Table of Contents
ToggleMENOPAUSE
The term menopause originates from the Greek words:
Mens – meaning “monthly“
Pausis – meaning “cessation.”
Menopause is a natural stage in a woman’s aging process, characterized by a decline in ovarian function, leading to reduced production of the hormones estrogen and progesterone. This physiological change results in the permanent cessation of menstruation and the end of reproductive capability.
Key characteristics of menopause:
- It signifies the end of fertility in women.
- Menopause is confirmed after 12 consecutive months of amenorrhea (absence of menstruation).
This stage is a gradual process, accompanied by numerous physical, psychological, and social changes that vary among individuals.
Menopause is defined as the permanent cessation of menstruation due to the loss of ovarian follicular activity.
It marks the end of a woman’s reproductive life.
Note:
– Natural Menopause: Defined as the absence of menstruation for at least 12 months in women aged 45 years or older without any pathological cause.
– Average Age: The average age of menopause is around 51 years but ranges between 45–55 years.
– Premature Ovarian Failure (POF): Menopause occurring before the age of 40 years is classified as premature ovarian failure.
Phases/Stages of Menopause
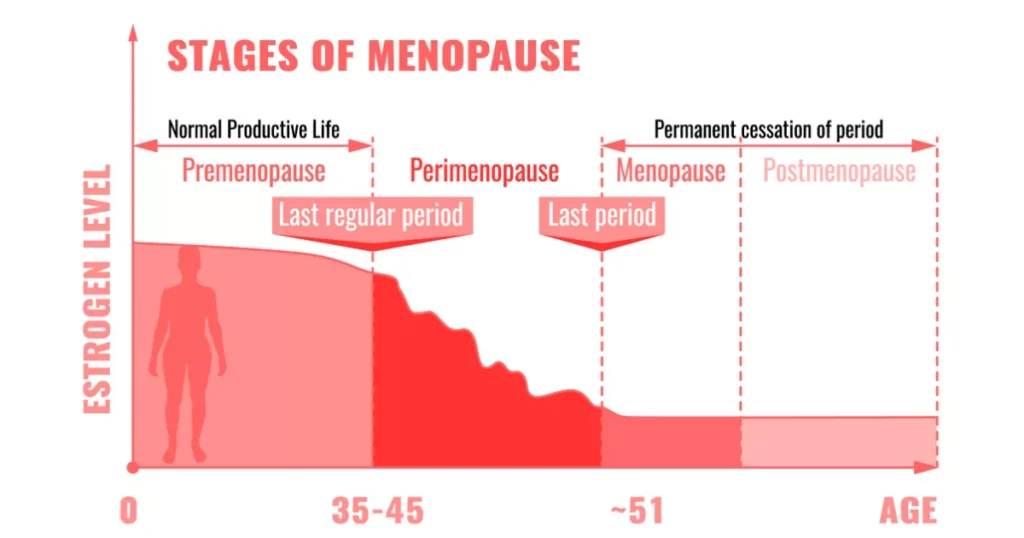
The menopausal transition is not a single event but a process having several phases and these are;
1. Premenopause: This refers to the time before menopause, during which menstrual cycles may start becoming irregular. Usually occurs before the age of 40 years.
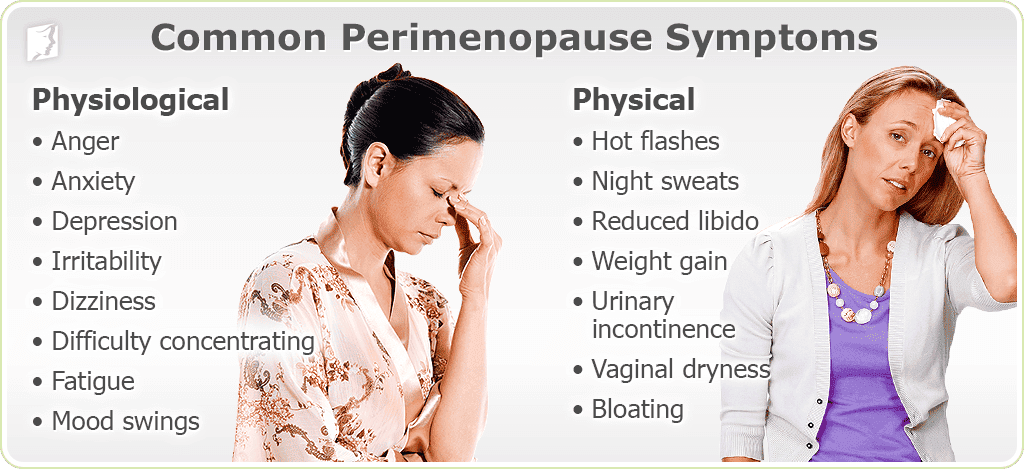
2. Perimenopause(Climacteric): This is the transitional period surrounding menopause, generally lasting from 40 to 55 years of age. It encompasses the physiological changes associated with the end of reproductive capacity, culminating in menopause. During this time, hormonal fluctuations cause a wide range of symptoms.
- Physiological changes indicating the end of reproductive capacity.
- Irregular menstruation.
- Transition ends with the completion of menopause.
3. Menopause: This marks the final menstrual period. It’s considered complete after 12 months of amenorrhea. The average age is 50, falling within the broader 45-55 year range.
- Represents the final menstrual period and occurs between the ages of 45–55 years.
- The average age of menopause is 50 years.
4. Postmenopause: This phase begins after 12 consecutive months of amenorrhea, signifying the permanent cessation of menstrual cycles.
- The phase after 12 consecutive months of amenorrhea.
- Hormonal changes stabilize, but long-term consequences of estrogen deficiency become evident, such as bone density loss and cardiovascular risks.

Diagnosis of Menopause
Diagnosing menopause relies primarily on the retrospective observation of 12 consecutive months without menstruation (amenorrhea) in a woman aged 45 or older, in the absence of any underlying medical conditions. Several factors influence the timing of menopause:
- Age: Menopause commonly occurs between the ages of 45–55 years, with an average of 51 years.
- Amenorrhea: A woman is considered menopausal after 12 consecutive months without menstruation.
- Genetic Factors: The timing of menopause is influenced by genetics.
- Body type: Thinner women tend to experience menopause earlier.
- Lifestyle Factors: Early menopause is associated with:
- Smoking
- Severe malnutrition
- Being underweight
Clinical Confirmation: Retrospective confirmation occurs after observing amenorrhea for 12 months, ensuring no pathological cause for the absence of menstruation.
Causes of Menopause
The primary cause is the natural depletion of ovarian eggs. Once the ovaries are depleted to a point where no amount of hormonal stimulation can trigger ovulation, menopause ensues. Other causes include:
- Premature Ovarian Failure (POF): Menopause occurring before age 40 due to early depletion of ovarian follicles.
- Surgical Menopause: Removal of both ovaries (Oophorectomy) or the uterus (hysterectomy).
- Chemotherapy or Radiation Therapy: Certain chemotherapy regimens can induce premature menopause due to damage to ovarian tissues.
- Stress and Chronic Illness: While the exact role of stress is debated, it may contribute to earlier menopause onset in some individuals. Contributing factors to hormonal imbalance.
Physiological Changes in Menopause
1. General Appearance;
Skin:
- Loses elasticity due to reduced elastin and collagen.
- Becomes thinner and more fragile.
Hair:
- Hair becomes dry, coarse, and prone to loss.
Weight:
- Mood swings may contribute to irregular eating habits, resulting in weight gain.
Voice:
- Becomes deeper due to thickening of the vocal cords.
Fat Distribution:
- Increased fat accumulation around the hips, waist, and buttocks.
2. Vasomotor Changes;
Hot Flashes:
- Sudden sensations of intense heat (Sudden warmth), often starting from the face and spreading to the upper body.
- Can occur frequently and are accompanied by sweating.
Night Sweats:
- Episodes of sweating severe enough to disturb sleep.
- Hot flashes that occur during sleep, often severe enough to disrupt sleep and cause insomnia. These can lead to secondary effects such as palpitations and panic attacks due to sudden awakenings.
3. Metabolic Changes;
Cholesterol Levels:
- Rise in LDL cholesterol increases the risk of cardiovascular diseases and stroke.
Bone Density Loss:
- Rapid calcium loss from bones in the first five years after menopause.
- Increased risk of osteoporosis and fractures.
Digestive Changes:
- Slower digestion and constipation due to reduced metabolic activity.
Urinary Changes:
- Thinning and drying of the urethral and bladder lining due to low estrogen can cause increased urinary frequency and a higher susceptibility to urinary tract infections (UTIs).
4. Changes in Genital Organs;
Uterus:
- Atrophy (shrinking) of uterine muscles, resulting in a smaller, fibrotic uterus.
Cervix:
- The cervix shrinks and may become indistinguishable from the vagina in older women. Cervical and vaginal discharge diminishes and eventually ceases.
Ovaries:
- The ovaries become smaller and shriveled. Increased androgen secretion can lead to facial hair growth and voice changes. In obese women, increased androgen production can increase the risk of endometrial hyperplasia and carcinoma.
Vagina:
- The vaginal mucous membrane thins, resulting in dryness, a change in pH (becoming more alkaline), loss of glycogen and lactobacilli, and dyspareunia (painful sexual intercourse).
Vulva and External Genitalia:
- The labia majora may lose fat, the mons pubis may decrease in size, pubic hair may become sparse, and the vaginal opening (introitus) may narrow.
- Sparse pubic hair and reduced fat in the mons pubis and labia majora.
Breasts:
- Breasts may become flatter and shriveled in thin women, or flabby and pendulous in heavier women.
Psychological Changes in Menopause
Hormonal fluctuations significantly impact mood and cognitive function, leading to:
- Headaches: Frequent headaches are common.
- Mood Disturbances: Irritability, depression, anxiety, mood swings, aggression, and tension are frequently reported.
- Cognitive Changes: Fatigue, memory loss, difficulty concentrating are often experienced.
- Emotional Changes: Depression, anxiety, and unstable moods are prevalent.
- Sleep Disturbances: Sleepiness, insomnia, restlessness and phobias are common complaints. Low self-esteem and tearfulness can also occur.
These changes may impact self-esteem and interpersonal relationships.

Hormone Replacement Therapy (HRT)
Hormone Replacement Therapy (HRT) is a therapeutic intervention designed to alleviate symptoms of menopause by supplementing the diminished levels of hormones, particularly estrogen.
This approach targets both physical and psychological menopausal symptoms, enhancing the quality of life for affected women
HRT: Hormone replacement therapy (HRT) aims to alleviate menopausal symptoms by supplementing declining levels of estrogen (and sometimes progesterone) in women.
Purpose:
- Alleviate symptoms such as hot flashes, night sweats, and vaginal dryness.
- Protect against long-term effects of hormone deficiency, including osteoporosis and cardiovascular disease.
Indications for HRT
- Symptomatic Women: Women experiencing menopausal symptoms related to estrogen deficiency.
- Premature Ovarian Failure (POF): To manage symptoms and improve health in women with POF.
- Surgical or Radiation-Induced Menopause: To mitigate the abrupt onset of menopausal symptoms following surgery (oophorectomy, hysterectomy) or radiation treatments.
- Prophylaxis (Preventive): While controversial, some women may consider HRT to prevent long-term consequences of estrogen deficiency, such as osteoporosis, though this use is not universally recommended.
- Women with gonadal dysgenesis.
Drugs Used in HRT
Category | Common Drugs | Function |
Estrogen | Conjugated estrogen, Micronized estradiol | Replaces lost estrogen to alleviate vasomotor symptoms and prevent osteoporosis. |
Progesterone | Medroxyprogesterone acetate, Dydrogesterone, Micronized progesterone | Prevents endometrial hyperplasia when given alongside estrogen. |
Tibolone | Synthetic steroid with weak estrogenic, progestogenic, and androgenic properties | Relieves hot flashes, prevents osteoporosis, and increases libido. |
Raloxifene | Selective estrogen receptor modulator (SERM) | Provides estrogen-like effects on bones without stimulating breast or endometrial tissue. |
Bisphosphonates | Alendronate, Risedronate | Used to treat and prevent osteoporosis by inhibiting bone resorption. |
Soy Isoflavones | Plant-based compounds with mild estrogenic activity | Provide a natural alternative to estrogen therapy for symptom relief. |
Androgens | Testosterone | Prescribed occasionally to improve libido and energy in postmenopausal women. |
Types of HRT
HRT formulations are tailored to individual needs, depending on whether the patient has an intact uterus or has undergone hysterectomy.
Type | Indication | Details |
Estrogen & Progesterone | For women with an intact uterus. | Prevents endometrial hyperplasia by balancing estrogen’s effect on the uterine lining. |
Estrogen Only | For women who have undergone hysterectomy. | No risk of endometrial cancer; progesterone is not needed. |
Progestin Only | Rarely used; indicated for women who cannot tolerate estrogen or have a history of estrogen-sensitive cancers. | Provides symptom relief, especially for hot flashes and prevention of osteoporosis. |
Commonly Used HRT Preparations
Oral HRT
- Estrogen alone: For women post-hysterectomy.
- Estrogen + Cyclic Progestin: Estrogen is given for 25 days; progestin is added during the last 12–14 days to protect the uterine lining.
- Continuous Estrogen + Progestin: Both hormones are given daily to minimize risks of endometrial hyperplasia.
Non-Oral HRT Options
Method | Details | Advantages |
Transdermal Patch | Releases 50 µg estradiol/24 hours; applied below the waistline and changed twice weekly. | Bypasses the liver, reduces triglycerides. |
Vaginal (Cream, Ring, Pessary) | Contains conjugated estrogen; applied locally for urogenital atrophy symptoms. | Effective for atrophic vaginitis and urinary issues. |
Subdermal Implants | Implants of estradiol (25–100 mg) inserted subcutaneously every six months. | Long-lasting effect. |
Percutaneous Gel | Applied daily on the abdomen or thigh; maintains blood estradiol levels. | Non-invasive and easy to use. |
Dosages of Estrogen
Formulation | Standard Dose | Low Dose |
Conjugated Estrogen (CEE) | 0.625 mg/day | 0.3–0.45 mg/day |
Micronized Estrogen | 1–2 mg/day | 0.5 mg/day |
Transdermal Estrogen | 50 µg/day | 14 µg/day |
Duration and Contraindications of HRT
Duration
- Short-term use (3–5 years) is generally recommended.
- Dosage tapering is encouraged to minimize risks.
Contraindications
- Unexplained vaginal bleeding.
- Active liver or gallbladder disease.
- Estrogen-dependent cancers (e.g., endometrial or breast cancer).
- History of venous thromboembolism.
Benefits and Risks of HRT
Benefits | Risks |
Relief from vasomotor symptoms (70–80%). | Increased risk of breast cancer with long-term use. |
Prevention of osteoporosis and fractures. | Elevated risk of heart disease by 24%. |
Improvement in urogenital atrophy symptoms. | Possible endometrial hyperplasia if not balanced. |
Potential reduction in colorectal cancer risk. | Thromboembolic events. |
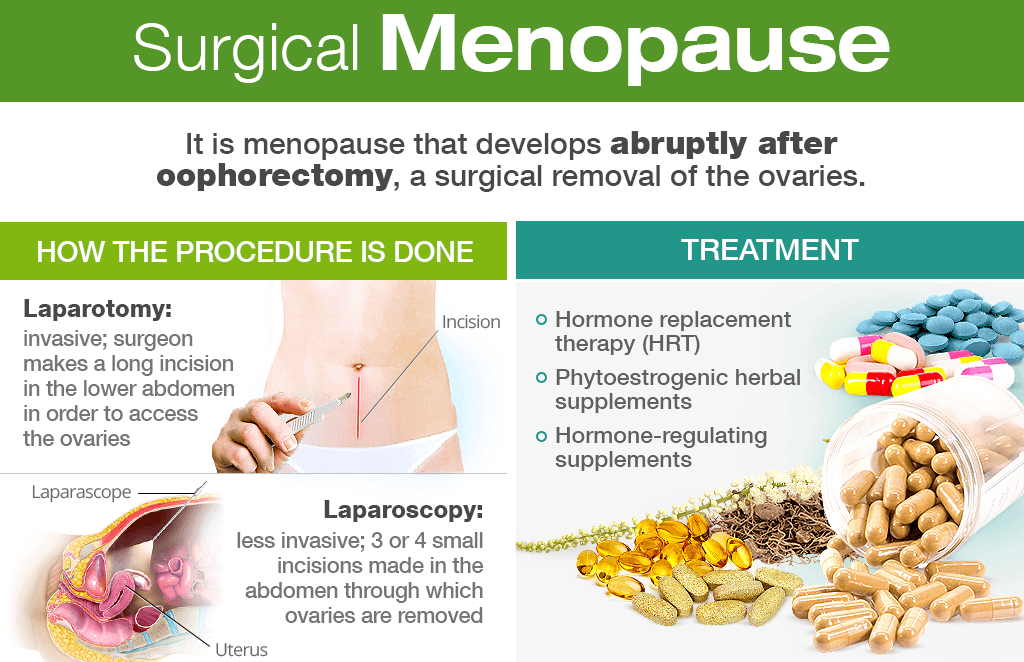
Surgical Menopause
Surgical menopause occurs when hormone production by the ovaries is abruptly interrupted due to procedures like hysterectomy.
Surgical menopause occurs due to the removal of ovaries (oophorectomy) or the combination of removal of the ovaries and uterus (hysterectomy). This results in an abrupt cessation of hormone production, leading to more severe and potentially longer-lasting menopausal symptoms compared to natural menopause.
Symptoms of Surgical Menopause
Essentially, the symptoms mirror those of natural menopause, but are often more intense and can include:
- Intense hot flashes and night sweats
- Sleep disturbances
- Severe vaginal dryness and atrophy
- Decreased libido
- Dyspareunia (painful intercourse)
- Increased risk of osteoporosis, cardiovascular disease, and mood disorders
Management
- HRT: Includes oral tablets, patches, gels, vaginal creams, and implants.
- Lifestyle Adjustments: Regular exercise, a calcium-rich diet, and stress management.
- Counseling: Addressing emotional and psychological aspects of menopause.
Guidance and Counseling
Counseling plays a pivotal role in helping women navigate menopause. Counseling is crucial for managing the physical and emotional aspects of menopause. This involves:
- Individualized assessment of needs and priorities.
- Address emotional and psychological challenges such as anxiety, depression, and loss of fertility.
- Educate women on symptom management, including lifestyle modifications and dietary adjustments.
- Promote regular physical activity and social connections to improve overall well-being.
- Support for decision-making around HRT.
- Addressing psychological concerns such as anxiety and depression.
Specific Lifestyle Advice to Manage Menopausal Symptoms
Symptom | Management Tips |
Hot Flushes | Wear cotton clothes, use fans, avoid triggers (caffeine, alcohol, spicy foods), avoid caffeine, and practice relaxation techniques. |
Vaginal Dryness | Use lubricants or vaginal creams; spend more time in foreplay during intimacy. |
Urinary Incontinence | Perform pelvic floor exercises like Kegel exercises to strengthen bladder control. |
Osteoporosis Prevention | Engage in weight-bearing exercises; consume calcium-rich foods like dairy products and green vegetables. |
Preventive Measures
Condition | Action |
Cardiovascular Disorders | Maintain a healthy diet rich in fruits, vegetables, and olive oil; exercise regularly. |
Gynecological Cancers | Perform regular breast self-examinations; undergo mammograms and Pap smears as advised. |
ROLE OF MIDWIFERY NURSE IN MANAGEMENT OF MENOPAUSE
- Educator: Teaching women about what to expect during menopause, including common symptoms and how long they may last.
- Symptom Assessor: Talking with women about their symptoms to understand their experiences and needs.
- Lifestyle Advisor: Suggesting healthy lifestyle changes like diet and exercise to help manage symptoms naturally.
- Hormone Therapy Advisor: Explaining hormone replacement therapy (HRT) options, benefits, risks, and suitability for each woman.
- Medication Manager: Helping women understand and manage their medications (HRT or other treatments) effectively.
- Mental Health Supporter: Recognizing and addressing emotional or mental health issues related to menopause (e.g., anxiety, depression). Referring to appropriate mental health professionals when necessary.
- Holistic Care Provider: Considering the whole woman – her physical, emotional, and social wellbeing – when planning her care.
- Advocate: Supporting women in making informed decisions about their menopausal care and advocating for their needs.
- Referral Specialist: Connecting women with other healthcare professionals (doctors, specialists) if needed for further assessments or treatments.
- Long-Term Care Planner: Helping women develop a long-term plan for managing their menopausal health, including strategies for preventing future problems like osteoporosis.

Well explained notes, easy to understand and brief