Table of Contents
ToggleClassifications of Drugs
A drug is any substance that, when introduced into a living organism, alters its structure or function. This includes anything from medications used to treat illnesses to recreational substances. Drugs are used for various reasons:
- Treatment: To cure or manage diseases and health conditions.
- Prevention: To protect against illnesses (e.g., vaccines).
- Diagnosis: To help identify medical conditions (e.g., contrast dyes used in medical imaging).
- Symptom Relief: To ease the discomfort associated with various ailments (e.g., pain relievers).
Drug Nomenclature: The Three Names of a Drug
Each drug typically has three names:
- Chemical Name: This is a complex, detailed description of the drug’s precise chemical structure and composition. It’s very long and complicated, rarely used in everyday practice (e.g., (+/-)-2-(p-isobutylphenyl) propionic acid).
- Generic Name: This is the official, non–proprietary name assigned to a drug by a regulatory body like the FDA (Food and Drug Administration) or EMA (European Medicines Agency). It’s simpler than the chemical name and universally recognized (e.g., ibuprofen). Doctors commonly use generic names when prescribing, and pharmacists usually use this name when dispensing medication.
- Brand Name (Trade Name or Proprietary Name): This is the name under which the drug is marketed and sold by a specific pharmaceutical company. It is a copyrighted name and often includes a trademark symbol (®) (e.g., Brufen®, Advil®, Motrin® – all brand names for ibuprofen). Many different companies may produce the same drug, each with a different brand name.
Examples of Generic and Brand Names: Note that a single generic drug can have many different brand names. Similarly, some brand names may combine multiple active ingredients, while others may simply repackage an existing generic drug.
Generic Name | Brand Name(s) | Indication/Use |
Amoxicillin | Amoxil®, Duramox®, Amoxapen®, and many more | Antibiotic (treats bacterial infections) |
Ibuprofen | Brufen®, Advil®, Motrin®, Nurofen®, and many more | Pain reliever, anti-inflammatory |
Paracetamol | Panadol®, Tylenol®, Acetaminophen®, and many more | Pain reliever, fever reducer |
Propranolol | Inderal®, InnoPran XL®, and others | Treats high blood pressure, angina, and tremors |
Salbutamol | Ventolin®, Proventil®, and others | Bronchodilator (treats asthma and other lung conditions) |
Diazepam | Valium®, Diastat®, and others | Anti-anxiety medication, muscle relaxant |
Metformin | Glucophage®, Fortamet®, and others | Treats type 2 diabetes |
Lisinopril | Prinivil®, Zestril®, and others | Treats high blood pressure |
Atorvastatin | Lipitor®, and others | Reduces cholesterol levels |
Important Note: While brand-name and generic drugs contain the same active ingredient, there might be slight differences in inactive ingredients (fillers, binders). These differences usually don’t affect the drug’s efficacy, but some individuals might experience minor differences in how the medication affects them. This is usually not clinically significant, but it’s important to be aware of.
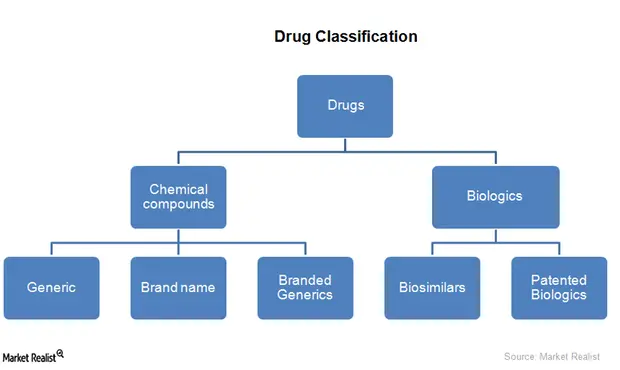
Drug Classification
Drugs can be categorized in several ways, each serving a specific purpose in understanding their use, regulation, and pharmacological properties. The primary classifications include:
- Prescription Classification
- Pharmacological Classification
- Legal Classification
Prescription Classification
This classification system divides drugs based on whether they require a prescription from a healthcare provider or can be obtained over the counter.These need a doctor’s prescription because they’re powerful, can have serious side effects if misused, or are easily abused.
Prescription-Only Medicines (POM):
These drugs necessitate a prescription due to their potential for harm if misused or self-administered. Examples include:
- Antibiotics: Amoxicillin (treats bacterial infections), Ciprofloxacin (treats various bacterial infections), and others targeting specific bacterial strains. The choice of antibiotic depends heavily on the identified pathogen and its susceptibility.
- Analgesics: Diclofenac (a nonsteroidal anti-inflammatory drug, NSAID, for pain and inflammation). Other NSAIDs like ibuprofen and naproxen also fall into this category, differing in their mechanisms and side-effect profiles.
- Cardiovascular Medications: Nifedipine (a calcium channel blocker used to treat hypertension and angina). Numerous other cardiovascular drugs exist, targeting various aspects of the cardiovascular system, including blood pressure, heart rate, and cholesterol levels. Each drug has specific indications and contraindications.
- Antidepressants: Sertraline (Zoloft), Fluoxetine (Prozac). These treat depression and other mood disorders. They should only be taken under a doctor’s supervision due to potential side effects and the need for careful dose adjustment.
- Anti-anxiety Medications: Alprazolam (Xanax), Diazepam (Valium). These are used for anxiety and panic disorders, and can be habit-forming.
- Asthma Inhalers: Many inhalers containing corticosteroids or bronchodilators require a prescription to ensure appropriate use and monitoring for side effects.
- Diabetes Medications: Insulin (various types), Metformin. These require careful monitoring and adjustment by a doctor to maintain blood sugar levels within a safe range.
Over-the-Counter (OTC) Drugs:
These are considered safe for self-administration when used as directed. These are considered safe enough for you to buy without a prescription. They’re readily available in pharmacies and other retail outlets. Examples include:
Analgesics: Panadol® (paracetamol/acetaminophen), Hedex® (containing paracetamol and other ingredients). The specific formulation of OTC analgesics varies widely, influencing their effectiveness and potential side effects.
Vitamins and Minerals: Numerous vitamin and mineral supplements are sold OTC, but their efficacy and safety depend on factors like dosage, individual needs, and potential interactions with other medications or underlying health conditions.
Cough and Cold Remedies: Goodmorning syrup® (and similar products) containing ingredients intended to alleviate cough symptoms. It’s crucial to consider the specific active ingredients and potential interactions before use.
Antacids: Tums, Rolaids. These neutralize stomach acid for heartburn relief. Overuse can be problematic.
Antihistamines: Diphenhydramine (Benadryl), Cetirizine (Zyrtec). These relieve allergy symptoms. Some can cause drowsiness.
Laxatives: Many types exist for treating constipation. Overuse can lead to dependence.
Pharmacological Classification
This system categorizes drugs based on their mechanism of action or their effect on the body. This focuses on what the drug does in the body.
By Target Body System:
Drugs are grouped according to the organ system they primarily affect. Examples include:
- Cardiovascular Drugs: Affecting the heart and blood vessels (e.g., beta-blockers, ACE inhibitors, diuretics). Each class within cardiovascular drugs has specific actions and clinical applications.
- Neurological Drugs: Affecting the nervous system (e.g., antidepressants, antipsychotics, anticonvulsants). The choice of neurological medication is highly individualized based on diagnosis and patient response.
- Gastrointestinal Drugs: Affecting the digestive system (e.g., antacids, laxatives). Different gastrointestinal drugs target specific aspects of digestive function.
- Respiratory Drugs: Affecting the lungs and airways (e.g., bronchodilators, corticosteroids). Respiratory drugs are crucial in managing conditions like asthma and COPD.
By Activity on Microorganisms:
This is particularly important for antimicrobial drugs:
- Antibiotics: Targeting bacteria (e.g., penicillin, tetracycline, cephalosporins). Antibiotic classes differ in their mechanisms of action and spectrum of activity.
- Antivirals: Targeting viruses (e.g., acyclovir, oseltamivir). Antiviral drugs often have highly specific targets and mechanisms.
- Antifungals: Targeting fungi (e.g., fluconazole, ketoconazole). Antifungal drugs can have differing effects depending on the type of fungus being treated.
Legal Classification
Legal classification divides drugs into categories based on their potential for abuse and medical use. In otherwords, Drugs are classified based on their therapeutic use, abuse potential, and legal status.
Class A Drugs:
These include highly controlled substances such as:
- Morphine
- Pethidine
- Cocaine (Schedule I and II)
Class B Drugs:
These include a broader range of controlled substances such as:
- Phenobarbitone
- Ciprofloxacin
- Amoxicillin
- Diazepam
- Codeine
- Griseofulvin
- Metformin (Schedule 3, 4, and 5)
Class C Drugs:
These include over-the-counter drugs that are generally considered safe for public use without a prescription.
Class | Description | Examples |
Class A | High abuse potential, controlled substances | Morphine, pethidine |
Class B | Prescription required, lower abuse potential | Amoxicillin, antihypertensives |
Class C | Over-the-counter, safe for self-medication | Paracetamol, aspirin |
Schedule of Controlled Substances
Controlled substances are further categorized into schedules based on their potential for abuse and accepted medical uses. That is to say, this classification is based on the potential for abuse and the drug’s medical usefulness.
Schedule I Drugs (High Abuse Potential, No Accepted Medical Use): Heroin, lysergic acid diethylamide (LSD). These are typically subject to the strictest control measures.
- Examples: Heroin, Lysergide (LSD)
- Characteristics: High abuse potential and no currently accepted medical use.
Schedule II Drugs (High Abuse Potential, Accepted Medical Use): Morphine, codeine, pethidine (meperidine), methadone, cocaine. These drugs are tightly regulated, requiring specific prescribing protocols and record-keeping. Their use is generally reserved for situations where the benefits outweigh the substantial risks of addiction and misuse.
- Examples: Morphine, Codeine, Pethidine, Methadone, Cocaine
- Characteristics: High abuse potential but accepted medical uses. These drugs can lead to severe physical and psychological dependence.
Schedule III Drugs (Moderate Abuse Potential, Accepted Medical Use): Phenobarbitone, preparations containing limited quantities of opioids (e.g., codeine combined with paracetamol/acetaminophen – co-codamol). These have less stringent control measures than Schedule I and II drugs but still require careful monitoring.
- Examples: Phenobarbitone, preparations containing limited quantities of opioids, and combinations with non-controlled substances like Paracetamol with Codeine (Co-codamol)
- Characteristics: Less abuse potential than Schedule I and II drugs, with accepted medical uses.
Schedule IV Drugs (Low Abuse Potential, Accepted Medical Use): Diazepam, lorazepam (benzodiazepines). While considered less prone to abuse, these can still cause dependence with prolonged use.
- Examples: Diazepam, Lorazepam
- Characteristics: Lower abuse potential than Schedule I-III drugs, with accepted medical uses.
Schedule V Drugs (Lowest Abuse Potential, Accepted Medical Use): Drugs for cough or diarrhea containing limited quantities of opioid substances (e.g., loperamide in some formulations, piritex with codeine syrup, kaolin). These are often available with less stringent regulatory oversight than higher scheduled drugs.
- Examples: Drugs generally used for relief of cough or diarrhea, containing limited quantities of certain opioids like Loperamide, Kaolin, and Piritex with Codeine Syrup
- Characteristics: Lower abuse potential due to their low strength, with accepted medical uses.
Drug Administration
Drug administration refers to how drugs are delivered to patients.
Route | Description | Advantages | Disadvantages |
Enteral (Oral) | Taken by mouth | Convenient, safe | Slow onset, GI absorption variability |
Parenteral (IV, IM, SC) | Injections directly into the body | Rapid effect, precise control | Requires skill, painful, risk of infection |
Topical | Applied to skin or mucous membranes | Localized effect, non-invasive | Slow absorption, limited drug types |
Inhalational | Inhaled gases or aerosols | Quick relief for respiratory conditions | Requires technique, potential for irritation |
Prescription Writing and Dispensing
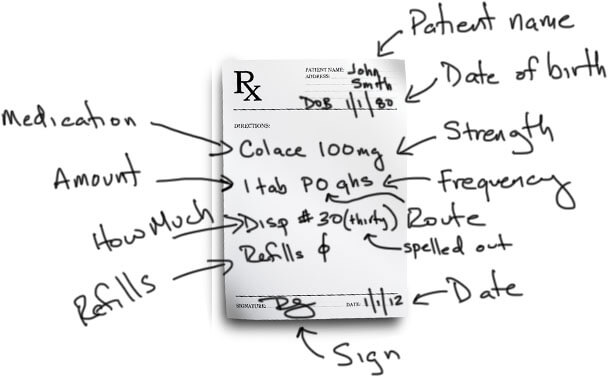
Prescription Writing
A prescription is a legal document—a written order from a licensed healthcare professional (doctor, nurse practitioner, physician assistant, etc.) to a pharmacist or other authorized dispenser, instructing them to provide a specific medication to a patient.
The prescriber has a legal and ethical responsibility to ensure the prescription is accurate, clear, and safe.
A good prescription must include the following essential information:
1. Legibility: Written clearly in indelible ink (permanent ink that won’t fade or smear).
2. Date: The date the prescription was written.
3. Patient Information: The patient’s full name and address. For children, their age and weight are crucial for accurate dosing.
4. Diagnosis: The medical reason for prescribing the medication. While not always explicitly stated on every prescription, this is medically critical information used to justify the treatment and assess the appropriateness of the drug.
5. Medication Details:
- Drug Name: The full name of the medication (generic name preferred for clarity).
- Dosage Form: Tablet, capsule, liquid, injection, etc.
- Strength: The amount of active ingredient per dosage unit (e.g., 500mg).
- Quantity: The total amount of medication to be dispensed.
- Duration: The length of treatment (e.g., “take for 7 days”).
- Frequency: How often the medication should be taken (e.g., “twice daily”).
6. Patient Instructions: Clear, concise directions on how to take the medication, including when to take it (with or without food, at bedtime, etc.).
7. Prescriber Information: The prescriber’s full name, address, and contact information (phone number, etc.).
8. Facility Information: The name and address of the healthcare facility where the prescription is written.
Qualities of a Good Prescriber
A good prescriber is knowledgeable, careful, and patient-centered. They:
- Prescribe Only When Necessary: Avoid unnecessary medication.
- Choose Appropriate Regimens: Select the most effective and safest treatment based on the patient’s specific condition and other health factors (allergies, other medications).
- Adjust Treatment as Needed: Monitor the patient’s response to treatment and adjust the dosage or medication as needed.
- Explain Treatment Clearly: Communicate effectively with the patient, explaining their condition, the medication’s purpose, potential side effects, and how to take it properly.
- Monitor Patient Progress: Follow up with the patient to assess their progress and make adjustments as needed.
The Rational Prescribing Process
Good prescribing follows a structured process:
- Define the Problem: Accurately diagnose the patient’s condition.
- Specify Therapeutic Objectives: Clearly define the desired outcome of treatment (e.g., pain relief, blood pressure control).
- Choose Appropriate Treatment: Select the most effective, safe, and well-tolerated medication, considering the patient’s overall health, potential drug interactions, and cost.
- Write an Accurate Prescription: Follow all the guidelines above.
- Inform the Patient: Educate the patient about their condition, treatment, and potential side effects.
- Review and Adjust Treatment: Regularly monitor the patient’s response and make changes as needed.
Over-Prescribing vs. Under-Prescribing: Both are problematic:
- Over-prescribing: Wastes resources, increases the risk of side effects and adverse drug reactions, and can lead to addiction and increased healthcare costs.
- Under-prescribing: Leads to ineffective treatment, potentially worsening the condition, delaying recovery, and ultimately increasing the cost of treatment over time due to the need for more extensive treatment down the road.
The Dispensing Process
Dispensing is the process of providing medication to the patient as directed by the prescription.
It’s performed by a licensed pharmacist or other authorized personnel (nurse, pharmacy technician).
Roles of a Dispenser
- Medication Dispensing: Accurately filling prescriptions.
- Patient Education: Providing medication information and instructions to patients.
- Record Keeping: Maintaining accurate drug records.
- Drug Storage: Ensuring proper storage conditions.
- Consultation with Prescriber: Advising prescribers on medication issues. (in some settings)
- Drug Procurement: Assisting with ordering drugs. (in some settings)
The Dispensing Procedure
- Receiving the Prescription: Checking for completeness and accuracy.
- Interpreting the Prescription: Understanding the instructions.
- Retrieving the Medication: Obtaining the correct medication from stock.
- Patient Counseling: Explaining how to take the medication and what to expect.
- Packaging: Ensuring the medication is properly packaged and labeled.
- Record Keeping: Documenting the dispensing process.
- Providing the Medication: Giving the medication to the patient.
Knowledge Required for Dispensing
Dispensers need comprehensive knowledge of:
- Drug formulations and dosages
- Indications and uses of medications
- Precautions and contraindications
- Potential side effects
- Packaging, labeling, and storage requirements
- Legal requirements for controlled substances
- Medication administration techniques
- Basic disease processes
Prescribing Medications
Prescribing involves selecting the appropriate drug, dose, route, and duration for treatment.
Consideration | Details |
Patient factors | Age, weight, sex, pregnancy status, organ function, allergies, comorbidities |
Drug factors | Efficacy, safety, side effects, interactions, cost |
Compliance | Ensuring patient understanding and adherence to the regimen |
Prescription Requirements:
A legal prescription must include patient details, drug information, and prescriber information.
Prescription Element | Description |
Patient Information | Name, age, address |
Drug Details | Name, strength, dosage, quantity, instructions |
Prescriber Information | Name, signature, registration number |
Abbreviations Used in Drug Administration
A wide range of abbreviations are used by doctors when making a prescription. These abbreviations are utilized to save time and space on prescriptions. They are categorized as follows:
1) Abbreviations Related to Frequency of Drug Administration
Abbreviation | Meaning |
OD | Once daily |
BID | Twice daily |
TDS | 3 Times daily |
QID | 4 Times daily |
PRN | When necessary |
Stat | Immediately |
Ac | Before meals |
Pc | After meals |
2) Abbreviations Related to Dosage Form
Abbreviation | Meaning |
Caps | Capsules |
Tabs | Tablets |
Syr | Syrup |
Gut | Eye drops |
Inf. | Infusion |
Pess. | Pessaries |
Mist | Mixture |
Iv | Intravenous |

common questions in pharmacology 1