Table of Contents
ToggleDRUGS USED IN MIDWIFERY
Drugs used in midwifery are drugs specifically used during pregnancy, labor, delivery, and postpartum care to ensure the health of the mother and baby.
They may induce labor, prevent complications, manage pain, or treat postpartum conditions.
Examples;
- Oxytocics: e.g., Oxytocin (induces or augments labor), Misoprostol (induces labor or manages postpartum hemorrhage).
- Tocolytics: e.g., Nifedipine, Terbutaline (delay preterm labor).
- Anticoagulants: e.g., Heparin (prevents thromboembolism during pregnancy).
- Antiemetics: e.g., Doxylamine + Pyridoxine (treat nausea and vomiting in pregnancy).
- Analgesics/Anesthetics: e.g., Epidural anesthesia (manages labor pain).
- Magnesium Sulfate: Prevents seizures in preeclampsia/eclampsia.
- Rh Immunoglobulin: Prevents Rh incompatibility complications.
Clinical Use;
- Inducing or augmenting labor.
- Managing preterm labor.
- Preventing or treating postpartum hemorrhage.
- Managing pregnancy-related conditions like preeclampsia, nausea, or pain.
DRUGS USED IN LABOUR
Drugs in Labor refers to the medications that are administered to a woman during labor to manage pain, assist with the process of childbirth, or address complications. These drugs can be used for pain relief, induction or augmentation of labor, and management of medical conditions that may arise during labor.
Drugs used in labor can be grouped according to the effect they have on the uterus.
- Uterine relaxants (Tocolytics): These drugs relax the uterus, slowing or stopping contractions such as Nifedipine, Magnesium Sulfate.
- Uterine Stimulants/Uterine Motility drugs. (Oxytocics): These drugs stimulate the uterus to contract, helping to induce or strengthen labor, such as Oxytocin (Pitocin).
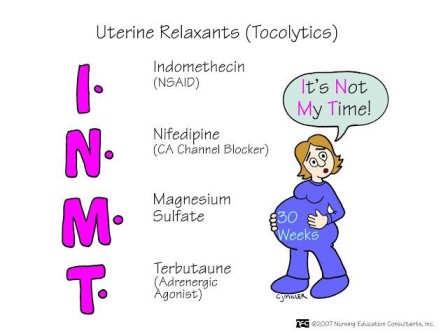
Uterine Relaxants
Uterine relaxants, also known as tocolytics, are a group of medications used to suppress uterine contractions and delay labor.
Their primary goal is to prolong pregnancy, allowing the fetus to develop further and increasing the chances of neonatal survival. These drugs are primarily used to prevent premature labor, particularly when cervical dilation is less than 4 cm.
Types of Uterine Relaxants
Beta-adrenergic agonists (Beta-2 agonists):
- Salbutamol.
- Terbutaline.
Calcium channel blockers:
- Nifedipine.
Magnesium sulfate
Nonsteroidal anti-inflammatory drugs (NSAIDs):
- Indomethacin.
Oxytocin receptor antagonists:
- Atosiban.
Corticosteroids:
- Dexamethasone: (used for fetal lung maturity rather than directly for uterine relaxation but is often used in combination with tocolytics in premature labor)

Salbutamol (A Beta-2 Adrenergic Agonist)
Legal Class: Class B controlled drugs
Medical Class: Tocolytic agent
Form: Tablets, sterile solution for injection
Dosage: Tablets 4 mg; Solution for injection 50 mg/mL
Mechanism of Action
Salbutamol stimulates beta-2 adrenergic receptors in the uterine smooth muscle, leading to increased levels of cAMP, which inhibits myosin light-chain kinase, thereby reducing uterine contractions.
Indications
- Uncomplicated premature labor between 24 to 33 weeks of gestation
- Asthma (as it also has bronchodilatory effects)
Contraindications
- Cardiac diseases (risk of tachycardia and other arrhythmias)
- Antepartum hemorrhage (APH)
- Intrauterine fetal death (IUFD)
- Intrauterine infections
- Ruptured membranes
- Eclampsia and pre-eclampsia
- First and second trimester of pregnancy (risk of fetal malformations)
Dosage
- Premature labor: IV infusion 10 mcg/min, gradually increase according to response at 10-minute intervals until contractions diminish, with a maximum dose of 45 mcg/min. Maintain rate for 1 hour, then gradually reduce by IV or IM injection 100-250 mg, repeated according to response, followed by oral administration of 4 mg every 6-8 hours.
- Duration of use: Do not use for more than 48 hours due to the risk of maternal and fetal complications.
Side Effects
- Hypoglycemia (especially in diabetic patients)
- Vomiting and nausea
- Sweating and tremors
- Hypotension
- Pulmonary edema
- Maternal and fetal tachycardia
- Headache and palpitations
- Urticaria
Adverse Effects
- Severe hypotension
- Pulmonary edema
- Cardiac arrhythmias
- Hyperglycemia

Magnesium Sulfate (MgSO4)
Legal Class: Class B controlled drugs
Medical Class: Tocolytic and anticonvulsant
Form: Sterile solution for injection
Strength/Dosage: 50% of 5 grams/10 mL
Mechanism of Action
Mechanism of Action
Magnesium sulfate acts as a calcium antagonist by competing with calcium for entry into the cells, which decreases the action potential in uterine smooth muscle, leading to muscle relaxation. It also stabilizes membranes by interacting with sodium and potassium channels.
USING MAGNESIUM SULPHATE (MgSO₄) TO PREVENT OR STOP SEIZURES |
LOADING DOSE: |
1. Give 4 g of 20% MgSO₄ solution IV over 20 min. prepared as stated below: |
|
2. Immediately follow this with 10 g of 50% solution deep IM as shown below: |
|
3. If fits re-occur: |
|
MAINTENANCE DOSE: |
Give 5 g of 50% MgSO₄ deep IM in alternate buttocks every 4 hours as shown below: |
|
TOXICITY: |
|
ANTIDOTE: Calcium Gluconate |
|
Dosage
- Loading Dose: 4 g of MgSO4 given slowly IV over 15 to 20 minutes, followed by 10 g IM (5 g in each buttock) with 1 mL of 2% lignocaine to reduce pain.
- Maintenance Dose: 5 g of 50% MgSO4 IM on alternate buttocks every 4 hours. Treatment continues for 24 hours from the start or after the last seizure.
Indications
- Severe eclampsia and pre-eclampsia (prevention and treatment of seizures)
- Hypomagnesemia
- Severe asthma
- Short-term treatment of constipation (acts as a laxative)
- Myocardial infarction (as an adjunct)
Contraindications
- Hypermagnesemia
- Hypersensitivity to MgSO4
- Renal impairment
- Hepatic failure
- Hypotensive patients
- Patients with epilepsy
Side Effects
- Drop in blood pressure
- Flushing of the skin
- Dizziness and confusion
- Muscle weakness and loss of deep tendon reflexes (e.g., knee-jerk reflex)
- Prolonged bleeding time
- Diarrhea
Adverse Effects
- Hypermagnesemia (risk of respiratory depression, cardiac arrest, and coma)
- Magnesium toxicity, leading to respiratory paralysis
- Shock in hypertensive patients

Nifedipine (A Calcium Channel Blocker)
Legal Class: Class B controlled drugs
Medical Class: Tocolytic and antihypertensive
Form: Tablets
Mechanism of Action
Nifedipine inhibits calcium influx through voltage-dependent calcium channels in the smooth muscle, including the uterus, which leads to relaxation and reduced contractility.
Dosage
- Initial Dose: 20 mg, repeat after 30 minutes if contractions persist.
- Maintenance Dose: If contractions continue after 3 hours, give 20 mg every 3-8 hours until contractions cease. The maximum dose is 160 mg/day.
Indications
- Threatened abortion
- Preterm labor less than 34 weeks of gestation
- Hypertension (both chronic and pregnancy-induced)
Contraindications
- Maternal cardiac diseases
- Uncontrolled hypertension
- Intrauterine infections
- Conditions where prolonging pregnancy is contraindicated
- Intrauterine fetal death
Side Effects
- Dizziness and headache
- Flushing and warmth sensation
- Peripheral edema
- Fatigue
- Nausea
Adverse Effects
- Severe hypotension
- Reflex tachycardia
- Congestive heart failure (CHF) exacerbation
Uterine Stimulants/Uterine Motility Drugs (Oxytocics)
Uterine motility drugs, also known as oxytocics, are agents used to stimulate uterine contractions.
These medications are primarily used to induce or augment labor, manage postpartum hemorrhage, and facilitate uterine evacuation in cases of incomplete abortion or fetal death. They are also employed as abortifacients to induce abortion.
Oxytocics
Oxytocics are drugs that stimulate uterine contractions, mimicking the action of the natural hormone oxytocin. They are used to induce or augment labor, control postpartum bleeding, and in some cases, manage incomplete or missed abortions.
Types of Oxytocics

Oxytocin (Pitocin, Syntocinon)
- Legal Class: Class B controlled drugs
- Medical Class: Oxytocic drugs
- Form: Sterile solution for injection
- Strength: 10 IU per ampule
Indications of Oxytocin:
- Induction of Labor: When labor is not progressing naturally.
- Augmentation of Labor: To strengthen contractions when labor is slow or stalled.
- Control of Postpartum Bleeding (PPH): To contract the uterus after delivery and prevent excessive bleeding.
- Active Management of the Third Stage of Labor: To help deliver the placenta and reduce the risk of PPH.
Others include;
- Management of hypotonic uterine contractions
- Treatment of intrauterine fetal death
- Prevention and treatment of postpartum hemorrhage (PPH)
- Active management of the third stage of labor
- Management of preeclampsia and eclampsia
- Treatment of congestive heart failure secondary to fluid overload in pregnancy
- Management of post-term pregnancies
- Incomplete or missed abortion
Contraindications of Oxytocin.
- Hypertonic Uterine Contractions: When the uterus is already contracting too strongly.
- Fetal and Maternal Distress: When the baby or mother is experiencing complications.
- Multiple Pregnancy: Increased risk of complications.
- Trial of Labor: When a woman is attempting a vaginal delivery after a previous Cesarean section.
- Malpresentation: When the baby is in a position that makes vaginal delivery difficult (e.g., breech, brow).
- Cephalo Pelvic Disproportion: When the baby’s head is too large to fit through the mother’s pelvis.
- Low Blood Pressure: Oxytocin can further lower blood pressure.
Dosage of Oxytocin
- Induction/Augmentation of Labor: 5 IU in 500 mL of IV infusion, initially at 5 drops per minute, titrated as needed.
- Prevention of PPH: 5 IU slow IV injection after delivery of the placenta, with an increase in rate if necessary during the third stage of labor.
- PPH: 10 unit IM after delivery of placenta
Routes of Administration:
- Intramuscular (IM)
- Intravenous (IV), often in combination with normal saline or dextrose
Side Effects of Oxytocin
- Dizziness
- Nausea and vomiting
- Skin rashes
- Fetal bradycardia
- Hypotension
Adverse Effects:
- Uterine rupture, particularly in cases of hyperstimulation
- Severe hypotension
- Tachycardia
- Fetal anoxia and hypoxia leading to birth asphyxia
Pharmacokinetics:
- Absorption: Rapid following IV injection
- Distribution: Distributed throughout the extracellular fluid, with some crossing into fetal circulation
- Metabolism: Primarily in the liver and kidneys, with rapid metabolism and excretion in the urine

Syntometrine
Syntometrine is a combination drug containing both ergometrine and oxytocin, designed to provide a synergistic effect in controlling postpartum bleeding.
- Legal Class: Class B controlled drug
- Medical Class: Oxytocic drug
- Form: Sterile solution for injection
- Strength: Combination of ergometrine 0.5 mg + oxytocin 5 IU (International Units)
- Dosage: 1 mL as a single dose, but can be repeated if necessary if bleeding is not controlled.
Route:
- Intramuscular: Injection into a muscle.
- Intravenous: Injection into a vein.
Indications:
- Multigravidas: Women who have had multiple pregnancies, as they are at higher risk for PPH.
- History of Postpartum Hemorrhage: Women with a previous history of PPH.
- Multiple or Twin Delivery: Due to the larger placental site.
- Heavy Lochia: Excessive vaginal discharge after delivery.
- Abortion: When the fundal height (measurement of the uterus) is less than 12 weeks.
Contraindications:
- Cardiac Disease: Syntometrine can worsen heart conditions.
- Preeclampsia and Eclampsia: Syntometrine can exacerbate these conditions.
- Hypertension: Syntometrine can raise blood pressure.
Adverse Effects:
- Retained Placenta: The placenta may not be fully expelled.
- IUFD (Intrauterine Fetal Death) in Undiagnosed Second Twin: If a second twin is present and undiagnosed, Syntometrine can lead to its death.
- Retained Second Twin: The second twin may not be fully expelled.
- Uterine Rupture: If given during abortion after 20 weeks of gestation, especially if the products of conception are not fully expelled.
- Hypoxia and Anoxia: Lack of oxygen to the fetus or mother.
Side Effects:
- Nausea and Vomiting
- Headache
- Hypotension: Low blood pressure.
- Dyspnea: Difficulty breathing.
- Muscle Pain

Ergometrine
Ergometrine is a potent oxytocic that acts directly on the uterine muscle to cause sustained contractions.
Legal Class: Class B controlled drug
Medical Class: Oxytocic drug
Form: Tablet and sterile solution
Strength/Dosage:
- Tablets: 0.25 to 0.5 mg
- Injection: 200 mcg/mL or 0.5 mg/mL
Effects: Causes sudden, prolonged, intermittent uterine contractions.
Indications: Similar to Syntometrine, primarily used to control postpartum bleeding.
Contraindications: Similar to Syntometrine.
Side Effects: Similar to Syntometrine.
Dangers: Similar to Syntometrine.

Indomethacin (An NSAID)
Legal Class: Prescription-only medication
Medical Class: NSAID, tocolytic
Form: Tablets, rectal suppositories, oral suspension
Mechanism of Action
Indomethacin inhibits the cyclooxygenase (COX) enzymes, leading to reduced synthesis of prostaglandins, which are crucial for uterine contractions.
Dosage
- Preterm labor: 50-100 mg rectally or orally, followed by 25-50 mg every 6-8 hours. The treatment duration is limited to 48 hours to minimize fetal side effects.
Indications
- Preterm labor (especially when caused by polyhydramnios)
- Patent ductus arteriosus (PDA) closure in neonates
Contraindications
- Fetal distress
- Intrauterine fetal death
- Peptic ulcer disease
- Renal impairment
- Bleeding disorders
Side Effects
- Gastrointestinal discomfort (nausea, vomiting, epigastric pain)
- Dizziness and headache
- Rash
Adverse Effects
- Oligohydramnios (reduced amniotic fluid)
- Premature closure of the ductus arteriosus in the fetus
- Renal impairment in both mother and fetus
Abortifacients
Abortifacients are drugs that induce abortion by causing strong uterine contractions, leading to the expulsion of uterine contents. They are often used in the first and second trimesters of pregnancy for medical termination, and are often used in conjunction with other medications.
Types of Abortifacients

Misoprostol
- Legal Class: Class B controlled drugs
- Medical Class: Oxytocic drugs/Cervical ripening agent
- Form: Tablets
- Strength: 100 mcg or 200 mcg per tablet
Indications of Misoprostol:
- Induction of Labor: When labor is not progressing naturally.
- Control of Postpartum Hemorrhage: Due to uterine atony.
- Cervical Ripening: To soften the cervix before labor induction.
- Intrauterine Fetal Death: To induce labor and expel the fetus.
- Gastric and Duodenal Ulcerations: Off-label use for treating ulcers.
- Medical termination of pregnancy in combination with mifepristone
Contraindications of Misoprostol:
- Malpresentation: When the baby is in a position that makes vaginal delivery difficult.
- Placenta Previa Grade 3 and 4: When the placenta is covering the cervix.
- Multiparous Mothers: Increased risk of complications.
- Cephalo Pelvic Disproportion: When the baby’s head is too large to fit through the mother’s pelvis.
- Hypersensitivity to Misoprostol: Allergic reaction.
Dosage of Misoprostol:
- Induction of Labor: 25-50 mcg vaginally every 4-6 hours until adequate uterine contractions are achieved
- NSAID-Induced Ulceration: 200 mcg orally four times daily
Routes of Administration:
- Sublingual: Under the tongue.
- Rectal: Inserted into the rectum.
- Vaginal: Inserted into the vagina.
- Oral: Swallowed
Side Effects:
- Headache
- Dizziness
- Fever and shivering
- Nausea and vomiting
- Uterine rupture (rare but serious)
Adverse Effects:
- Fetal distress and bradycardia
- Uterine hyperstimulation leading to rupture
- Severe gastrointestinal disturbances
Pharmacokinetics:
- Absorption: Rapidly absorbed after oral, sublingual, or vaginal administration
- Distribution: Well distributed throughout the body, crossing into fetal circulation
- Metabolism: Hepatically metabolized to active prostaglandin analogs
- Excretion: Primarily excreted in urine.
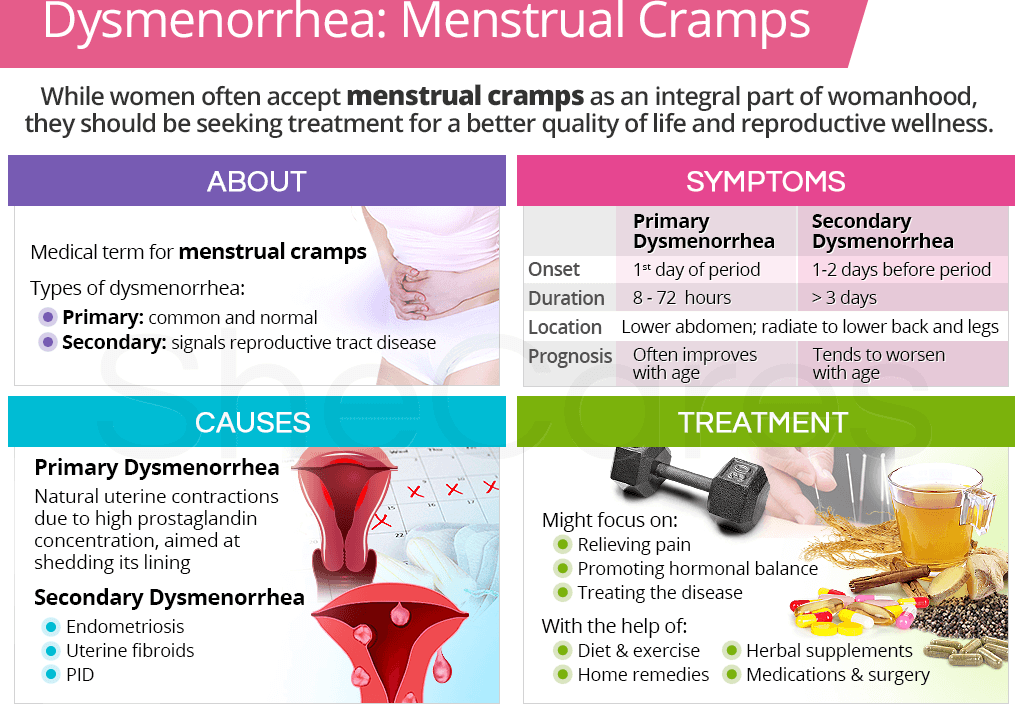
Dysmenorrhea: Drug Treatment
Dysmenorrhoea refers to pain during menstruation, caused by excessive prostaglandin production, leading to strong uterine contractions.
Dysmenorrhea, or painful menstruation, is categorized into primary and secondary types, based on the presence or absence of an identifiable underlying cause.
I. Primary Dysmenorrhea:
- Cause: Unknown; believed to be related to excessive prostaglandin production leading to intense uterine contractions.
- Risk Factors: Early menarche, heavy menstrual bleeding, family history of dysmenorrhea, smoking.
- Signs and Symptoms: Cramping abdominal pain, headache, nausea/vomiting, diarrhea, lower back pain, loss of appetite.
- Non-Pharmacological Management: Regular exercise, hot water bottles/warm baths, adequate rest and sleep, back massage, low-fat diet, nutritional supplements (Vitamin E, zinc, Vitamin B1). Educate the patient that the condition isn’t a gynecological abnormality.
- Pharmacological Management:
- Non-Steroidal Anti-inflammatory Drugs (NSAIDs): Reduce prostaglandin production. Start 1-2 days before anticipated menstruation for optimal effectiveness.
- Mefenamic acid: 500mg three times daily for 3-4 days.
- Ibuprofen: 400mg three times daily for 3-4 days.
- Indomethacin: 50mg three times daily for 3-4 days.
- Diclofenac: 50mg three times daily for 3-4 days.
- Aceclofenac: 100mg twice daily for 3-4 days. (Note: The provided text lists 10mg, but 100mg is a more common and appropriate dosage.)
- Hormonal Therapy: Used if NSAIDs are ineffective. These suppress ovulation, reducing prostaglandin production.
- Combined Oral Contraceptives (COCs): Examples include Pilplan and Microgynon.
- Norethisterone (Primolut-N): A progestogen.
- Antispasmodics: Relax uterine smooth muscle, providing relief from spasms. May be used alone or in combination with NSAIDs for severe cases.
- Drotaverine (Nospa): 80mg three times daily for 3 days.
II. Secondary Dysmenorrhea:
- Cause: Identifiable underlying condition, such as: pelvic inflammatory disease (PID), endometriosis, fibroids, ovarian cysts, intrauterine devices (IUDs).
- Signs and Symptoms: Abdominal bloating, backache, pain starting 3-5 days before menstruation, pain during sexual intercourse.
- Management: Treatment focuses on addressing the underlying cause. NSAIDs may provide temporary pain relief while the underlying condition is treated.
Others;
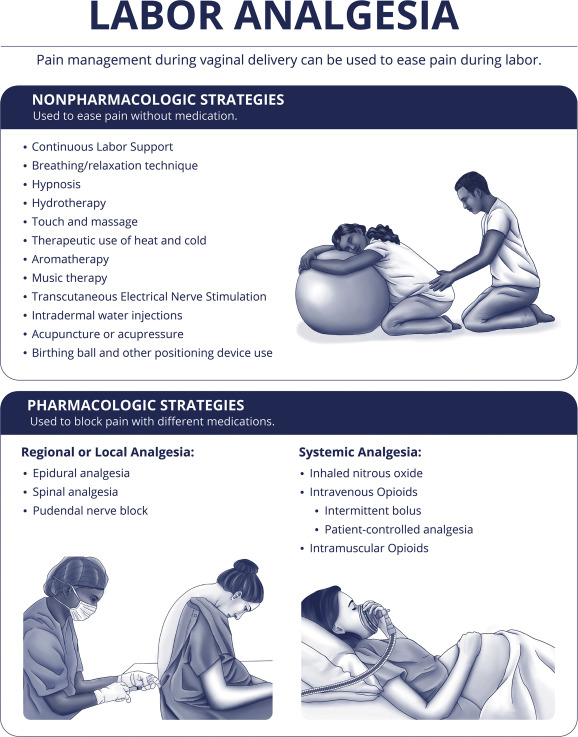
Analgesics and Anesthetics for Labor Pain
Purpose: Provide pain relief during labor and delivery.
Examples:
Epidural Anesthesia:
- Mechanism: Local anesthetics (e.g., bupivacaine) injected into the epidural space to block pain signals.
- Indications: Pain relief during labor.
- Administration: Continuous infusion via epidural catheter.
Nitrous Oxide:
- Mechanism: Inhaled analgesic that provides mild pain relief.
- Indications: Labor pain.
- Administration: Inhalation.
Opioids:
- Mechanism: Bind to opioid receptors in the brain to reduce pain perception.
- Examples: Fentanyl, Remifentanil.
- Indications: Moderate to severe labor pain.
- Administration: IV or IM.
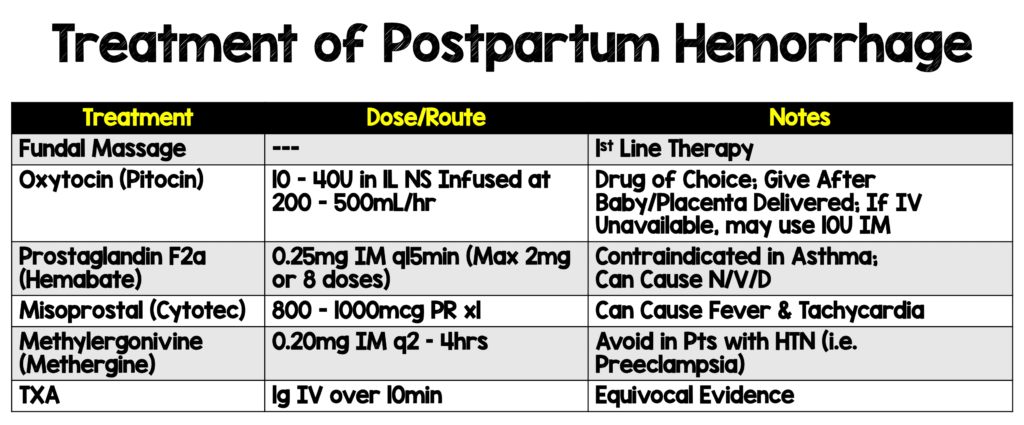
Drugs for Postpartum Hemorrhage (PPH)
Purpose: Prevent or treat excessive bleeding after delivery.
Examples:
Oxytocin:
- Mechanism: Stimulates uterine contractions to reduce bleeding.
- Indications: First-line treatment for PPH.
- Administration: IV or IM.
- Dosage: 10-40U in 1L normal saline infused at 200-500mL/hr.
Misoprostol:
- Mechanism: Induces uterine contractions.
- Indications: PPH, especially in resource-limited settings.
- Administration: Oral, sublingual, or rectal.
- Dosage: 800-1000 mcg PR(Per Rectal) once.
Carboprost:
A medication used after the delivery of a baby to control bleeding from the uterus that has not resolved with other treatments.
- Mechanism: Strong uterine contractor.
- Indications: PPH unresponsive to oxytocin.
- Administration: IM.
Tranexamic Acid:
A medication used to control episodes of heavy bleeding.
- Mechanism: Antifibrinolytic that reduces bleeding.
- Indications: PPH.
- Administration: IV.
- Dosage: 1g over 10 minutes
Rh Immunoglobulin :
A medication used to prevent unwanted immune reactions in blood transfusions or pregnancy.
Human Rho(D) immune globulin is a solution of antibodies used to prevent isoimmunization of Rho(D) negative patients exposed to Rho(D) positive blood in pregnancy or transfusion.
- Purpose: Prevent Rh sensitization in Rh-negative mothers.
- Mechanism: Prevents the mother’s immune system from producing antibodies against Rh-positive fetal blood cells.
- Indications: Rh-negative mothers with Rh-positive babies.
- Administration: IM, usually at 28 weeks of pregnancy and within 72 hours of delivery.

Antiemetics for Nausea and Vomiting in Pregnancy
Purpose: Manage nausea and vomiting, including hyperemesis gravidarum.
Examples:
First-Line Pharmacotherapy:
This is the initial treatment approach. Two options are presented:
Pyridoxine (Vitamin B6)
- Dosage: 10-25mg orally every 6-8 hours: This is a common first-line treatment for mild NVP.
Doxylamine + Pyridoxine:
This combination therapy is often more effective than pyridoxine alone, particularly for moderate NVP.
- Mechanism: Antihistamine and vitamin B6 combination.
- Indications: Nausea and vomiting in pregnancy.
- Administration: Oral.
If symptoms persist despite first-line treatment and dehydration occurs, proceed to:
Second-Line Pharmacotherapy:
This stage involves intravenous (IV) fluid resuscitation to correct dehydration in addition to one of the following antiemetic medications given intravenously:
Metoclopramide
- Dosage: 5-10 mg every 8 hours: This medication stimulates gastric motility and can help with nausea.
Ondansetron:
- Mechanism: Serotonin 5-HT3 receptor antagonist.
- Indications: Severe nausea and vomiting.
- Administration: 8mg every 12 hours, Oral or IV.
Promethazine
- Dosage: 12.5-25mg every 4-6 hours: An antihistamine with antiemetic properties.
If vomiting remains uncontrolled (“refractory vomiting”) despite second-line therapy, proceed to:
Third-Line Pharmacotherapy:
This is reserved for severe, persistent cases. Again, IV fluid resuscitation is crucial, and one of the following medications is added:
Methylprednisolone
- Dosage: 16mg every 8 hours orally or intravenously for 3 days (tapering over 2 weeks, continuing for a total of 6 weeks if effective): A corticosteroid with potent anti-inflammatory and antiemetic effects. The tapering schedule is crucial to minimize side effects.
Chlorpromazine
- Dosage: 25-50mg intravenously or intramuscularly every 4-6 hours: A phenothiazine derivative with antiemetic and sedative properties. Use cautiously due to side effects.
Chlorpromazine
- Dosage: 10-25mg orally every 4-6 hours: Oral alternative to the IV/IM route.
Corticosteroids for Fetal Lung Maturation
Purpose: Accelerate fetal lung development in preterm labor.
Examples:
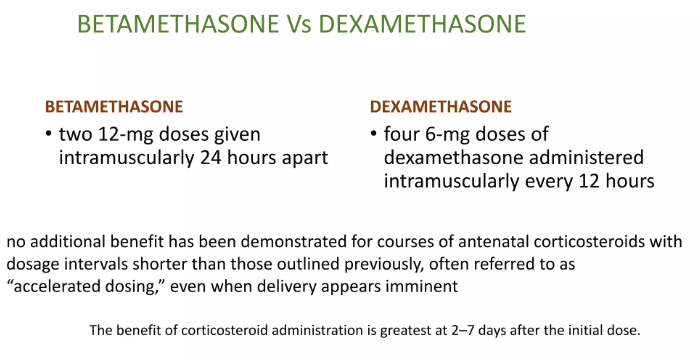
Betamethasone:
- Mechanism: Stimulates surfactant production in fetal lungs.
- Indications: Preterm labor (24–34 weeks gestation).
- Administration: Two 12 mg doses given IM 24 hours apart.
Dexamethasone:
- Mechanism: Similar to betamethasone.
- Indications: Preterm labor.
- Administration: Four 6 mg doses given IM every 12 hours.
Iron and Folic Acid Supplements
- Purpose: Prevent or treat anemia during pregnancy.
- Mechanism: Supports red blood cell production and fetal development.
- Indications: Routine supplementation during pregnancy.
- Administration: Oral.
Drugs for Hypertension in Pregnancy
Hypertension in pregnancy is a serious condition requiring careful management due to potential risks to both mother and fetus.
Types of Hypertension in Pregnancy:
- Chronic Hypertension: This pre-existing condition is diagnosed before pregnancy or before 20 weeks gestation.
- Gestational Hypertension: Onset occurs after 20 weeks of gestation and resolves postpartum. It’s characterized by elevated blood pressure without proteinuria (protein in the urine).
- Pre-eclampsia: A more serious condition, diagnosed after 20 weeks gestation. It involves hypertension with proteinuria, often accompanied by other symptoms like edema (swelling), headaches, visual disturbances, and abdominal pain.
- Eclampsia: The most severe form, characterized by seizures in a woman with pre-eclampsia. This is a life-threatening emergency requiring immediate medical intervention.
Management Strategies:
Treatment depends heavily on the type and severity of hypertension and the presence of complications. The primary goals are to prevent seizures, reduce blood pressure to a safe level, and deliver the baby at an appropriate time.
Anticonvulsants (Primarily for Eclampsia):
Magnesium Sulfate: This is the first-line treatment for eclampsia to prevent seizures.
- Dosage: A loading dose of 4g intravenously (IV) is administered over 10-15 minutes, followed by a maintenance dose of 10g intramuscularly (IM), typically divided into two 5g injections (one in each buttock). Continuous monitoring of magnesium levels is essential to prevent toxicity.
- Toxicity Management: Calcium gluconate 1-2g IV is the antidote for magnesium sulfate toxicity. Symptoms of toxicity include decreased deep tendon reflexes, respiratory depression, and cardiac arrhythmias.
Diazepam: Used for immediate seizure control in eclampsia, although it’s not the primary preventative agent like magnesium sulfate. Diazepam 10mg IV is usually administered.
Antihypertensives:
The choice of antihypertensive medication depends on several factors, including the type of hypertension, severity of blood pressure elevation, and the presence of any co-existing conditions. The goal is to gradually lower blood pressure to avoid sudden drops that could compromise placental perfusion.
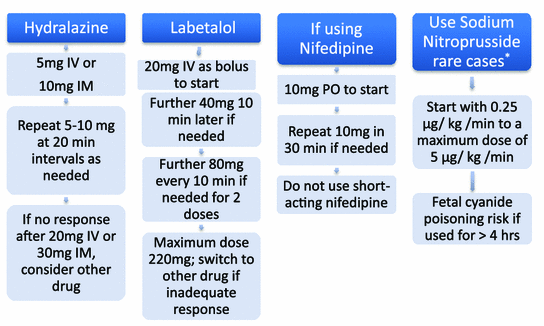
Severe Hypertension (Emergency):
- Hydralazine 5-10mg IV: A vasodilator that acts quickly to lower blood pressure. Careful monitoring is essential due to its potential side effects.
- Nifedipine 20mg sublingual: A calcium channel blocker with rapid-onset action. It’s typically given sublingually for fast-acting effects in hypertensive emergencies.
Chronic Hypertension (Non-Emergency):
- Methyldopa 250mg twice daily to three times daily: A centrally acting alpha-2 agonist that is generally considered safe in pregnancy. The dosage is adjusted based on blood pressure response.
- Nifedipine retard 20mg twice daily: A long-acting calcium channel blocker that offers sustained blood pressure control. Again, dose adjustments are necessary based on clinical monitoring.
ANTIMALARIAL DRUGS
Malaria is an acute febrile illness caused by protozoa of the genus Plasmodium. It is transmitted from person to person through the bite of a female Anopheles mosquito.
The Four Species of Malaria Parasites:
- Plasmodium falciparum
- Plasmodium vivax
- Plasmodium ovale
- Plasmodium malariae
Life Cycle of Malaria Parasites
Malaria parasites undergo both a sexual cycle (in the female Anopheles mosquito) and an asexual cycle (in humans).
- Mosquito Bite: The mosquito injects sexual forms of the parasite (sporozoites) into the bloodstream.
- Hepatic Cycle: Sporozoites enter liver cells, forming tissue schizonts, which rupture and release merozoites. Some sporozoites become dormant forms (hypnozoites), which may reactivate later.
- Erythrocytic Cycle: Merozoites invade red blood cells (RBCs), forming blood schizonts. The schizonts rupture the RBCs, causing the clinical symptoms of malaria.
- Gametocyte Formation: Some merozoites develop into male and female gametocytes. If taken up by a mosquito, they complete the life cycle, forming sporozoites.
Classification of Antimalarial Drugs
Classification I
- Tissue Schizonticides: Act on malaria parasites in the liver (Primaquine, Pyrimethamine, Proguanil).
- Blood Schizonticides: Act on schizonts in RBCs (Chloroquine, Amodiaquine, Proguanil, Pyrimethamine, Mefloquine, Quinine, Artemisinin).
- Gametocides: Prevent transmission by destroying gametocytes (Primaquine).
Classification II
- 4-Aminoquinolines: Chloroquine, Amodiaquine
- 8-Aminoquinolines: Primaquine
- 4-Methanolquinolines (Quinoline Methanols): Quinine, Mefloquine
- Biguanides: Proguanil
- Sulphonamides: Sulfadoxine
- Artemisinin Derivatives: Artemether, Artesunate, Dihydroartemisinin, Artemisinin
- Antibiotics: Doxycycline, Tetracycline, Clindamycin
QUININE
- Type: Alkaloid derived from the bark of the cinchona tree.
- Classification: 4-Methanolquinoline
- Action: Rapid blood schizonticide active against Plasmodium falciparum, vivax, ovale, malariae.
- Mechanism: Inhibits haem polymerase, preventing the polymerization of haem to haemozoin.
Available Preparations:
- Tablets 300 mg
- Injection 300 mg/ml
- Syrup 100 mg/5 ml
Pharmacokinetics:
- Absorbed from the gastrointestinal tract, widely distributed, metabolized in the liver, excreted mainly in urine.
Indications:
- Uncomplicated and severe malaria.
Dosage:
- Oral: Adults 600 mg 8-hourly for 7 days.
- IV: Adults 600 mg 8-hourly in dextrose 5%, to run for 4 hours.
- Children: 10 mg/kg 8-hourly for 7 days (oral), or same dose IV in dextrose.
Contraindications:
- Hypersensitivity, cardiac abnormalities (e.g., AV block), myasthenia gravis, haemoglobinuria, visual/auditory problems.
Side Effects:
- Headache, blurred vision, abdominal pain, diarrhea, tinnitus, hypersensitivity reactions, nausea, hypoglycemia, “cinchonism” (tinnitus, dizziness, visual disturbances).
Drug Interactions:
- Increases digoxin and warfarin levels.
- Delayed absorption with aluminum antacids.
- Cimetidine increases quinine blood levels.
SULFADOXINE WITH PYRIMETHAMINE (FANSIDAR)
- Action: Synergistically inhibit folic acid synthesis in parasites.
- Available Preparations: Tablets (500 mg sulfadoxine/25 mg pyrimethamine).
Pharmacokinetics:
- Well absorbed, widely distributed, metabolized in the liver, and slowly excreted.
Indications:
- Malaria prophylaxis and intermittent presumptive treatment (IPT) in pregnancy.
Dosage:
- IPT in Pregnancy: 3 tablets during 2nd and 3rd trimesters.
Contraindications:
- Hypersensitivity, severe renal failure, infants < 2 months, first trimester pregnancy.
Side Effects:
- Urticaria, vomiting, diarrhea, nausea, headache, Stevens-Johnson syndrome.
Drug Interactions:
- Increased antifolate effect with methotrexate and cotrimoxazole, raises phenytoin plasma concentration.
ARTEMISININ AND DERIVATIVES
- Derived from Artemesia annua (Chinese herb Qinghaosu).
- Action: Rapidly acting blood schizonticides effective against multidrug-resistant Plasmodium falciparum.
- Derivatives: Artesunate (water-soluble), Artemether (lipid-soluble).
Artemether:
- Available Forms: Injection (20 mg/ml, 40 mg/ml, 80 mg/ml).
- Indications: Uncomplicated and severe malaria.
- Dose: Adults 300 mg loading dose, followed by 100 mg once daily for 4 days.
Side Effects:
- Nausea, vomiting, diarrhea, dizziness, tinnitus.
Contraindications:
- Hypersensitivity, first trimester of pregnancy.
ARTEMETHER + LUMEFANTRINE
- Available Forms: Tablets (20 mg/120 mg, 40 mg/240 mg), suspension (15 mg/90 mg/5 ml).
- Indications: First-line treatment for uncomplicated malaria.
Dosage:
Weight | Age | Day 1 | Day 2 | Day 3 |
5-14 kg | 4 months-3 yrs | 1 tablet 12-hourly | 1 tablet 12-hourly | 1 tablet 12-hourly |
15-24 kg | 3-7 yrs | 2 tablets 12-hourly | 2 tablets 12-hourly | 2 tablets 12-hourly |
25-34 kg | 7-12 yrs | 3 tablets 12-hourly | 3 tablets 12-hourly | 3 tablets 12-hourly |
≥35 kg | 12+ yrs | 4 tablets 12-hourly | 4 tablets 12-hourly | 4 tablets 12-hourly |
Contraindications:
- Cardiac arrhythmias, bradycardia, breastfeeding.
Side Effects:
- Abdominal pain, diarrhea, nausea, headache, fatigue, skin rash.
Drug Interactions:
Avoid concurrent use with amiodarone, ciprofloxacin, fluconazole, mefloquine.
ARTESUNATE
Type: Derivative of artemisinin, water-soluble.
Classification: Blood schizonticide and gametocide, particularly effective against Plasmodium falciparum, including multidrug-resistant strains.
Mechanism of Action: Artesunate is a prodrug that is rapidly converted to dihydroartemisinin, its active form. It works by producing free radicals within the parasite’s food vacuole, leading to the destruction of the parasite.
Available Preparations:
- Tablets: 50 mg, 100 mg
- Injection: 60 mg vial (for intravenous and intramuscular use)
Pharmacokinetics:
- Rapidly absorbed
- Widely distributed in body tissues
- Metabolized in the liver to dihydroartemisinin
- Excreted mainly in urine
Indications:
- Severe and complicated malaria
- Uncomplicated malaria (especially when caused by Plasmodium falciparum resistant to other drugs)
Dosage:
- Severe malaria: Initial IV dose of 2.4 mg/kg at 0, 12, and 24 hours, then once daily.
- Uncomplicated malaria: 4 mg/kg once daily for 3 days (used in combination therapy).
Contraindications:
- Known hypersensitivity to artemisinin derivatives.
- First trimester of pregnancy (unless the benefits outweigh the risks).
Side Effects:
- Nausea
- Vomiting
- Dizziness
- Diarrhea
- Low neutrophil count (rare)
- Injection site reactions (for IV/IM administration)
Drug Interactions:
- Caution with drugs affecting the heart’s electrical activity (e.g., antiarrhythmics like amiodarone).
- Avoid concurrent use with drugs that prolong QT interval (e.g., quinidine, erythromycin).


l want to know about supplements like ferrous sulfate and follic acid
it’s so good and useful l have gained out of it