Table of Contents
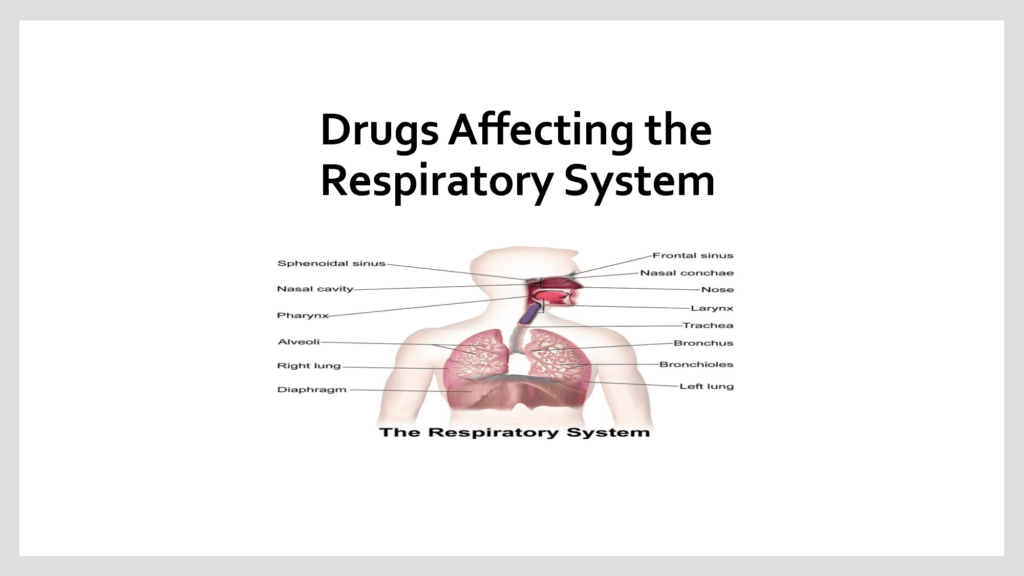
ToggleDrugs Acting on the Respiratory System
Drugs used in the treatment of respiratory tract disorders include:
- Drugs for Asthma
- Drugs for Allergic Rhinitis
- Drugs for Cough
- Drugs for Common Cold and Flu
Drugs Used in the Treatment of Asthma
Asthma is a chronic disease of the airways characterized by inflammation and reversible bronchospasm. It is associated with symptoms such as wheezing, breathlessness, chest tightness, and cough. Drugs used in the treatment of asthma are broadly divided into two categories:
- Bronchodilators
- Anti-inflammatory drugs
Table 1: Classification of Anti-Asthmatic Drugs
Class | Examples |
Bronchodilators | Beta2 agonists, Xanthine derivatives, Anticholinergics |
Anti-inflammatory drugs | Corticosteroids, Mast cell stabilizers, Leukotriene receptor antagonists |
Beta2 Agonists
Beta2 agonists promote bronchodilation by stimulating beta2 receptors in bronchial smooth muscles. They are further divided into short-acting and long-acting beta2 agonists.
- Short-acting beta2 agonists such as salbutamol and terbutaline have a rapid onset and short duration of action. They are recommended for the treatment of acute asthma attacks.
- Long-acting beta2 agonists such as salmeterol and formoterol have a delayed onset and long duration of action. These drugs are usually combined with inhaled corticosteroids such as budesonide for the long-term control of chronic asthma.
Salbutamol
Available Preparations:
- Inhaler: 100 mcg
- Nebulized solution: 5 mg/ml
- Syrup: 2 mg/5 ml
- Tablets: 4 mg
Available Brands: Ventolin®, Vental®, Kamvent®
Pharmacokinetics: Salbutamol is readily absorbed from the gastrointestinal tract, metabolized in the liver, rapidly excreted in the urine as metabolites and as unchanged drug, and a small amount is excreted in the feces.
Indications:
- Prophylaxis and treatment of asthma
- Chronic obstructive pulmonary disease
- Arrest premature labor
Contraindications:
- Hypersensitivity to salbutamol
- Eclampsia and severe preeclampsia
Dosage:
Oral:
Adults: 4 mg 3-4 times daily, max single dose 8 mg
Children:
- 7-12 years: 2 mg 3-4 times daily
- 2-6 years: 1-2 mg 3-4 times daily
- 1 month-2 years: 100 mcg/kg 3-4 times daily
Aerosol Inhalation:
- Adults: 100-200 mcg (1-2 puffs, for persistent symptoms up to 4 times daily)
- Children: 100 mcg (1 puff), increased to 200 mcg (2 puffs) if necessary, for persistent symptoms up to 4 times daily
Nebulized Solution:
- Children: > 2 years: 2.5-5 mg, repeat 3-4 times daily as necessary
- Children: < 2 years: 0.1 mg/kg up to 2.5 mg, repeat 3-4 times daily
Prophylaxis in Exercise-Induced Bronchospasm:
- Adults: 200-400 mcg (2 puffs)
- Children: 100-200 mcg up to 4 times daily
Side Effects:
- Tachycardia
- Arrhythmias
- Nervousness
- Angioedema
- Fine tremor, especially of hands
- Hypersensitivity reactions
- Palpitations
- Insomnia
- Muscle cramps
- Headache
Drug Interactions:
- Diuretics or digoxin: risk of cardiac arrhythmias is increased
- Corticosteroids: risk of hypokalemia and hyperglycemia is increased
Key Issues to Note:
- Salbutamol may delay labor in pregnant mothers near term
- Patients should swallow tablets whole with a glass of water
- Do not administer salbutamol within 1 hour of ingesting antacids, milk, or dairy products
- Salbutamide is habit-forming; therefore, long-term use may result in laxative dependency and loss of normal bowel function
- Onset of action is 6-12 hours for tablets, 15-60 minutes for suppository
- Warn the patient that prolonged use of salbutamol suppositories may cause proctitis
Xanthines
Xanthines include:
- Aminophylline
- Theophylline
They act by relaxing bronchial smooth muscle by inhibiting phosphodiesterase, the enzyme which breaks down cyclic AMP. Aminophylline is usually preferred to theophylline when greater solubility in water is required, particularly in intravenous formulations.
Aminophylline
Available Preparations:
- Tablets: 100 mg
- Injection: 250 mg/10 ml
Indications:
- Acute severe asthma
- Reversible airway obstruction
- Relieve apnea in neonates
- Nocturnal asthma
Contraindications:
- Porphyria
- Known hypersensitivity to aminophylline
Dosage:
Chronic Asthma:
- Oral: 100-200 mg 3-4 times daily, after food
Acute Severe Asthma (not treated with theophylline before):
Adults: IV loading dose 5-6 mg/kg slowly over 20-30 min diluted in normal saline or dextrose 5%
Maintenance: IV infusion 0.5 mg/kg/hour
Children: IV loading dose 4-6 mg/kg slowly over 20-30 min suitably diluted and 1.5-2.5 mg per kg in those using oral theophylline
Maintenance: By IV infusion
- 6 months-9 years: 1 mg/kg/hour
- 10-16 years: 0.8 mg/kg/hour
Side Effects:
- Restlessness
- Anxiety
- Palpitations
- Insomnia
- Convulsions
- Urticaria
- Gastrointestinal irritation
- Hypotension, especially if given by rapid injection
- Tremor
- Headache
- Dizziness
- Arrhythmias
- Epigastric pain
Drug Interactions:
- Beta blockers: may decrease the effects of aminophylline
- Cimetidine, ciprofloxacin, erythromycin, norfloxacin: may increase aminophylline blood concentration and risk of aminophylline toxicity
- Phenytoin, rifampicin, carbamazepine: may increase aminophylline metabolism
- Smoking: may decrease aminophylline blood concentration
- Caffeine: may intensify the adverse effects of aminophylline on the CNS and heart
Key Issues to Note:
- Rapid IV injection should be avoided as it may result in hypotension, seizures, and arrhythmias (less than 20-25 mg/min) is required
- Patients taking oral aminophylline should not receive intravenous aminophylline unless plasma concentration is available to guide dosage
- Patients should avoid caffeine-containing beverages and other sources of caffeine
Corticosteroids
Corticosteroids may be given parenterally, orally, or as inhalers. Inhaled corticosteroids include:
- Beclomethasone
- Budesonide
- Fluticasone
These drugs are the most effective in the treatment of chronic asthma. Corticosteroids reduce bronchial mucosal inflammation and bronchial hyper-reactivity. They are recommended for the prophylaxis of asthma in patients who have not responded to beta2 agonists or if symptoms disturb sleep more than once a week. Corticosteroid inhalers must be used regularly for effective control of symptoms. Alleviation of symptoms usually occurs after 7 days of initiating treatment.
Beclomethasone
Available Preparations:
- Metered Inhaler: 50 mcg
Available Brands: Becotide®, Beclate®
Indications:
- Prophylaxis of asthma
Contraindications:
- Status asthmaticus
- Hypersensitivity to beclomethasone
- Acute infections uncontrolled by antimicrobial chemotherapy
Dosage:
- Adults: 200 mcg twice daily or 100 mcg 3-4 times daily
- Children: 50-100 mcg 2-4 times daily or 100 mcg twice daily
Side Effects:
- Oropharyngeal candidiasis
- Hoarseness
- Paradoxical bronchospasm
- Adrenal suppression
- Impaired bone metabolism
- Glaucoma and cataracts
Systemic Corticosteroids
These drugs are given either orally or by injection. Examples include:
- Prednisolone/Prednisone
- Betamethasone
- Triamcinolone
- Hydrocortisone
- Dexamethasone
- Methylprednisolone
Table 2: Characteristics of Corticosteroids
Class | Examples |
Short-acting | Hydrocortisone |
Intermediate-acting | Prednisolone, Prednisone, Methylprednisolone, Triamcinolone |
Long-acting | Dexamethasone, Betamethasone |
Prednisolone
Available Preparations:
- Tablets: 5 mg
Available Brands: Kampred®
Indications:
- Bronchial asthma
- Cerebral edema
- Allergic reactions
- Acute leukemia
- Rheumatic disease
- Inflammatory bowel disease
- Suppression of inflammatory reactions
- Acute or chronic adrenal insufficiency
Contraindications:
- Systemic infection (unless life-threatening)
- Avoid live virus vaccines
- Hypersensitivity to prednisolone
Dosage:
- Initially: 10-20 mg daily (up to 60 mg in severe diseases) preferably taken in the morning after breakfast, and often be reduced within a few days but may need to be continued for several weeks or months
- Maintenance: 2.5-15 mg daily but higher doses may be needed
- Children:
- 1-6 years: 5 mg daily up to 15 mg in severe cases
- 7-12 years: 5-10 mg daily up to 30 mg in severe cases
Side Effects:
- Dyspepsia
- Osteoporosis
- Glaucoma
- Skin atrophy
- Weight gain
- Menstrual irregularities
- Peptic ulcer
- Increased appetite
- Acne
- Adrenal suppression
- Striae
Drug Interactions:
- Prednisolone may decrease the effect of diuretics, insulin, oral antidiabetics, and potassium supplements
- Prednisolone may increase the risk of digoxin toxicity caused by hypokalemia
- Prednisolone may decrease the patient’s antibody response to vaccines
Key Issues to Note:
- Take the drug after meals, with food or milk to decrease GI upset
- Advise the patient to avoid alcohol, limit caffeine
- Advise the patient not to decrease the dose or discontinue without doctor’s approval
Dexamethasone
Available Preparations:
- Tablets: 0.5 mg
- Injection: 4 mg/ml
Available Brands: Dexona®
Pharmacokinetics: Dexamethasone is readily absorbed from the gastrointestinal tract, crosses the placenta with minimal inactivation, and is excreted in urine within 24 hours.
Indications:
- Cerebral edema
- Rheumatic diseases
- Anaphylaxis
- Septic shock
- Nausea and vomiting due to anti-cancer drugs
- Bacterial meningitis (in combination with antibiotics)
- Acute exacerbation of chronic allergic disorders
Contraindications:
- Hypersensitivity to dexamethasone
- Systemic infections
- Avoid live virus vaccines
Dosage:
Oral:
- Adults: 0.5-2 mg daily but higher doses may be required depending on the severity of the condition
- Children: 100-1000 mcg/kg daily in 1-2 divided doses
Injection:
- Adults: 1M or slow IV or infusion: 0.5-24 mg daily
- Children: 200-400 mcg/kg daily in 1-2 divided doses
Cerebral Edema Associated with Malignancy:
- IV injection (as dexamethasone phosphate): initially 10 mg then 4 mg by IM every 6 hours for 2-4 days gradually reduced and stopped over 5-7 days
- Children: IV 0.25 mg/kg/day in divided doses for up to 2 days then gradually taper down over the next 5 days
Side Effects:
- Hypertension
- Hyperglycemia
- Edema
- Glaucoma
- Weight gain
- Growth suppression in children
- Increased appetite
- Muscle atrophy
- Cataracts
- Peptic ulcer
- Hypokalemia
Drug Interactions:
- Increased risk of hypokalemia when used concurrently with amphotericin B or loop diuretics
- Concurrent use with aspirin may lead to increased gastrointestinal tract side effects
Key Issues to Note:
- Administer the drug with food or milk to minimize GI side effects
- Advise the patient to avoid alcohol and limit caffeine intake
- Advise the patient to avoid exposure to measles or chickenpox
- Inform the patient not to decrease the dose or stop treatment without doctor’s recommendation
Hydrocortisone
Available Preparations:
- Injection: 100 mg
Available Brands: Cardilan®, Primacort®, Stricort®
Indications:
- Hypersensitivity reactions including anaphylaxis
- Inflammatory bowel disease
- Asthmatic attack
- Hemorrhoids
- Rheumatic diseases
- Adrenocortical insufficiency
- Angioedema
Contraindications:
- Systemic infections
- Avoid live virus vaccines in those receiving immunosuppressive doses
- Hypersensitivity to hydrocortisone
Dosage:
Anaphylaxis; Acute Severe Asthma and Shock:
IV slow IV injection or infusion:
Adults: 100-500 mg 3-4 times daily
Children:
- 6-12 years: 100 mg 3-4 times daily
- 1-5 years: 50 mg 3-4 times daily
- Up to 1 year: 25 mg 3-4 times daily
Side Effects:
- Dyspepsia
- Adrenal suppression
- Weight gain
- Glaucoma
- Nausea
- Peptic ulceration
- Menstrual irregularities
- Increased appetite
- Acne
- Malaise
Drug Interactions:
- Anti-convulsants, rifampicin: reduce the effectiveness of hydrocortisone
- Hydrocortisone: reduces the action of antidiabetic drugs
- Hydrocortisone: reduces the effect of antihypertensive drugs
- Hydrocortisone: may decrease the patient’s antibody response to vaccines, increase vaccine side effects, and potentiate virus replication when given with live virus vaccine
Leukotriene Receptor Antagonists
This class includes:
- Zafirlukast
- Montelukast
These drugs act by suppressing the effects of leukotrienes, compounds that promote bronchoconstriction as well as eosinophil infiltration, mucus production, and airway edema.
Zafirlukast
Available Preparations:
- Tablets: 20 mg
Available Brands: Accolate®
Pharmacokinetics: Zafirlukast is rapidly absorbed after oral administration, extensively metabolized in the liver, and excreted in feces.
Indications:
- Prophylaxis of asthma
- Exercise-induced asthma
Contraindications:
- Hypersensitivity to zafirlukast
- Breastfeeding
- Hepatic impairment
Dosage:
- Adults: 20 mg twice daily at least 1 hour before or 2 hours after meals
- Children under 12 years: Not recommended
Side Effects:
- Headache
- Diarrhea
- Insomnia
- Dyspepsia
- Dizziness
- Nausea
- Fever
- Malaise
- Vomiting
- Abdominal pain
Drug Interactions:
- Blood levels are increased by aspirin
- Blood levels are decreased by erythromycin and theophylline
- Zafirlukast increases the effects and risk of bleeding with warfarin
Key Issues to Note:
- Give the drug at least 1 hour before or 2 hours after a meal
- Advise the patient to take the drug as prescribed even during symptom-free periods
- Do not use the drug to treat acute episodes of asthma
- Advise the patient not to decrease the dose or stop unless instructed by the doctor
- Nursing women should not take zafirlukast
- Inform the patient to report symptoms such as abdominal pain, nausea, fatigue, itching, or anorexia
Drugs for Allergic Rhinitis
Rhinitis is an inflammation of the nasal mucous membrane and is characterized by periods of nasal discharge, sneezing, and nasal congestion.
Rhinitis may be allergic or non-allergic in origin.
Allergic Rhinitis
Allergic rhinitis is defined as a nasal mucous membrane inflammation caused by a hypersensitivity response to foreign allergens mediated by IgE antibodies.
Drugs used in the treatment of allergic rhinitis include:
- Antihistamines
- Decongestants
- Corticosteroids
- Mast cell stabilizers
Antihistamines
Antihistamines are the mainstay in the treatment of seasonal and perennial allergic rhinitis. They relieve symptoms such as rhinorrhea, edema, nasal itching, sneezing, and ocular symptoms such as conjunctivitis. They are more effective when taken before the start of symptoms.
Classification of Antihistamines
Antihistamines are classified as follows:
- Sedating antihistamines
- Non-sedating antihistamines
Sedating Antihistamines
They are also called first-generation antihistamines. Sedating antihistamines cross the blood-brain barrier and are associated with marked sedation and depression.
Examples:
- Chlorpheniramine
- Hydroxyzine
- Promethazine
- Cyproheptadine
Chlorpheniramine
Available Preparations:
- Tablets: 4 mg
- Syrup: 2 mg/5 ml
Available Brands: Piriton®, Piton®
Pharmacokinetics: Chlorpheniramine is well absorbed following oral administration, distributed to body tissues, including the placenta. It is metabolized in the liver and excreted in urine.
Indications:
- Conjunctivitis
- Allergic rhinitis
- Pruritus of allergic origin
- Acute urticaria
- Insect stings
- Severe angioedema
Contraindications:
- Hypersensitivity to chlorpheniramine
- Acute attack of asthma
- Third trimester of pregnancy
- Breastfeeding
- Narrow-angle glaucoma
Dosage:
Adults and Children over 12 years: 4 mg every 4-6 hours
Children:
- 6-12 years: 2 mg every 4-6 hours
- 1-5 years: 1 mg 3 times daily
- 6 months-12 months: 1 mg twice daily
Side Effects:
- Drowsiness
- Dizziness
- Epigastric pain
- Headache
- Palpitations
- CNS depression
- Urinary retention
- Dry mouth
- Blurred vision
- Sweating
- Tremor
Drug Interactions:
- Chlorpheniramine potentiates sedative effects of barbiturates, hypnotics, opioid analgesics
- Increased sedative effects with alcohol
Key Issues to Note:
- Advise the patient to take the drug after food to minimize GI distress
- Inform the patient that chlorpheniramine may cause drowsiness and impair the ability to perform activities requiring mental alertness
- Advise the patient to avoid direct exposure to sunlight since it may cause severe sunburn
- Avoid alcohol while taking chlorpheniramine
Non-Sedating Antihistamines
Non-sedating antihistamines are less sedating than the first generation.
Examples:
- Cetirizine
- Loratadine
- Desloratadine
- Levocetirizine
- Ebastine
Cetirizine
Available Preparations:
- Tablets: 10 mg
- Syrup: 5 mg/5 ml
Available Brands: Zyrtec®, Finallergy®, Zyncet®, Allercet®, Alerid®
Pharmacokinetics: Cetirizine is rapidly and almost completely absorbed from the GIT, undergoes slow first-pass metabolism, and is excreted in urine primarily as unchanged drug.
Indications:
Symptomatic relief of allergy such as:
- Allergic rhinitis
- Allergic conjunctivitis
- Atopic dermatitis
- Chronic urticaria
Contraindications:
- Hypersensitivity to cetirizine
- Breastfeeding
- Pregnancy
- Acute attacks of asthma
Dosage:
Adults and Children over 6 years: 10 mg daily or 5 mg twice daily
Children:
- 2-5 years: 2.5 mg once daily or 2.5 mg twice daily
- 6 months-1 year: 2.5 mg once daily
Side Effects:
- Somnolence
- Insomnia
- Headache
- Dizziness
- Dry mouth
- Abdominal pain
- Nausea and vomiting
- Diarrhea
- Bronchospasm
- Pharyngitis
- Malaise
Drug Interactions:
- Alcohol and other CNS depressants may increase CNS depression
Key Issues to Note:
- The drug can be given without regard to food
- Cetirizine may cause drowsiness and impair the ability to perform activities requiring mental alertness
- Cetirizine may cause dry mouth; therefore, advise the patient to drink a lot or to use sugarless gum
- Avoid alcohol while taking cetirizine
Drugs Used in the Treatment of Cough
Cough is a useful natural response to irritation of the lungs and airways aimed at removing foreign substances or excessive secretions.
Cough may occur as a symptom of an underlying disorder such as asthma, pneumonia, sinusitis, or gastroesophageal reflux disease.
It may be classified as follows:
- Non-productive cough
- Productive cough
Productive Cough
Productive cough is characterized by the presence of sputum and may be associated with conditions such as chronic bronchitis, asthma, and pneumonia. It is commonly treated with cough expectorants or mucolytics.
Non-Productive Cough
This type of cough is associated with no mucus production and is regarded as a useless cough. It is commonly associated with the common cold and is treated with cough suppressants or antitussives.
Cough Expectorants
Cough expectorants facilitate the expulsion of mucus and other materials from the lungs. Cough expectorants contain one or more of the following:
- Guaifenesin
- Ammonium chloride
- Ipecacuanha
- Squill
- Volatile oils
- Guaiacol
- Iodides
- Sodium citrate
- Creosote
Preparations which contain cough expectorants include:
- Cadistin syrup®
- Cadiphen syrup®
- Histalin syrup®
- Hydrylin syrup®
- Delased chesty®
- Actified expectorant®
- Menthodex syrup®
- Zecuf herbal syrup®
Mucolytic Expectorants
Mucolytics reduce the viscosity of bronchial secretions by breaking down the structure of tenacious sputum, thereby facilitating its removal by coughing. Mucolytics are often used in chronic bronchitis and chronic asthma where sputum production is high.
Examples:
- Bromhexine
- Carbocisteine
- Ambroxol
Common compound preparations containing mucolytics include:
- Rhinathiol syrup®
- Brozedex®
- Ascoril®
- Bisolvin®
- Ambrodil®
Demulcents
Demulcent cough preparations coat the mucosa of the pharynx and provide short-lived relief of the irritation that provokes the cough reflex. They contain soothing substances such as:
- Glycerol
- Honey
- Liquorice
- Sucrose syrup
Compound preparations containing demulcents include:
- Simple linctus
- Menthodex lozenges
- Zecuf lozenges
Cough Suppressants
Cough suppressants act centrally to reduce the sensitivity of the cough center. They should be avoided in chronic obstructive airway diseases as they may also depress respiration. Most cough suppressants are opiate derivatives and may cause constipation and abuse. They should be avoided in children below one year.
Examples include codeine, pholcodine, and dextromethorphan; the latter two generally have fewer adverse effects than codeine.
Compound preparations containing cough suppressants include: Benylin with codeine®, Benylin DM®, Rhinathiol dry cough®, Piritex with codeine®, Hydryllin DM®, Piritex Junior®, Actifed syrup®, Delased dry cough®, and Zedex®.