Table of Contents
ToggleElephantiasis (Lymphatic Filariasis)
Elephantiasis, also known as lymphatic filariasis, is a chronic parasitic disease caused by filarial worms.
It results in severe swelling, primarily of the legs, arms, breasts, and genitals, due to blockage of the lymphatic system. The condition gets its name from the enlargement of affected limbs, resembling that of an elephant.
Elephantiasis is a debilitating disease that can significantly impact a person’s physical, social, and economic well-being. The swelling can cause pain, disfigurement, disability, and social stigma. It is a neglected tropical disease (NTD) primarily affecting impoverished communities in tropical and subtropical regions.
Transmission:
Vector: The disease is transmitted by mosquitoes, specifically species of the genera Culex, Anopheles, and Aedes.
Lifecycle:
In the Mosquito (Vector):
- Infected mosquitoes ingest filarial larvae (microfilariae) from an infected person’s blood.
- The microfilariae develop into mature larvae (L3 larvae) in the mosquito.
- L3 larvae migrate to the mosquito’s mouthparts, ready for transmission.
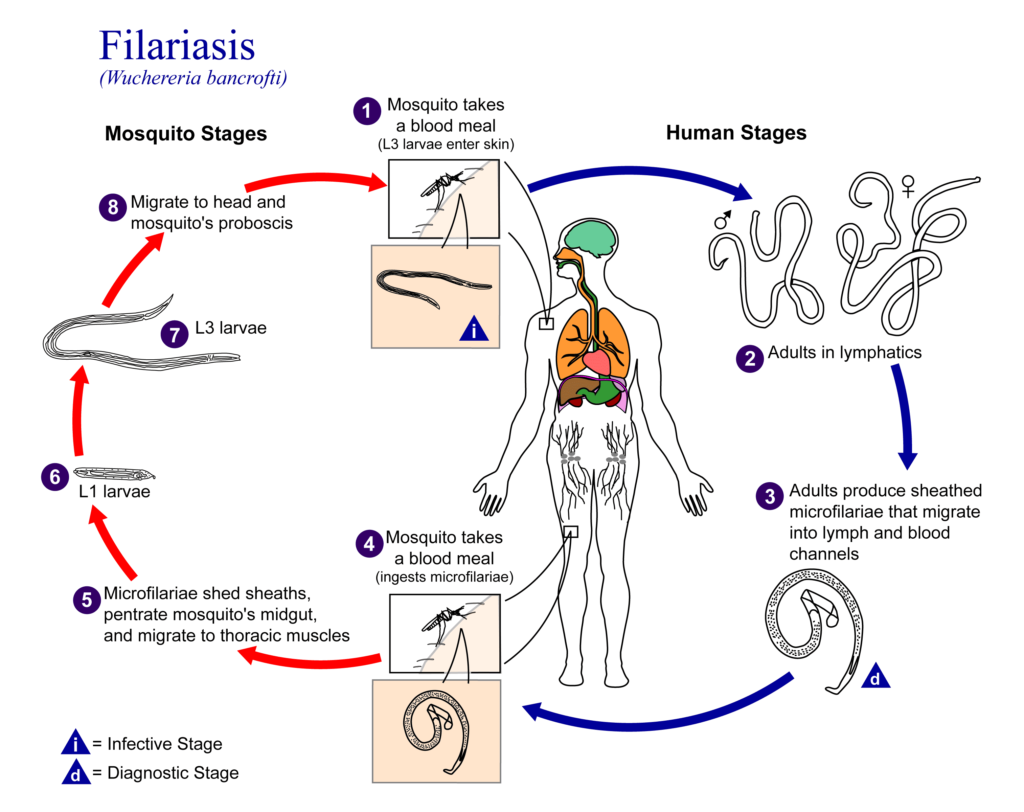
In Humans (Host):
- Infected mosquitoes bite humans, transmitting the L3 larvae into the bloodstream.
- L3 larvae mature into adult worms in the lymphatic system, typically residing in lymph nodes.
- Adult worms reproduce, releasing microfilariae into the bloodstream, which can then be ingested by mosquitoes, completing the cycle.
Routes of Transmission:
- Mosquito Bite: The primary route of transmission is through the bite of an infected mosquito.
- Blood Transfusion: Transmission is possible through contaminated blood transfusions, although less common.
Causes/Aetiology:
Filarial Worms: The disease is caused by three main species of filarial worms:
- Wuchereria bancrofti (most common)
- Brugia malayi
- Brugia timori
Clinical Features:
1. Early Stage (Lymphangitis):
- Fever
- Chills
- Pain and redness along lymphatic vessels
- Lymphadenitis (swollen lymph nodes)
2. Subcutaneous Stage (Lymphedema):
- Swelling in the extremities, particularly legs and arms.
- Pitting edema (fluid retention that leaves indentations when pressed)
- Skin thickening and roughness
3. Late Stage (Elephantiasis):
- Massive swelling of the limbs, breasts, or genitals.
- Thickened and deformed skin.
- Lymphatic obstruction leading to fluid buildup.
- Increased susceptibility to secondary infections.
4. Genital Manifestations:
- Hydrocele (fluid accumulation in the scrotum).
- Lymphoedema of the scrotum (scrotal elephantiasis).
- Lymphoedema of the vulva (vulvar elephantiasis).
5. Other Complications:
- Chylous ascites (fluid buildup in the abdomen).
- Chylothorax (fluid buildup in the chest).
- Chronic kidney disease.
Diagnosis and Investigations:
Clinical Examination: Characteristic swelling and history of mosquito bites in endemic areas.
Microscopic Examination:
- Blood smear: To detect microfilariae in blood samples.
- Lymph node aspirate: To detect microfilariae in lymph node fluid.
Serological Tests: Blood tests to detect antibodies against filarial worms.
Imaging Studies:
- Ultrasound: To visualize the lymphatic system and detect adult worms.
- CT scan: To evaluate the extent of lymphatic obstruction.
- MRI: To assess the lymphatic system and surrounding tissues.
Prevention:
Vector Control:
- Mosquito control measures, such as insecticide spraying, insecticide-treated bed nets, and source reduction (eliminating mosquito breeding sites).
- Use of repellents.
Mass Drug Administration (MDA):
- Regular administration of anti-filarial medications (DEC and albendazole) to prevent transmission and reduce disease burden.
- Large scale treatment/preventive chemotherapy Give annually
- to all population at risk, for 4-6 years
- Ivermectin 150-200 mcg/kg plus albendazole 400 mg single dose
Health Education: Educate communities about the disease, transmission, and preventive measures.
Improved Sanitation and Hygiene: Maintain clean surroundings and reduce mosquito breeding sites.
Management:
Aims of Management:
- To kill adult worms and prevent the spread of infection.
- To reduce lymphatic obstruction and swelling.
- To improve quality of life and reduce disability.
Medical Management:
- Anti-filarial Medications: Diethylcarbamazine (DEC) and Albendazole are the primary drugs for treatment.
- Diethylcarbamazine (DEC)
- Albendazole
- Ivermectin (alternative medication)
- Combinations of these drugs may be used.
Antibiotics: For treating secondary bacterial infections.
Doxycycline 100 mg twice a day for 4-6 weeks (do not administer antiparasitic treatment during an acute attack)
Pain Relievers: To manage pain and inflammation.
Diuretics: To reduce fluid buildup.
- Supportive Care:
- Elevate affected limbs.
- Use compression bandages.
- Manage pain and inflammation.
- Supportive treatment during an attack (bed rest, limb elevation, analgesics, cooling, hydration)
Continuous Management:
- Long-term Anti-filarial Therapy: May be required to prevent disease progression.
- Lymphedema Management:
- Regular massage.
- Compression therapy.
- Skin care and hygiene.
Monitoring for Complications: Regular follow-up appointments to monitor for complications, such as secondary infections and kidney damage.
Surgical Management:
- Chronic case: Supportive treatment: bandage during the day, elevation of affected limb at rest, analgesics and surgery (hydrocelectomy)
- Surgery for Complications:
- Surgery may be required to treat complications such as hydrocele, lymphoedema, and chylous ascites.
- Lymphatic bypass surgery may be considered in some cases.
Nursing Care:
- Symptom Management: Provide comfort measures for pain, swelling, and discomfort.
- Skin Care: Promote good skin hygiene to prevent infections.
- Compression Therapy: Apply compression bandages to reduce swelling and improve lymphatic flow.
- Lymphedema Management: Teach patients techniques for self-management of lymphoedema.
- Education: Educate patients about the disease, treatment, and prevention.
Complications:
- Secondary Infections: Frequent skin infections due to impaired lymphatic drainage.
- Lymphedema: Progressive swelling of the affected limbs, leading to disfigurement and disability.
- Elephantiasis: Severe and permanent disfigurement and disability.
- Hydrocele and Lymphoedema of the Genitals: Can cause pain, discomfort, and reproductive problems.
- Chronic Kidney Disease: Fluid overload and lymphatic obstruction can strain the kidneys.
- Social Stigma: Elephantiasis can lead to social isolation and discrimination.
- Psychological Distress: The disease can have a significant impact on self-esteem and mental health.

