Table of Contents
ToggleEPILEPSY IN PREGNANCY
Epilepsy is a chronic disorder characterized by recurrent, unpredictable seizures due to temporary dysfunction of the brain’s neurons producing excessive electrical discharge.
Although it typically presents in childhood, it has a second peak in older adults, with women of childbearing age accounting for 23% of those affected. The prevalence of epilepsy in pregnancy is 0.35%.
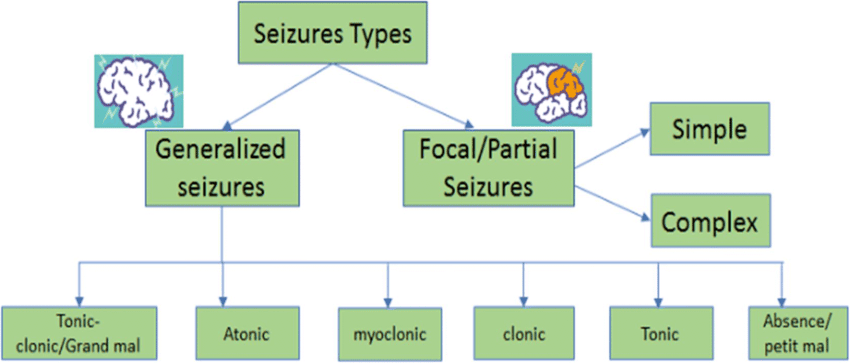
Types of Epilepsy
A. Partial Epilepsy
1. Simple Partial Seizures:
- Consciousness remains intact.
- Experiences an aura (premonition).
- Sensations like pins and needles in the arms or legs.
- Pallor or a flushed face with sweating.
- Muscle twisting in limbs with some stiffness.
2. Complex Partial Seizures:
- Loss of memory of the event.
- Hand rubbing.
- Chewing and smacking of lips.
- Random noises.
- Unusual posture.
B. Generalized Epilepsy
1. Absence Seizures:
- Staring and blinking.
- Daydreaming with loss of awareness for 5-20 seconds (mainly affects children).
2. Myoclonic Seizures:
- Brief muscle jerking in an arm or leg, lasting a fraction of a second while remaining conscious.
- All body muscles contract for less than 20 seconds without convulsions, causing the individual to fall.
3. Tonic-Clonic Seizures:
- Whole body contracts, arms and legs convulse.
- Incontinence is possible.
- Lasts 1-2 minutes, leaving the individual tired and wanting to sleep.
- The most common type of seizure (60% of cases).
4. Atonic Seizures:
- Sudden loss of muscle tone, causing the individual to fall limply.
- Head injury is probable, but the individual gets up immediately with no confusion.
Causes of Epilepsy in Pregnancy
- Idiopathic: Most cases have no underlying cause.
- Genetic Predisposition: 30% of cases have a family history of epilepsy.
- Secondary Epilepsy: Can be encountered in pregnancy in patients with:
- Previous brain surgery.
- Intracranial mass lesions (e.g., meningiomas and arteriovenous malformations).
- Antiphospholipid syndrome.
Other Causes of Seizures in Pregnancy
- Eclampsia.
- Cerebral vein thrombosis (CVT).
- Thrombotic thrombocytopenic purpura (TTP).
- Stroke.
- Subarachnoid hemorrhage.
- Drug and alcohol withdrawal.
- Hypoglycemia.
- Infections (e.g., tuberculoma, toxoplasmosis).
- Gestational epilepsy (seizures confined to pregnancy).
Diagnosis
Most women are already diagnosed with epilepsy. However, if a first seizure occurs during pregnancy, the following investigations are appropriate:
- Blood pressure, urinalysis, platelet count, clotting screen, blood film.
- Blood glucose, serum calcium, serum sodium, liver function tests.
- CT or MRI of the brain.
- EEG (electroencephalogram).
Effects of Epilepsy on Pregnancy
On the Fetus:
- No increased risk of miscarriage or obstetric complications unless a seizure results in abdominal trauma. This is a positive aspect, indicating that epilepsy itself doesn’t inherently increase the risk of these complications.
- Fetal malformations: These can include a range of abnormalities affecting various organs and systems.
- Intrauterine growth restriction (IUGR): This refers to the fetus not growing at the expected rate, potentially leading to low birth weight.
- Oligohydramnios: This is a condition where there is too little amniotic fluid surrounding the fetus, which can be associated with developmental issues.
- Preeclampsia: This is a serious condition characterized by high blood pressure and protein in the urine, which can affect both mother and fetus.
- Stillbirths: This refers to the death of a fetus before birth.
On the Newborn:
- Birth defects are increased two-fold. This could be related to the severity of the disease and also due to the anticonvulsants used. Pattern of abnormalities is related to the type of anticonvulsant drugs (valproate 5.9%, Carbamazepine, 2.3% and Lamotrigine 2.1%).
- The malformations include—Cleft lip and/or palate, mental retardation, cardiac abnormalities, limb defects and hypoplasia of the terminal phalanges. Sodium valproate is associated with neural tube defects.
- There is chance of neonatal hemorrhage and is related to anticonvulsant induced reduction of coagulation factors (vitamin K dependent). The risk of developing epilepsy to the offspring of an epileptic mother is 10%.
On the Mother:
- Increased risk of seizures during pregnancy and postpartum. Hormonal changes and physiological stress associated with pregnancy can trigger seizures.
- Potential for worsening of epilepsy. Some women may experience an increase in seizure frequency or severity during pregnancy.
- Difficulty in managing epilepsy medication during pregnancy. Many anticonvulsants are teratogenic (can cause birth defects), requiring careful consideration and monitoring.
- Increased risk of postpartum depression. This can be exacerbated by the challenges of managing epilepsy and raising a child.
Stress and anxiety associated with pregnancy and childbirth. The fear of seizures and their potential impact on the baby can contribute to maternal stress.
Management of Epilepsy in Pregnancy
Pre-Pregnancy Counseling
1. Control of Epilepsy:
- Maximize seizure control with the lowest dose of the most effective treatment.
- Review antiepileptic drugs (AEDs) considering the risk of teratogenesis and adverse neurodevelopmental effects.
2. Stopping Treatment:
- AEDs should be withdrawn slowly to reduce the risk of withdrawal-associated seizures, particularly important for benzodiazepines and phenobarbitone.
- Current recommendations suggest stopping driving from the start of the drug withdrawal period and for six months after cessation of treatment if there are no seizures.
Newer Drugs with Safety Profiles:
- Topiramate: 100–400 mg/day.
- Levetiracetam: 1–3 gm/day, not an enzyme inducer.
Folic Acid: All women on AEDs should take pre-conception folic acid 4 mg daily starting before pregnancy and continuing throughout pregnancy.
Antenatal Management
1. Medication:
- Keep the dose of chosen drugs as low as possible and monitor serum levels regularly.
- Commonly used drugs include:
- Phenobarbitone (60-100mg daily in divided doses).
- Phenytoin (150-300mg daily in divided doses).
- Carbamazepine (0.8-1.2g daily in divided doses).
- Continue folic acid daily before conception and throughout pregnancy to prevent folate-deficiency anemia.
2. Seizure Control:
- IV Phenytoin: Administer a slow loading dose of 15–20 mg/kg for effective, long-duration control with fewer side effects.
- Benzodiazepines: 10–20 mg slow IV if phenytoin is not effective.
3. Support:
- Educate relatives, friends, and partners on placing the woman in the recovery position to prevent aspiration during a seizure.
- Administer Vitamin K (10 mg daily) orally in the last two weeks of pregnancy.
- Intrapartum Management
4. Seizure Risk:
- The risk of seizures increases around delivery. Women with major convulsive seizures should deliver in a hospital.
- Continue anticonvulsant medication throughout labor with regular review by the obstetric team.
- Administer short-acting benzodiazepines if seizures recur.
5. Labor and Delivery:
- Women should not be left alone during labor, and dehydration, hyperventilation, and exhaustion should be avoided as they can trigger seizures.
6. Vitamin K:
- 10 mg daily orally to the mother in the last two weeks of pregnancy.
- Infant: 1 mg IM at birth to prevent neonatal hemorrhage
- Birth can be spontaneous, facilitated by the midwife. Administer vitamin K to the baby promptly after birth to protect against AED-induced hemorrhagic disease.
- Caesarean section is only necessary for recurrent generalized seizures in late pregnancy or labor.
Postpartum Management
7. Seizure Risk:
- The risk of seizures increases in the first 24 hours after birth, so the woman should remain in the hospital.
- Encourage breastfeeding.
- Monitor the baby closely and report any concerns to the pediatrician immediately.
- Provide safety advice for caring for the baby in case of maternal seizures.
8. Breastfeeding:
- There is no contraindication for breastfeeding.
- Infant: May be drowsy due to medication.
9. Postpartum Management:
- Readjustment of Anticonvulsant Dosage: Reduce to pre-pregnancy levels by 4–6 weeks postpartum.
10. Contraception:
- Avoid steroidal contraceptives due to hepatic microsomal enzyme induction.
11. Risk to Infant:
- The risk of having epilepsy in an infant born to a mother with a seizure disorder is four times higher compared to infants born to mothers without a seizure disorder.
Complications Associated with Epilepsy
- Trauma: During seizures, injuries such as tongue biting and head or limb injuries can occur.
- Status Epilepticus: A seizure lasting more than 30 minutes or a series of seizures without regaining consciousness between them.
- Sudden Unexpected Death in Epilepsy (SUDEP): An unexplained sudden death in a person with epilepsy.

