Table of Contents
ToggleSevere Acute Respiratory Syndrome (SARS)
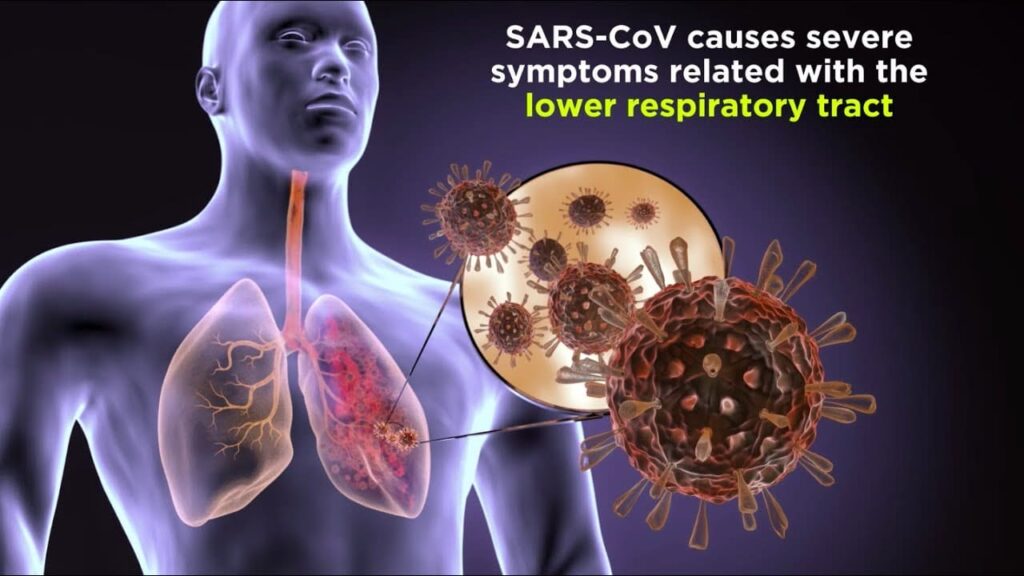
Severe Acute Respiratory Syndrome (SARS) is a viral respiratory illness caused by the SARS coronavirus (SARS-CoV), first identified in 2002.
It’s characterized by a rapid onset of fever, cough, and shortness of breath, often progressing to pneumonia and acute respiratory distress syndrome (ARDS).
While the 2003 outbreak was effectively contained, the emergence of SARS-CoV-2 (the virus causing COVID-19) highlights the ongoing threat of novel coronaviruses.
SARS is considered a zoonotic disease, meaning it originated in animals and then spread to humans.
The exact animal origin remains uncertain, but evidence suggests it may have originated in bats, possibly with an intermediate animal host facilitating transmission to humans.
Forms and Routes of Transmission:
SARS primarily transmits through close contact with an infected individual. There are no known distinct “forms” of SARS like there are for anthrax (cutaneous, inhalation, etc.). The routes of transmission include:
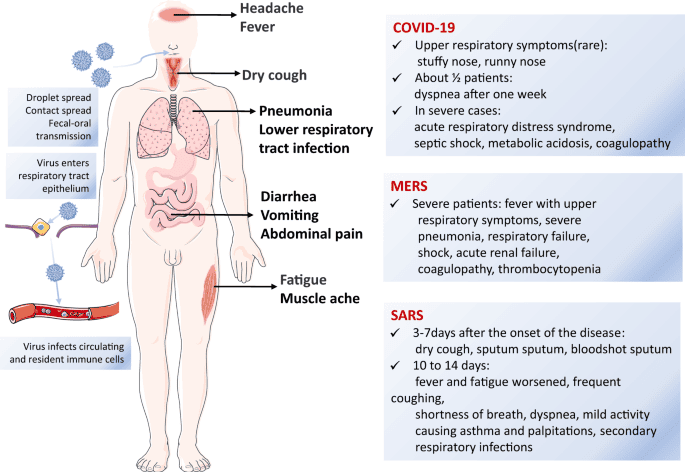
Droplet Transmission: The primary route. Large respiratory droplets expelled during coughing, sneezing, or talking can infect individuals within close proximity (generally within 6 feet).
Contact Transmission: Touching contaminated surfaces (e.g., doorknobs, handrails) and then touching one’s face (eyes, nose, mouth) can lead to infection.
Fecal-Oral Transmission: Although less common, SARS-CoV RNA has been detected in stool samples, suggesting potential fecal-oral transmission, especially in healthcare settings.
Incubation Period:
The incubation period for SARS is usually 2-10 days, with a median of about 5 days. This means that symptoms may not appear until several days after exposure.
Causes/Etiology:
The causative agent is the SARS coronavirus (SARS-CoV), a positive-sense single-stranded RNA virus belonging to the Coronaviridae family.
Clinical Features
SARS presents with a range of symptoms, often starting with a relatively mild prodrome:
- High Fever: Typically above 38°C (100.4°F).
- Dry Cough: Often a prominent symptom.
- Shortness of Breath: Progressing to dyspnea (difficulty breathing).
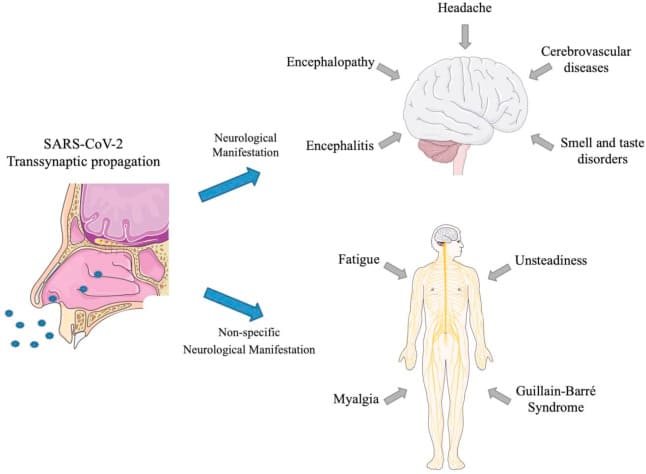
- Myalgia (Muscle Aches): Widespread muscle pain.
- Headache: Often reported.
- Chills: Feeling cold and shivering.
- Fatigue: Significant exhaustion and weakness.
- Malaise: A general feeling of illness and discomfort.
- Diarrhea: Can occur in some patients.
- Sore Throat: May be present.
- Pneumonia: Often develops, leading to respiratory distress.
- Acute Respiratory Distress Syndrome (ARDS): A life-threatening complication involving severe lung inflammation.
Definitive Diagnosis and Investigations:
Diagnosis is confirmed through laboratory testing:
- Reverse Transcription-Polymerase Chain Reaction (RT-PCR): Detects the SARS-CoV RNA in respiratory samples (e.g., nasal swabs, sputum). This is the gold standard for diagnosis.
- Serological Tests: Detect antibodies against SARS-CoV in blood samples. These tests are helpful for retrospective diagnosis but may not be positive early in the course of infection.
- Chest X-ray or CT Scan: May show characteristic findings of pneumonia. These imaging techniques help assess lung involvement but are not specific for SARS.
Management:
Aims of Management:
- Supportive care to manage symptoms and complications.
- Prevention of secondary infections.
- Prevention of the spread of the virus.
Emergency Management:
Patients with severe respiratory distress (e.g., hypoxia, ARDS) require immediate emergency care including oxygen therapy, mechanical ventilation, and intensive care unit (ICU) admission.
First Aid/Initial Management:
- Isolate the suspected patient to prevent further spread.
- Provide supportive care: fluids, rest, fever control (acetaminophen).
- Seek immediate medical attention.
Medical Management:
- Antiviral Medications: No specific antiviral treatment proved definitively effective against SARS-CoV during the 2003 outbreak. Research is ongoing. However, supportive care is paramount.
- Oxygen Therapy: For patients with hypoxia.
- Mechanical Ventilation: For patients with severe respiratory failure and ARDS.
- Corticosteroids: May be used in some cases to reduce inflammation, but their benefit is still debated.
Nursing Care:
- Strict Infection Control: Use appropriate personal protective equipment (PPE) – gowns, gloves, masks, eye protection – to prevent transmission.
- Respiratory Support: Monitor oxygen saturation, provide oxygen therapy, and assist with mechanical ventilation.
- Fluid Balance: Monitor fluid intake and output, and administer intravenous fluids as needed.
- Monitoring Vital Signs: Closely monitor temperature, heart rate, blood pressure, respiratory rate, and oxygen saturation.
- Psychological Support: Provide emotional support to the patient and their family.
- Isolation and Ventilation: Admit patients to a well-isolated and ventilated area to prevent further spread.
- Protective Gear: Wear appropriate personal protective equipment (PPE) like gowns, gloves, masks, and eye protection when caring for SARS patients.
- History and Physical Examination: Take a thorough history and perform a general physical examination.
- Vital Signs: Monitor temperature, pulse, respiration, and blood pressure regularly and record the findings.
- Temperature Management: For high fever, tepid sponging may be used to reduce body temperature.
- Oxygen Therapy: Provide supplemental oxygen for patients with hypoxemia (low oxygen levels in the blood).
- Medication Administration: Administer prescribed medications following proper protocols.
- Hygiene: Practice strict hand hygiene – washing hands before and after caring for the patient.
- Limit Staff Exposure: Minimize the number of healthcare workers caring for the patient to reduce transmission risk.
Reporting: Report suspected cases to the appropriate authorities for effective case management.
Management Up to Discharge:
Patients must meet specific criteria for discharge, including resolution of fever, improvement in respiratory symptoms, and two negative RT-PCR tests.
Advice on Discharge:
- Continue to monitor for any recurrence of symptoms.
- Contact a healthcare provider immediately if symptoms worsen.
- Follow up appointments as scheduled.
Prevention:
Infection Control: Strict adherence to infection control measures in healthcare settings and other high-risk environments.
Hygiene: Frequent handwashing with soap and water or alcohol-based hand sanitizer.
Respiratory Hygiene: Covering coughs and sneezes with a tissue or elbow.
Quarantine: Isolation of infected individuals to prevent transmission.
Contact Tracing: Identifying and monitoring individuals who have been in contact with infected persons.
Early Detection and Case Management: Prompt identification and treatment of infected individuals.
Complications:
Pneumonia: A common complication that can be life-threatening.
Acute Respiratory Distress Syndrome (ARDS): A severe lung condition leading to respiratory failure.
Sepsis: A systemic inflammatory response to infection.
Multiple Organ Failure: Can occur in severe cases.