair metabolism, leading to drug accumulation |
Excretion
Excretion is the removal of drugs or their metabolites from the body, mainly via the kidneys.
Route | Description | Examples |
Renal (urine) | Primary route via kidneys | Most drugs and metabolites |
Biliary (feces) | Excretion via bile into the intestines | Some drugs are excreted unchanged |
Pulmonary (breath) | Exhalation of volatile drugs | Inhaled anesthetics |
Others (sweat, saliva, breast milk) | Minor routes | Depends on drug properties |
Pharmacodynamics
Pharmacodynamics involves the study of the effects of drugs on the body, including mechanisms of action, dose-response relationships, and therapeutic outcomes.
Term | Definition | Examples |
Mechanism of Action | How a drug produces its effects | Inhibition of enzymes, receptor binding |
Dose-Response Relationship | Relationship between dose and effect | Higher doses generally lead to greater effects |
Therapeutic Index | Ratio of toxic dose to therapeutic dose | A higher index indicates a safer drug |
Side Effects | Unintended drug effects at therapeutic doses | Nausea, drowsiness |
Toxicity | Harmful effects from excessive dosing | Overdose leading to organ damage |
Adverse Drug Reactions (ADRs) | Harmful reactions to normal doses | Allergic reactions, anaphylaxis |
Application of Pharmacology to Midwifery Nursing and Patient Education
Pharmacological knowledge is important for safe and effective patient care and education. The nursing process provides a framework for applying this knowledge.
Pre-administration Assessment
The pre-administration assessment aims to:
1. Establish Goals:
- Collect baseline data to evaluate both therapeutic and adverse responses. This requires understanding the medication’s intended effects and potential side effects.
- Identify high-risk patients based on factors like age, renal/hepatic function, genetic predispositions, allergies, pregnancy, and concurrent medications.
- Assess the patient’s capacity for self-care, including understanding, dexterity(ability to use hands), and cognitive abilities.
2. Collecting Baseline Data: Gathering data (vital signs, lab results, symptom assessment) before medication administration establishes a benchmark to measure therapeutic effectiveness and detect adverse effects.
3. Identifying High-Risk Patients: This involves recognizing predisposing factors such as:
- Pathophysiology: Compromised liver or kidney function significantly impacts drug metabolism and excretion.
- Genetic Factors: Genetic polymorphisms can alter drug metabolism and response.
- Drug Allergies: A history of allergic reactions necessitates careful medication selection.
- Pregnancy: Pregnancy alters physiology, impacting drug absorption, distribution, metabolism, and excretion. Fetal safety must be prioritized.
- Age: Both very young and older adults often require dosage adjustments due to differences in organ function.
- Comorbidities and Concurrent Medications: Interactions between multiple medications or underlying health conditions significantly impact drug response.
4. Tools for identification include patient history, physical examination, and laboratory tests. Knowledge of potential drug interactions is crucial.
Implementing the Medication Order
A. Making PRN Decisions: A PRN (pro re nata, “as needed”) order requires the nurse to exercise clinical judgement regarding the timing and dosage based on the patient’s needs and assessment. The rationale for medication use must be clearly understood.
B. Managing Toxicity: Early recognition and management of drug toxicity are very key. Nurses must be familiar with the early signs of toxicity for each medication and the appropriate intervention protocols.
Application of Pharmacology in Patient Education
Patient education is paramount for safe and effective drug therapy. Essential information includes:
- Drug Name and Therapeutic Category: Include both generic and trade names.
- Dosage Size and Schedule: Clear instructions on how much to take and when.
- Route and Technique of Administration: Detailed instructions on how to administer the medication (oral, injection, topical, etc.).
- Duration of Treatment: Specify the length of therapy.
- Method of Drug Storage: Instructions on proper storage to maintain drug efficacy and safety (e.g., refrigeration, protection from light).
- Expected Therapeutic Response and Onset: Explain the expected benefits and when they should appear.
- Non-drug Measures: Discuss complementary therapies or lifestyle modifications that can enhance treatment.
- Symptoms of Major Adverse Effects: Educate patients on recognizing and reporting adverse effects. Include strategies for minimizing discomfort or harm.
- Major Adverse Drug-Drug and Drug-Food Interactions: Explain potential interactions and precautions to take.
- Contact Information: Provide contact information for reporting adverse effects or treatment concerns.
Application of the Nursing Process in Drug Therapy
The nursing process provides a systematic approach to medication administration and patient care:
A. Review of the Nursing Process:
- Assessment: Data collection via interview, medical history, physical exam, observation, and laboratory tests.
- Analysis/Nursing Diagnosis: Identifying actual and potential health problems related to medication therapy. This includes judging the appropriateness of the prescribed regimen, identifying potential drug-induced problems, and assessing the patient’s capacity for self-care.
- Planning: Defining goals, setting priorities, and identifying interventions to maximize therapeutic effects and minimize adverse effects.
- Implementation (Intervention): Carrying out the planned interventions, including medication administration and patient education. This includes both independent (nurse-initiated) and collaborative (physician-ordered) interventions.
- Evaluation: Determining the effectiveness of the interventions by analyzing data collected during implementation. This guides adjustments to the care plan as needed.
B. Applying the Nursing Process in Drug Therapy:
1. Pre-administration Assessment: This section summarizes essential information needed before administering a drug. It includes:
- Patient History: Reviewing allergies, current medications (prescription and over-the-counter), relevant medical history (renal/hepatic function, etc.), and any potential drug interactions.
- Baseline Data: Obtaining vital signs, relevant lab results, and other pertinent assessment data to establish a benchmark against which to measure therapeutic and adverse effects.
- Patient Understanding: Assessing the patient’s understanding of the medication, their ability to self-administer, and their overall capacity for adherence to the treatment regimen.
2. Implementation:
Administration: This section outlines the safe and effective administration of the medication, including:
- Routes of Administration: Describing appropriate routes (oral, intravenous, intramuscular, subcutaneous, topical, etc.) and any specific techniques for each.
- Dosage and Adjustment Guidelines: Summarizing appropriate dosage ranges, factors influencing dosage adjustments (e.g., age, renal function), and any special instructions for dose titration.
- Special Considerations: Highlighting any unique considerations during administration (e.g., rate of infusion, injection site selection, monitoring for adverse effects during administration).
Enhancing Therapeutic Effects: This section focuses on strategies to optimize the medication’s therapeutic effect, including:
- Dietary Modifications: Describing any necessary dietary changes to enhance drug absorption or minimize interactions (e.g., taking medication with food or avoiding certain foods).
- Comfort Measures: Identifying strategies to improve patient comfort and adherence (e.g., managing side effects with antiemetics or analgesics).
- Adherence Strategies: Outlining methods to promote adherence, such as medication reminders, pill organizers, or support systems.
3. Ongoing Evaluation and Intervention: This section outlines the ongoing monitoring and management of both therapeutic and adverse responses to the medication.
- a. Monitoring: Summarizes physiological and psychological parameters requiring monitoring to detect both therapeutic and adverse responses. This includes regular vital signs, lab tests (as appropriate), and ongoing assessments of the patient’s subjective experience.
- b. Evaluating Therapeutic Effects: Describes the criteria and procedures for evaluating the effectiveness of the medication in achieving its intended therapeutic goal. This should include specific, measurable outcomes.
- c. Minimizing Adverse Effects: Summarizes major adverse reactions that should be monitored for and outlines appropriate interventions to minimize harm. This could include both pharmacological and non-pharmacological interventions.
- d. Minimizing Adverse Interactions: Summarizes potential drug-drug and drug-food interactions and provides interventions to mitigate the risks.
- e. Managing Toxicity: Describes the major symptoms of drug toxicity and the appropriate treatment protocols. This section is crucial for early recognition and intervention to prevent serious complications.
4. Patient Education: This section summarizes essential information to be provided to the patient to promote safe and effective use of the medication. It should include:
- Medication Name and Purpose: Clearly explaining both the generic and brand name, along with its intended therapeutic use.
- Dosage, Route, and Schedule: Providing clear and concise instructions for medication administration.
- Expected Therapeutic Effects and Onset: Informing the patient what to expect and when to expect it.
- Common Side Effects and Management Strategies: Educating the patient on potential side effects and how to manage them safely.
- Adverse Reactions Requiring Immediate Attention: Clearly outlining warning signs and symptoms requiring immediate medical attention.
- Medication Storage and Disposal: Instructing the patient on the proper storage and disposal methods.
- Follow-up Care: Instructing the patient on any scheduled follow-up appointments or tests.