Table of Contents
TogglePULMONARY TUBERCULOSIS
Pulmonary Tuberculosis is an infectious disease of the lungs caused by acid-fast bacilli known as Mycobacterium.
INCIDENCE:
The incidence ranges between 1% and 2% amongst the hospital deliveries in the tropics, being confined predominantly to the underprivileged sectors of society. Incidence of tuberculosis is rising worldwide with the rising prevalence of HIV infected patients. In 2000, WHO showed the emergence of multidrug resistant tuberculosis (MDR-TB) all over the world. It is a “global health emergency”.
Causes of Tuberculosis in Pregnancy:
TB is caused by the bacterium Mycobacterium tuberculosis. This bacteria spreads through the air when an infected person coughs, sneezes, talks, or sings, releasing tiny droplets containing the bacteria. When a healthy person inhales these droplets, the bacteria can enter the lungs and cause infection.
Incubation Period:
- The time between exposure to M. tuberculosis and the onset of symptoms is usually 4-6 weeks, but it can vary widely depending on individual factors.
Mode of Spread:
- Droplet Infection: The primary mode of transmission is through airborne droplets released when an infected person coughs, sneezes, talks, or sings. These droplets contain the bacteria, which can be inhaled by a healthy person.
- Sputum in Open Air Spaces: The presence of infected sputum in shared spaces can also facilitate transmission.
- Drinking Unpasteurized Milk: While less common, bovine tuberculosis can be transmitted through unpasteurized milk.
- Inhalation: Inhalation of contaminated dust containing M. tuberculosis can also lead to infection.
Types of Tubercle Bacterium:
- Human Tuberculosis: This is the most prevalent form of TB, primarily spread through person-to-person contact through droplet infection.
- Bovine Tuberculosis: This form is spread through infected animals, primarily cattle, and can be transmitted to humans through consumption of unpasteurized milk or contact with infected animals.
Types of Tuberculosis:
Pulmonary TB: This is the most common form of TB, affecting the lungs.
Signs & Symptoms:
- Persistent Cough: A cough that lasts for more than 3 weeks, often with the production of sputum.
- Sputum: Sputum may be purulent (containing pus), blood-stained (hemoptysis), or both.
- Evening Fevers: Fluctuations in body temperature, with fever typically occurring in the evening.
- Low-grade Fever and Malaise: Feeling unwell with a persistent low-grade fever and fatigue.
- Night Sweats: Excessive sweating during the night.
- Weight Loss: Significant and unexplained weight loss.
- General Lymphadenopathy: Swelling of lymph nodes throughout the body.
- Loss of Appetite: Decreased appetite and difficulty eating.
- Pleural Effusion: Fluid accumulation in the space between the lungs and the chest wall.
- Anemia and Massive Hemoptysis: Severe blood loss from the lungs, along with a decrease in red blood cells.
- Enlargement of Cervical Glands: Swelling of lymph nodes in the neck.
- Family History of Tuberculosis: Having a close family member with a history of TB increases the risk of infection.
- Amenorrhea: Absence of menstruation, particularly in women who are of reproductive age.
Extra Pulmonary TB: This form of TB affects organs other than the lungs. While less common than pulmonary TB, it can be serious and life-threatening.
Affected Areas:
- Meninges (Meningitis): Inflammation of the membranes surrounding the brain and spinal cord.
- Abdominal Pelvic Organs: Can affect the intestines, stomach, liver, and reproductive organs.
- Peritoneum: Inflammation of the membrane lining the abdominal cavity.
- Spine (Tuberculous Spondylitis): Infection of the vertebrae, often resulting in pain, stiffness, and deformity.
- Lymph Nodes: Swelling and inflammation of lymph nodes, particularly in the neck, armpits, and groin.
- Bones: Can affect bones throughout the body, leading to pain, swelling, and joint dysfunction.
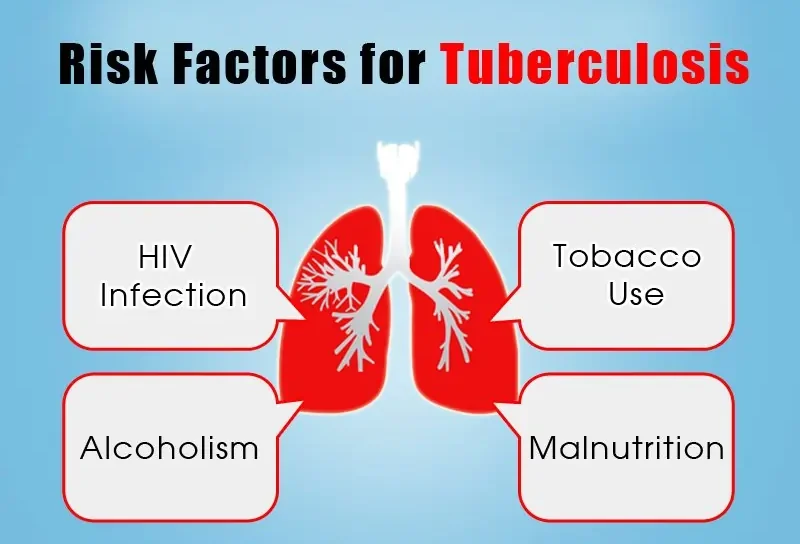
Risk Factors for Tuberculosis in Pregnancy:
- Pre-existing TB infection: A previous history of TB infection, even if treated, increases the risk of reactivation during pregnancy.
- Exposure to infected individuals: Living with or working closely with someone who has TB increases the risk of infection.
- Weakened Immune System: Pregnancy can temporarily suppress the immune system, making it easier for the TB bacteria to take hold and multiply.
- Malnutrition and Anaemia: Pregnant women who are malnourished or anaemic have a weaker immune system, making them more susceptible to TB infection.
- HIV Infection: HIV infection weakens the immune system significantly, increasing the risk of TB infection and making the disease more difficult to treat.
- Other Underlying Health Conditions: Conditions like diabetes, chronic kidney failure, and alcoholism can weaken the immune system and increase the risk of TB infection.
- Socioeconomic Factors: Poverty, overcrowding, poor sanitation, and inadequate access to healthcare can all contribute to the spread and development of TB.
- Environmental Factors: Exposure to dust, smoke, and other airborne irritants can irritate the lungs, making them more susceptible to TB infection.
Diagnosis of Tuberculosis in Pregnancy:
- Tuberculin Skin Test (TST): The TST involves injecting a small amount of purified protein derivative (PPD) under the skin. A positive reaction (induration ≥ 5 mm) indicates exposure to TB, especially in high-risk individuals (e.g., those with HIV).
- Chest X-ray: A chest X-ray can reveal abnormalities in the lungs consistent with TB infection. However, it is usually performed after 12 weeks of pregnancy to minimize potential risks to the fetus.
- Sputum Culture: Early morning sputum samples are collected for three consecutive days and examined for the presence of acid-fast bacilli (AFB), the hallmark of TB.
- Gastric Washings: For individuals who cannot produce sputum, gastric washings can be analyzed for AFB.
- Diagnostic Bronchoscopy: In some cases, a bronchoscopy, a procedure that allows for visualization of the airways, may be necessary to obtain tissue samples for diagnosis.
- Extrapulmonary TB Diagnosis: TB can affect other organs like lymph nodes and bones (although rare in pregnancy).
- Direct Amplification Tests: These tests, like PCR (polymerase chain reaction), amplify DNA specific to M. tuberculosis, allowing for sensitive and specific detection.
Investigations:
- Sputum examination will reveal the bacilli.
- Examination of aspirates for pleural effusion.
- Tuberculosis skin test (to show whether the patient has been in contact with tuberculosis bacilli).
- Biopsy, e.g., of lymph nodes.
- Serology for HIV.
- Blood smear for malaria parasites.
- Chest X-ray examination.
- Erythrocyte sedimentation rate (ESR).
- Haemoglobin (HB).
- Urinalysis.
- Stool examination.
Management in Maternal/Child (M/C) Care:
Aims:
- Health education about the disease.
- Promote healing.
Procedure when a Mother Comes:
- Create a nurse-patient relationship and take history (family, social, medical, and obstetrical).
- Observations: Take TPR (temperature, pulse, respiration) and BP (blood pressure).
- Conduct general and abdominal examinations.
- Reassure the mother, document all findings, and refer her to a hospital.
In Hospital: During Pregnancy:
- If sputum is negative, she can be treated as an outpatient before delivery, under the care of a physician and obstetrician.
- She should visit ANC (Antenatal Care) regularly.
- If she is infectious, she should be admitted to an isolation room.
- Histories and observations (BP, TPR) are taken.
- General and abdominal examinations are done, and the doctor is informed.
- Prepare an examination tray for taking specimens for observations.
- When the doctor comes, he examines the patient.
Medical Treatment: New Cases:
- 2EHRZ 6EH
- Ethambutol (E) 25mg/kg.
- Isoniazid (H) 300mg.
- Rifampicin (R): <50kg: 450mg; ≥50kg: 600mg.
- Pyrazinamide (Z): <50kg: 1.5g; ≥50kg: 2.0g.
Other Treatment for TB:
- Relapse: Patients treated before, who had initial care but the disease reoccurred later.
- Defaulters: Patients who stop treatment regardless of the reason.
- Treatment: 2SE (HR) Z/IE (HR) Z/5EHR. Streptomycin 60 injections dose 0.75g (not given in pregnancy due to side effects).
Failures: Patients with positive sputum 2 months after starting treatment.
- Treatment: 2 months SE (HR) Z/E (HR) 5 months SE (HR).
Side Effects of Drugs:
- Some other drugs: pyridoxine, prednisone for TB meningitis, codeine phosphate to reduce the rate of spread of infectious bacteria.
- All patients must be counseled before starting treatment to ensure understanding of the number of drugs, duration of treatment, and expected side effects.
Nursing Care:
- Isolation room should be ventilated.
- Diet: Plenty of protein and fluids; intake and output should be well recorded.
- Rest and sleep: Important during day and night, with occupational therapy.
- Hygiene: Daily bath, oral hygiene, spitting in a sputum mug (emptied and disinfected regularly), using disposable handkerchiefs that should be burned, changing and disinfecting bed sheets.
- Exercise: Teach deep breathing to expand the lungs.
- Position: Sitting up if dyspneic.
- Observations: Take T, R, P, and BP; assess general condition and fetal well-being twice a week.
- Bowel and bladder: Encourage regular bowel and bladder function.
- Reassurance: Provide support and encouragement to the mother.
During Labour: Problems May Include:
- Fatigue
- Reduced lung function
Doctor’s Case:
- Inform the doctor, physician, obstetrician, and paediatrician once labour starts.
- Manage the first stage as usual, with Oxygyen if ordered by the doctor. Use sitting up position if dyspneic.
- In the second stage, use episiotomy, forceps, or vacuum extraction to reduce over-straining from pushing.
- Perform C-section only for specific obstetrical indications, e.g., fetal distress.
- Actively manage the third stage to prevent unnecessary blood loss.
During Puerperium:
- Manage as other mothers.
- If the mother has an active infection, she should breastfeed with a mask, and the baby should be taken back to the nursery.
- No Contraindication: Breastfeeding is not contraindicated when a woman is taking anti-tuberculous drugs.
- Avoidance: Breastfeeding should be avoided if the infant is also receiving anti-tuberculosis medications to prevent drug accumulation.
- Active Lesions: Breastfeeding is contraindicated in cases of active TB. The infant should be isolated from the mother after delivery and given prophylactic isoniazid (10-20 mg/kg/day) for 3 months.
- Chemotherapy: If the mother has been on effective chemotherapy for at least two weeks, there is no need to isolate the baby.
- If the mother’s sputum is positive, give the baby BCG at birth and protect with isoniazid syrup (2.5mg/kg/day). The vaccine becomes effective in 3-6 weeks; if any family member is infected, separation is advised.
- Mantoux test is carried out after 6 weeks.
- If the mother is negative or inactive, she can stay with her baby.
- Advise rest and sleep, and a well-balanced diet to avoid recurrence of active disease.
- Avoid pregnancies until the disease has been controlled for 2 years.
- Long-term medical and social follow-up is necessary to monitor the disease and its treatment.
Effects of TB on Pregnancy:
Maternal Effects on Pregnancy:
- General Debilitation: TB weakens the mother’s overall health, making it challenging to cope with the demands of pregnancy.
- Placental Insufficiency: TB can impair placental function, leading to:
- Premature Labor: Increased risk of delivering before term.
- Intrauterine Fetal Death: Loss of the fetus during pregnancy.
- Intrauterine Growth Retardation (IUGR): The fetus fails to grow at an appropriate rate due to inadequate nutrient and oxygen supply.
- Fetal Hypoxia: Reduced oxygen levels in the fetus due to placental insufficiency.
- Asphyxia: Severe oxygen deprivation in the fetus, potentially leading to brain damage or death.
During Labour:
- Increased Risk of Assisted Deliveries: TB-related complications can increase the need for interventions like forceps or vacuum extraction.
- Maternal and Fetal Distress: Both the mother and the fetus may experience complications during labor, such as heart rate abnormalities, due to TB-related physiological changes.
- High Prenatal Mortality Rate: The risk of stillbirth is significantly elevated in mothers with TB.
Note: Pregnant or breastfeeding women with TB should be treated with short-course chemotherapy (e.g., Rifampicin, Isoniazid, Pyrazinamide, Ethambutol).
Effects on Puerperium:
- Anaemia: TB can worsen existing anaemia or lead to new iron deficiency in the postpartum period.
- Poor Lactation: TB can impair breast milk production, impacting infant nutrition.
- Lowered Resistance to Infection: The mother’s immune system is compromised, increasing her susceptibility to infections during the postpartum period.
Prevention:
In the Community:
- Sensitize and mobilize the community to create awareness about TB.
- Health education on ensuring well-ventilated homes, avoiding overcrowding, proper disposal of sputum, covering the mouth when coughing/sneezing, and screening family members.
- Encourage good nutrition, drinking pasteurized milk products, disinfecting patients’ belongings, and immunizing children with BCG.
- Ensure adequate management of chest infections and encourage mothers to attend ANC.
In Hospital:
- Encourage mothers to attend ANC for thorough examinations, histories, and investigations for management.
- Keep the hospital environment clean and dispose of refuse properly.
- Ensure ward cleanliness by scrubbing floors, dusting windows, and cleaning equipment daily.
- Health workers should avoid droplet infections, wash hands after every procedure, and isolate TB patients.
Complications:
Spontaneous Pneumothorax: A collapsed lung due to air leaking into the space between the lung and chest wall.
- Pleural Effusion: Fluid buildup in the space between the lung and chest wall.
- Gastrointestinal TB: TB infection affecting the digestive system.
- Massive Hemolysis: Breakdown of red blood cells, leading to anemia and potentially fatal complications.
- TB Meningitis: Infection of the membranes surrounding the brain and spinal cord.
- TB Pericarditis: Inflammation of the sac surrounding the heart.
- Anaemia: Iron deficiency, which can be exacerbated by TB infection.
- Death: In severe cases, TB can be fatal, especially in pregnant women who are immunocompromised.
- Hemoptysis: Coughing up blood due to lung damage.
- High Maternal Mortality Rate: The risk of death from TB is significantly elevated in pregnant women.