Table of Contents
ToggleCommunity Health & Tropical Medicine UNMEB Past Papers ✨
Prepared by Nurses Revision! Let's dive in! 😊
Paper 1 - Section A: Objective Questions (MCQs)
1. Which of the following priority areas should a Primary Health Care program focus on?
- (a) Personal hygiene and sanitation.
- (b) Punishing all thieves.
- (c) Having local council meetings.
- (d) Creating a link between two parties.
Why other options are wrong:
- (b) Punishing thieves: This is important for law and order, but not a health priority area for a health program. That's a job for the police and courts.
- (c) Having local council meetings: While local councils are important and can support health programs, the meetings themselves aren't a direct health priority area. They are a way to organize the community.
- (d) Creating a link between two parties: This is too general. PHC involves working with many groups, but the core focus is on health activities, not just any kind of link.
2. Which of the following is NOT a pillar of Primary Health Care?
- (a) Inter sectoral collaboration.
- (b) Community participation.
- (c) Appropriate technology.
- (d) Accessibility of services.
Why other options are (usually) pillars:
- (a) Inter sectoral collaboration: Absolutely a pillar. Health needs help from education, agriculture, water, etc.
- (b) Community participation: Essential pillar. PHC is not done *for* the community, but *with* them.
- (c) Appropriate technology: Key pillar. Using tools and methods that the community can afford and manage.
3. The major aim of health education in Primary Health Care activities is to
- (a) provide appropriate care to the community.
- (b) improve health of the community.
- (c) meet the needs of the cornmunity.
- (d) make a health plan for the future.
Why other options are wrong:
- (a) provide appropriate care: Health education helps people seek care and manage conditions, but it's not the *provision* of care itself (like giving medicine or treatment).
- (c) meet the needs of the community: Health education helps address health needs, but the *major aim* is the positive outcome on health status. Meeting needs is broader than just education.
- (d) make a health plan for the future: Making plans is a separate activity, often done by health professionals and community leaders. Education helps inform the plan and get support, but isn't the planning itself.
4. Which of the following factors promote community mobilisation?
- (a) Political interest.
- (b) Appropriate language.
- (c) Past bad experience.
- (d) Poor relationship.
Why other options are wrong:
- (a) Political interest: While political *support* can help, political *interest* alone doesn't guarantee the community will mobilize. It's an external factor that might help but isn't a direct *promoter* from within or in the interaction.
- (c) Past bad experience: This would definitely *hinder* mobilisation, not promote it. People would be hesitant to join if previous efforts failed or were negative.
- (d) Poor relationship: Like bad experiences, poor relationships between health workers and the community, or among community members, will make it harder to mobilize people.
5. Which of the following best explains a community based health program?
- (a) The community is involved in planning and implementation.
- (b) There is no outside assistance given in running community programs.
- (c) Only members of the community are given offices.
- (d) Offers training to the community members.
Why other options are wrong:
- (b) There is no outside assistance: Community-based doesn't mean isolated. Outside help (from government, NGOs, etc.) is often needed, but the key is the community's *central role*, not the absence of others.
- (c) Only members of the community are given offices: While community members often take leadership roles, this isn't the *defining* feature. The involvement in planning and doing the work is the core idea.
- (d) Offers training to the community members: Training is a common activity in community-based programs to build capacity, but it's a *part* of implementation, not the best explanation of the overall concept.
6. Which of the following is NOT a characteristic of a Primary Health Care practical approach?
- (a) Have social development dimensions.
- (b) Acceptable and affordable.
- (c) Making essential health care universally accessible.
- (d) Should not be determined by social goals.
Why other options are characteristics:
- (a) Have social development dimensions: Yes, PHC recognizes that health is linked to things like education, income, and equality (social development).
- (b) Acceptable and affordable: Yes, for PHC to be practical and used by the community, it must be acceptable (culturally right) and affordable (people can pay for it).
- (c) Making essential health care universally accessible: Yes, a core goal is that basic health services are available to everyone, no matter where they live or how much money they have.
7. Which of the following indicates the need for community participation?
- (a) Soliciting for external support.
- (b) Clear understanding of the project goal.
- (c) Good leadership and administration.
- (d) Self reliance in the set up projects.
Why other options are wrong:
- (a) Soliciting for external support: External support might be needed, but the *need* for participation is more about empowering the community itself, not just getting funds from outside.
- (b) Clear understanding of the project goal: A clear understanding is important for *effective* participation, but the *need* for participation exists even if understanding is initially low; participation helps *build* that understanding.
- (c) Good leadership and administration: Good leadership *facilitates* participation, but it's not the *reason* we need participation. The need comes from wanting the community to own and manage the initiative.
8. Which of the following is NOT a concept of equity?
- (a) Justice.
- (b) Fairness.
- (c) Inequality.
- (d) Equality.
Why other options are related to equity:
- (a) Justice: Equity is a fundamental aspect of social justice in health.
- (b) Fairness: Equity is essentially about fairness in health opportunities and outcomes.
- (d) Equality: While equity is not always the same as giving everyone an *equal amount* of resources, the goal of equity is to achieve greater equality in health outcomes by addressing different needs. It's related, though equity is often seen as the *means* to achieve equality in health.
9. The process of enabling people increase control over the determinants of health and thereby improve their own health is
- (a) health education.
- (b) health promotion.
- (c) health prevention.
- (d) health care.
Why other options are wrong:
- (a) health education: This is an important *tool* used in health promotion, but health promotion is broader than just giving information.
- (c) health prevention: This is about preventing diseases (e.g., vaccination, hygiene). It's a goal that health promotion helps achieve, but health promotion is the process of empowering people.
- (d) health care: This is about treating people who are already sick or injured. Health promotion focuses on keeping people well and addressing the root causes of ill health.
10. Which of the following factors of health does NOT affect the community?
- (a) Life style.
- (b) Environment.
- (c) Health services provision.
- (d) Empowerment.
Why other options ARE factors affecting community health:
- (a) Life style: Community health is the sum of individual healths, and lifestyle choices cluster within communities.
- (b) Environment: The physical and social environment (housing, sanitation, safety, social support) directly impacts community health.
- (c) Health services provision: Access to quality health services is a major determinant of community health outcomes.
11. Which of the following is the best way to make a community diagnosis?
- (a) Attend village gatherings to get information.
- (b) Carryout home visits in the community.
- (c) Look at existing medical records.
- (d) Talk to village leaders and health workers.
Why other options are useful but not the "best" single way:
- (b) Carryout home visits: Gives detailed info about individual families, but is time-consuming and doesn't give the full community picture.
- (c) Look at existing medical records: Provides clinical data on diseases seen at facilities, but misses many community-level issues, social determinants, and people who don't use facilities.
- (d) Talk to village leaders and health workers: Provides important key informant perspectives, but is limited to their view and might miss the voices of ordinary community members.
12. Nurses should assess the health status of a given population at a particular time through
- (a) community mobilisation.
- (b) clinical diagnosis.
- (c) community participation.
- (d) community diagnosis.
Why other options are wrong:
- (a) community mobilisation: This is the process of getting the community together to take action, not an assessment method.
- (b) clinical diagnosis: This is diagnosing illness in *one* person, not a whole population.
- (c) community participation: This is the community being involved in health activities, not a method for assessing their health status.
13. Which of the following types of prevention should be implemented when a person is in a healthy state?
- (a) Quaternary.
- (b) Secondary.
- (c) Primary.
- (d) Tertiary.
Why other options are wrong:
- (a) Quaternary: This is about preventing over-medicalization (too much treatment or testing).
- (b) Secondary: This is about detecting a disease *early* when a person might not even have symptoms yet (e.g., screening for high blood pressure).
- (d) Tertiary: This is about managing an existing disease to prevent complications, disability, or death (e.g., rehabilitation after a stroke, managing diabetes).
14. An approach that stimulates the community to initiate and maintain the running of health activities at its own cost is called
- (a) self reliance.
- (b) sustainability.
- (c) participation.
- (d) appropriate technology.
Why other options are wrong:
- (b) sustainability: This means the program continues over time, which self-reliance helps achieve, but self-reliance is the *means* (doing it themselves, perhaps at their cost) to achieve sustainability.
- (c) participation: This is the involvement of people, which is necessary for self-reliance and sustainability, but not the term for initiating and maintaining *at their own cost*.
- (d) appropriate technology: This is about using suitable tools, which helps self-reliance, but isn't the approach of doing it *at their own cost*.
15. An initiative by community members to look for locally available solutions for their health problems is termed as
- (a) community mobilisation.
- (b) community active participation.
- (c) top-down approach.
- (d) bottom-up approach.
Why other options are wrong:
- (a) community mobilisation: This is the *process* of getting people together, which is part of a bottom-up approach, but not the term for the *initiative* of seeking local solutions.
- (b) community active participation: This is the *level* of involvement, which is high in a bottom-up approach, but not the term for the *approach* of seeking local solutions.
- (c) top-down approach: This is the opposite; solutions come from outside, not locally from within the community.
16. Which of the following is defined as a collection of people identified by a set of shared values?
- (a) Family.
- (b) Society.
- (c) Community.
- (d) Communal village.
Why other options are wrong:
- (a) Family: A family is a small unit, while a community is usually larger.
- (b) Society: Society is a very broad term for a large group of people living in the same territory, not necessarily defined by a specific set of *shared values* in the way a community is.
- (d) Communal village: This is a specific type of community (geographically defined), but the definition provided (shared values) also applies to communities not based purely on location (like a community of people living with diabetes, or a religious community). "Community" is the general term.
17. The step of action where members identify their health needs, prioritize and plan their health activities is community
- (a) organisation.
- (b) diagnosis.
- (c) participation.
- (d) mobilisation.
Why other options are related but not the direct action step:
- (a) organisation: Community organisation is the process of building the structure and capacity for participation, but identifying/prioritizing/planning is the *activity* the organized group does.
- (b) diagnosis: Community diagnosis is the *outcome* or *result* of identifying needs, not the action of the members doing it.
- (d) mobilisation: This is getting people ready and together, but identifying/prioritizing/planning are specific activities that happen *after* or *during* mobilisation and organisation.
18. A health worker's ability to create interdependent relationships with individuals, groups and organisations to accomplish mutually set objectives is
- (a) coalition building.
- (b) networking.
- (c) empowerment.
- (d) development.
Why other options are related but different:
- (b) networking: This is building relationships in general, which is a necessary step before building a coalition, but coalition building is more formal and focused on achieving shared goals.
- (c) empowerment: This is about enabling others to gain control and power, which might be an outcome or a process within coalition building, but not the definition of creating the relationships themselves.
- (d) development: This is a broad term for progress and improvement, which coalition building can contribute to, but it's not the specific term for forming the relationships for objectives.
19. The following are both principles and pillars of primary healthcare
- (a) sustainability.
- (b) prioritisation and efficiency.
- (c) equity and affordability.
- (d) appropriate technology and equity.
Why other options are wrong:
- (a) sustainability: This is a very important *goal* or *outcome* of PHC, but not usually listed as one of the foundational *pillars* or *principles* itself, though PHC principles like participation and self-reliance help achieve it.
- (b) prioritisation and efficiency: These are good management practices, but not considered core pillars or founding principles of PHC itself.
- (c) equity and affordability: Equity is a principle/pillar component. Affordability is part of the accessibility/equity idea. This option is close, but (d) combines Appropriate Technology (a distinct pillar) and Equity (a key principle/pillar component), covering two different core areas.
20. When a nurse determines whether resources were maximised in the implementation phase, she is evaluating
- (a) effectiveness.
- (b) efficiency.
- (c) adequacy.
- (d) appropriateness.
Why other options are wrong:
- (a) effectiveness: This is about whether the program achieved its intended goals, regardless of the resources used.
- (c) adequacy: This is about whether there were *enough* resources available in the first place, not how well they were used.
- (d) appropriateness: This is about whether the interventions and methods used were suitable for the community and the problem.
Paper 1 - Fill in the Blank Spaces
21. The first step in the process of community empowerment is...?
22. A concept of PHC that involves provision of immunisation and treatment is...?
23. The first step to consider when entering the community is carrying out a...?
24. A social action process that allows people to gain mastery over their lives is known as...?
25. The study of populations is called...?
26. The process of enabling people to increase control over and to improve their health is known as health...?
27. Total elimination of a disease from the population is medically termed as...?
28. The best action to prevent spread of measles during an outbreak is...?
29. Health services whose cost can be met by most of the community members are said to be...?
30. The process that ensures maintenance of a vaccine's potency from the manufacturer to the consumer is...?
Paper 1 - Section B: Short Essay Questions
31.(a) State the five (5) stages of home visiting.
- Planning phase:📝Getting ready before you visit. This involves identifying the home, establishing friendly rapport and explaining the purpose of the visit. You observe the home and surroundings, survey the location, and gather information about the families and their health status. Analyzing this information helps identify health situations. You also prepare necessary documents and set objectives and goals for the visit.
- Entry & Establishing Rapport:Knock Knock 👋This part isn't explicitly a separate step in the provided text, but it's crucial within the "Planning phase" as you establish friendly rapport and explain the purpose of the visit upon arrival. Making them feel comfortable is key!
- Assessment & Intervention:👂觀察🩺This aligns with the "Implementation phase" where the health care provider implements the planned objectives. This includes providing health education, immunization, screening, and addressing sanitary facilities based on the assessment done during the planning phase.
- Termination/Ending the Visit:Wrap up 👋This isn't a separate step in the provided text, but it's an important part of completing the "Implementation phase" and transitioning to "Evaluation" and "Follow up." It would involve summarizing, ensuring understanding, and agreeing on next steps.
- Post-visit activities/Documentation & Evaluation/Follow up:✍️This combines the "Evaluation phase" and "Follow up." After the main activities, you assess the efficiency and acceptance of the services provided. Documentation of the visit would also fall under this, although not explicitly mentioned as a separate step. The "Follow up" involves monitoring activities to ensure expected proceedings.
31.(b) State five (5) advantages of home visiting.
- Allows assessment of the home environment:🏠🔍You can see where and how the family lives, which helps you understand factors affecting their health (like sanitation, safety, living conditions) that you wouldn't see in a clinic.
- Provides individualized and family-centred care:🧑👩👧👦❤️You can focus specifically on the family's unique needs and dynamics, tailoring your care and education to their specific situation in their own setting.
- Helps build rapport and trust:🤝Visiting people in their own home can make them feel more comfortable and respected, which helps build a strong trusting relationship between the health worker and the family.
- Facilitates reaching vulnerable populations:👵 Disabled🤱People who find it hard to come to the clinic (like the elderly, disabled, very sick, or new mothers) can be reached and cared for in their home.
- More convenient and comfortable for the family:🛋️ Time savedFamilies don't have to travel, wait in queues, or arrange childcare. It can be less disruptive to their daily life.
32. Explain the four (4) pillars of Primary Health Care.
- Equity:🌍➡️👩⚕️This pillar means that essential health services and resources should be available to everyone fairly, regardless of where they live, their social status, or how much money they have. It's about reducing inequalities in health access.
- Community Participation:🗣️🤝This pillar emphasizes that the community should not just be recipients of health services but should be actively involved in identifying their health problems, planning programs, implementing activities, and evaluating them. Their input and ownership are crucial.
- Intersectoral Coordination (or Collaboration):🏥🏫🌾💧Health is influenced by many things beyond just healthcare. This pillar means that the health sector must work together with other sectors like education, agriculture, water and sanitation, housing, etc., to address the root causes of ill health (social determinants).
- Appropriate Technology:🔧💡This pillar means using health technologies (methods, equipment, drugs) that are scientifically sound, affordable, culturally acceptable to the community, and can be maintained and used with local resources and skills. It's about choosing what is best and practical for the specific setting, not necessarily the most advanced.
Paper 1 - Section C: Long Essay Questions
33.(a) Define the term 'Primary Health Care'.
Primary Health Care (PHC) is essential health care made universally accessible to individuals and families in the community.🏠🤝It is based on practical, scientifically sound, and socially acceptable methods and technology.🧪🛠️ culturally okIt involves the full participation of the community🧑🤝🧑and is provided at a cost that the community and country can afford.💰✅PHC is the first level of contact people have with the health system, bringing health care as close as possible to where people live and work.📍🏥Its goal is to improve health outcomes by addressing the main health problems in the community and focusing on prevention, health promotion, and addressing social determinants of health, not just treating sickness.
33.(b) List ten (10) elements of primary health care.
PHC includes these key elements, often remembered by acronyms like 'ELEMENTS':
- Education:📚Health education about common health problems and how to prevent and control them.
- Locally endemic diseases:🦠Prevention and control of diseases common in the local area (like malaria, TB).
- Expanded Programme on Immunisation (EPI):💉Immunisation against major infectious diseases.
- Maternal and Child Health (MCH):🤰👶Including family planning services.
- Essential Drugs:💊Provision of essential medicines for common conditions.
- Nutrition:🍎Promotion of food supply and proper nutrition.
- Treatment:🩺🩹Appropriate treatment of common diseases and injuries.
- Safe water and sanitation:💧🚽Ensuring access to clean water and basic sanitation facilities.
- Mental Health:🧠😊Addressing mental health needs within the community.
- Dental Health:🦷Basic dental care and prevention.
33.(c) Outline five (5) roles of the community in primary health care activities.
The community is not just a receiver; they are active partners!
- Participation in Planning and Decision-Making:🗣️🗺️Community members help identify their own health needs and problems, prioritize them, and decide on the best ways to address them, alongside health workers.
- Contribution of Resources:🏗️💰Communities can contribute their own resources like labour, local materials, land, or even funds to support health activities (e.g., building a health post, digging a well, community health fund).
- Implementation of Health Activities:👷♀️👩🏫Community members can be trained as community health workers, volunteers, or health committee members to carry out various tasks like health education, basic first aid, contact tracing, or running village health teams.
- Monitoring and Evaluation:📊🔍Community members can help monitor how programs are working, provide feedback, and participate in evaluating their effectiveness and impact on the community.
- Promoting Healthy Behaviours and Practices:🍎🏃♀️🚭Community members can influence each other to adopt healthy lifestyles, practice good hygiene, use health services, and support health campaigns within their families and neighbourhoods.
34.(a) Define the term 'school health'.
School health refers to a set of planned activities and programs implemented within the school setting to protect and promote the health and well-being of students, school staff (teachers, administrators), and sometimes the wider community.🏫👩🏫🧑🎓It includes providing health services, teaching health education, and creating a safe and healthy school environment.🩺📚🌳The goal is to help students learn and grow into healthy adults by addressing their health needs while they are in school.
34.(b) State nine (9) reasons why school health programs are important.
School health programs are crucial for many reasons:
- Reach a large, accessible population:🏟️Schools gather large numbers of children and staff regularly, making it an efficient place to deliver health services and education.
- Address health issues affecting learning:🧠📖Health problems like poor vision, hearing loss, malnutrition, or infections can make it hard for children to learn. School health helps identify and address these barriers.
- Instill healthy habits early:🌱🍎Children form habits early. School health education can teach them about hygiene, healthy eating, physical activity, and preventing risky behaviours that will benefit them for life.
- Provide early detection of health problems:👀👂School health services can offer screenings for common issues (eyes, ears, growth) allowing for early detection and intervention before problems become severe.
- Offer a safe and supportive environment:🛡️😊A healthy school environment includes safe buildings, sanitation, clean water, and a supportive atmosphere free from violence or bullying, all of which affect physical and mental health.
- Promote mental and emotional well-being:😊🧘♀️Counselling and support services in schools help students deal with stress, emotional problems, and social challenges.
- Link school with family and community health:🏘️🤝🏫Schools can be a focal point for health information and activities that involve parents and the wider community, extending health promotion beyond the school gates.
- Prevent infectious disease outbreaks:🧼🚫🦠Programs can implement hygiene measures, vaccinations, and rapid response plans to control outbreaks within the school and prevent spread to the community.
- Prepare students for a healthy future:🎓➡️🌟By providing health knowledge and skills, school health programs equip students to make informed health decisions as they grow into adults.
34.(c) Outline seven (7) components of school health.
School health programs typically include several key components working together:
- School Health Education:📚🧠Teaching students knowledge and skills about health topics like hygiene, nutrition, preventing diseases (HIV/AIDS, malaria), safety, and healthy relationships.
- School Health Services:🩺🩹Providing basic health checks, first aid, managing minor illnesses, giving immunizations, health counselling, and referrals to other health facilities.
- Healthy School Environment:🌳💧🚽Ensuring safe buildings, clean water, proper sanitation (toilets), ventilation, lighting, space for physical activity, and a social climate that is supportive and free from harm.
- School Nutrition Services:🍎🥪Promoting healthy eating, providing school meals or snacks, and educating students about good nutrition.
- School Physical Education and Activity:🏃♀️⚽Providing opportunities for regular physical activity and teaching skills for various sports and exercises.
- School Counseling, Psychological, and Social Services:😊🗣️🤝Offering support for students' mental and emotional health, addressing social issues, and providing counselling services.
- School-Community Health Promotion:🏫🤝🏘️Activities that involve parents, families, and the wider community in supporting school health initiatives and extending health messages beyond the school.
Paper 2 - Section A: Objective Questions (MCQs)
1. The approach of diagnosing and treating a disease in its earliest stage is called ______ prevention.
- (a) Primary.
- (b) Secondary.
- (c) Tertiary.
- (d) Health.
Why other options are wrong:
- (a) Primary: Prevents the disease from starting at all (e.g., vaccination).
- (c) Tertiary: Manages an existing disease to prevent disability or complications (e.g., rehabilitation).
- (d) Health: This is the state of well-being, not a type of prevention.
2. Which of the following is the most appropriate approach to community entry?
- (a) Radio announcement.
- (b) Community survey.
- (c) Community leaders.
- (d) Church leaders.
Why other options are less appropriate as the *first* step:
- (a) Radio announcement: Good for informing later, but not the initial way to build relationships and get approval.
- (b) Community survey: This is a method for assessment *after* you've gained entry and permission.
- (d) Church leaders: Important in many communities, but focusing only on one type of leader might exclude others or sections of the community. Meeting broader community leaders is usually better initially.
3. Which of the following is NOT related to the importance of school health programme?
- (a) Promote provision of medical and dental care.
- (b) Promote better nutrition and feeding practices.
- (c) Provide counselling services to adolescents.
- (d) Tap talents of both male and female students.
Why other options ARE related to school health importance:
- (a) Promote provision of medical and dental care: Access to basic care in school is a clear health benefit.
- (b) Promote better nutrition and feeding practices: Good nutrition is fundamental to child health and development, a key area for school health.
- (c) Provide counselling services to adolescents: Adolescence is a time of unique health challenges, and counselling is a vital support service.
4. Environmental disease control measures include the following EXCEPT;
- (a) better housing and living conditions.
- (b) provision of safe water supply.
- (c) good life styles and healthy habits.
- (d) proper disposal of refuse.
Why other options ARE environmental control measures:
- (a) better housing and living conditions: Reduces overcrowding and exposure to poor sanitation.
- (b) provision of safe water supply: Prevents waterborne diseases.
- (d) proper disposal of refuse: Reduces breeding grounds for pests and prevents spread of pathogens.
5. The disease that is present the whole time in the community and occurs all year round is referred to as
- (a) holoepidermic.
- (b) holo endemic.
- (c) hyper epidemic.
- (d) hypo endemic.
Why other options are wrong:
- (a) holoepidermic: Not a standard epidemiological term.
- (c) hyper epidemic: Hyperendemic describes a persistent *high* level, but "epidemic" itself means an *increase* beyond the usual level.
- (d) hypo endemic: Describes a disease that is endemic but at a *low* level.
6. The type of survey that involves questioning and examining a sample of the population at one point at a period of time is termed as
- (a) longitudinal survey.
- (b) cross sectional survey.
- (c) horizontal survey.
- (d) screening.
Why other options are wrong:
- (a) longitudinal survey: Follows the same group of people over a period of time, taking measurements at different points.
- (c) horizontal survey: Not a standard epidemiological term.
- (d) screening: This is a quick test to *identify* potential cases of a disease, not a full survey method.
7. Which of the following is a method of community mobilization?
- (a) Political commitment.
- (b) Good leadership.
- (c) Home visiting.
- (d) Guidance and counseling.
Why other options are less direct methods of mobilization:
- (a) Political commitment: This is an enabling factor that can support community mobilization efforts, but it's not a method of engaging the community directly.
- (b) Good leadership: While essential for guiding and facilitating mobilization, leadership itself is a quality or role, not a specific *method* of reaching and engaging the community.
- (d) Guidance and counseling: These are individual-level support services and are not typically used as primary methods for mobilizing a whole community.
8. The best course of action to take when there is an outbreak of measles in the community is to
- (a) instruct mothers to feed their community adequately.
- (b) instruct mothers to keep their babies home.
- (c) give to babies aged 6-11 months vitamin A.
- (d) immunize babies aged 6-9 month with measles vaccine.
Why other options are less effective for outbreak control:
- (a) instruct mothers to feed adequately: Good nutrition is important for recovery but doesn't stop transmission.
- (b) instruct mothers to keep their babies home: Isolation helps, but vaccination is more proactive and provides lasting protection.
- (c) give to babies aged 6-11 months vitamin A: Vitamin A helps reduce the severity of measles, but it doesn't prevent infection or transmission. Vaccination is the primary preventive measure.
9. Which of the following is true with regards to guinea worm infection?
- (a) Cyclops are the intermediate hosts.
- (b) Larvae enter the body through intact skin.
- (c) Female worm may be seen in subcutaneous tissues.
- (d) To prevent infestation, step well should be used in bathing.
Why other options are false:
- (b) Larvae enter the body through intact skin: Infection happens by *drinking* contaminated water, not through the skin.
- (c) Female worm may be seen in subcutaneous tissues: The adult female worm migrates through the body and eventually emerges *from* the skin, usually on the leg, often causing a painful blister. You see her emerging, not just passively "seen" under the skin before she comes out.
- (d) To prevent infestation, step well should be used in bathing: This is wrong. Step wells are easily contaminated. Using *protected* water sources or filtering water is how you prevent infection. Bathing in infected water sources (like step wells) can spread the disease if an infected person enters the water while their worm is emerging.
10. Hyper pigmentation in onchocererciasis results in
- (a) module formation.
- (b) blindness.
- (c) lizard skin.
- (d) calabar swelling.
Why other options are wrong:
- (a) module formation: Onchocerciasis causes subcutaneous nodules (lumps) where adult worms live, but hyperpigmentation is a skin symptom, not the nodules themselves.
- (b) blindness: Blindness is a severe complication affecting the eyes, not a skin pigmentation issue.
- (d) calabar swelling: These are large, temporary swellings associated with Loiasis ("African eye worm"), a different parasitic infection.
11. The single and most important measure in the control of Tuberculosis in the community is
- (a) health education.
- (b) BCG immunization.
- (c) contact tracing.
- (d) treatment compliance.
Why other options are important but not the *single most* important:
- (a) health education: Helps people understand TB and seek care, but doesn't stop spread from already infected, untreated individuals.
- (b) BCG immunization: Protects young children from severe forms but is less effective against pulmonary (lung) TB in adults, which is the main source of spread.
- (c) contact tracing: Helps find people who might be infected, but they also need treatment/prevention (which relies on *treatment compliance* of the original case).
12. Which of the following gastro-intestinal complication may occur in a child with severe paroxysms of whooping cough?
- (a) Gastric ulcer.
- (b) Umblical hernia.
- (c) Ulcerative colitis.
- (d) Pylorospasm.
Why other options are unrelated:
- (a) Gastric ulcer: Sores in the stomach lining, not caused by coughing pressure.
- (c) Ulcerative colitis: Inflammation and ulcers in the large intestine, an inflammatory bowel disease.
- (d) Pylorospasm: Spasm of the muscle controlling the exit from the stomach, typically seen in infants causing vomiting, not directly related to whooping cough pressure.
13. Resistance of susceptible individual to certain bacterial or viral infections can be artificially enhanced by
- (a) medical treatment.
- (b) health education.
- (c) immunization.
- (d) good nutrition.
Why other options are wrong:
- (a) medical treatment: Treats an infection *after* it happens, doesn't prevent it by enhancing resistance beforehand.
- (b) health education: Provides information about preventing infection through behavior, but doesn't directly enhance the body's internal resistance.
- (d) good nutrition: Supports overall immune function, contributing to general resistance, but immunization provides specific, targeted artificial resistance.
14. An acute bacterial infection characterized by step ladder fever spread through contamination of food and water is
- (a) Typhoid.
- (b) Malaria.
- (c) Measles.
- (d) Dysentery.
Why other options are wrong:
- (b) Malaria: Caused by a parasite, spread by mosquitoes, and has cyclical fever, not step-ladder.
- (c) Measles: Caused by a virus, spread by air, causes rash, and has a different fever pattern.
- (d) Dysentery: Bacterial or amoebic, spreads via food/water (fecal-oral), causes severe diarrhea with blood, but step-ladder fever is not a key characteristic.
15. Organisms that usually benefit the person infested are called
- (a) pathogens.
- (b) commensals.
- (c) symbiotics.
- (d) parasites.
Why other options are wrong:
- (a) pathogens: Cause harm to the host.
- (b) commensals: Benefit themselves without significantly helping *or* harming the host.
- (d) parasites: Benefit themselves *at the expense of* the host (cause harm).
16. The primary health care pillar which helps in policy formation, resource allocation, community mobilization and support is called
- (a) community participation.
- (b) appropriate technology.
- (c) political commitment/will.
- (d) intersectoral collaboration.
Why other options are related but not the driving force for these activities:
- (a) community participation: The community's role in the program, enabled by support and policy.
- (b) appropriate technology: The suitable tools used in PHC.
- (d) intersectoral collaboration: Different sectors working together, which is facilitated by policy and political support.
17. The sustainable development goal builds on a principle called
- (a) health for all.
- (b) gender inequality.
- (c) holistic approach.
- (d) leaving no one behind.
Why other options are wrong:
- (a) health for all: A key principle of PHC and a goal addressed by SDG 3, but "leaving no one behind" is a broader principle guiding *all* SDGs.
- (b) gender inequality: This is a problem the SDGs aim to *solve* (SDG 5), not a principle they are built upon.
- (c) holistic approach: The SDGs do take a holistic view (seeing how everything is connected), but "leaving no one behind" is a more specific, named principle guiding their implementation.
18. The following are sustainable development goals EXCEPT;
- (a) affordable and clean energy.
- (b) climatic action.
- (c) to stop accidents.
- (d) industry innovation and infrastructure.
Why other options ARE SDGs:
- (a) affordable and clean energy (SDG 7).
- (b) climatic action (SDG 13).
- (d) industry innovation and infrastructure (SDG 9).
19. Which of the following explains the meaning of appropriate technology?
- (a) Drawing up of joint plans.
- (b) improving local capacity.
- (c) Improving development projects.
- (d) Improving community mobilization.
Why other options are outcomes or other activities:
- (a) Drawing up of joint plans: This is part of planning, not the meaning of appropriate technology itself.
- (c) Improving development projects: Appropriate technology helps make projects better, but it's a means to an end, not the definition of the technology concept.
- (d) Improving community mobilization: Appropriate technology can support mobilization (e.g., simple communication tools), but that's not what the concept of appropriate technology primarily means.
20. Which of the following is NOT a condition for effectiveness of the community health Services?
- (a) Availability.
- (b) Accessibility.
- (c) Equity.
- (d) Utilization.
Paper 2 - Fill in the Blank Spaces
21. Contact tracing of a person who has been exposed to a communicable epidemic disease helps the health worker to carry out...?
22. The component of community health that promotes the well being of the child and her education is called...?
23. The causative micro organism of jiggers infection is...?
24. Severe form of malaria caused by plasmodium falciparum is called...?
25. The characteristic sign that appears during the prodromal stage of measles is called...?
26. The period of isolation of an infectious or suspect case to prevent the spread of the disease is called...?
27. The recommended dose of BCG given to a child below 12 months is...?
28. Evaluation of immunization campaign is by carrying out...?
29. Health services whose cost can be met by most of the community members are said to be...?
30. The process that ensures maintenance of a vaccine's potency from the manufacturer to the consumer is...?
Paper 2 - Section B: Short Essay Questions
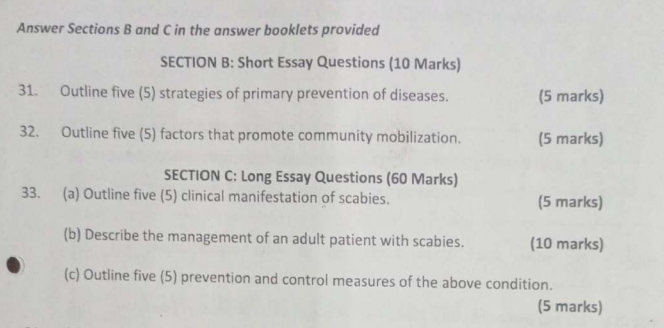
31. Outline five (5) strategies of primary prevention of diseases.
Primary prevention aims to stop diseases from starting in the first place, for healthy people.
- Health Education and Promotion:📚🍎🏃♀️Teaching people about healthy lifestyles, good hygiene, balanced diet, and the importance of physical activity to prevent various diseases.
- Immunization/Vaccination:💉🛡️Giving vaccines to protect individuals from specific infectious diseases (like measles, polio, tetanus) before they are exposed.
- Improving Environmental Sanitation:💧🚽🌳Ensuring access to clean and safe drinking water, proper disposal of waste (faeces, refuse), and vector control (like mosquito nets) to prevent infectious diseases.
- Specific Protection Measures:🧤🧢Using methods that directly protect against harm, such as using condoms to prevent STIs, wearing helmets when cycling, or using seatbelts in cars.
- Nutritional Programs:🥕🍚Promoting adequate and balanced nutrition, providing supplements (like Vitamin A or iron) to prevent deficiency diseases, especially in vulnerable groups like children and pregnant women.
32. Outline five (5) factors that promote community mobilization.
These factors help get a community motivated and organized for action:
- Strong Local Leadership:🗣️👍Having respected and dynamic leaders within the community who can inspire, guide, and organize people.
- Clear Identification of a Felt Need/Problem:💡🔥When community members clearly see and agree on a problem that affects them, they are more likely to be motivated to act to solve it.
- Trust and Good Relationship:🤝😊Building trust between the community members themselves and between the community and external health workers encourages open communication and willingness to work together.
- Perceived Benefit/Incentive:🎁🌟When community members believe that participating will bring clear benefits to them or their families, or if there's some form of motivation, they are more likely to get involved.
- Effective Communication:📣👂Using clear, simple, and culturally appropriate language and methods to share information, discuss issues, and plan activities ensures everyone understands and feels included.
Paper 2 - Section C: Long Essay Questions
33.(a) Outline five (5) clinical manifestation of scabies.
Scabies is a skin condition caused by tiny mites burrowing into the skin. Here are common signs you would see or hear about:
- Intense Itching (Pruritus):😩 itchy!This is the most common symptom, often severe and typically worse at night, which can disturb sleep.
- Rash:🔴bumpsSmall red bumps (papules) or tiny blisters can appear on the skin, often in a widespread pattern or clustered in certain areas.
- Burrows:〰️Tiny, slightly raised lines that look like tracks or tunnels on the skin surface. These are where the mites burrow. They are often found in the thin skin between fingers, on wrists, elbows, or feet.
- Sores or Crusting (especially in severe cases):🩹Scratching the itchy rash can lead to open sores, which can then get infected with bacteria. Crusted scabies is a very severe form with thick crusts containing many mites.
- Distribution Pattern:✋ Wrist🦶The rash and burrows often appear in specific body areas where the mites like to live, such as the webs of fingers and toes, wrists, elbows, armpits, waistline, buttocks, and genitals. In infants, the head, neck, palms, and soles can also be affected.
33.(b) Describe the management of an adult patient with scabies.
Managing scabies requires treating not only the patient but also their close contacts and cleaning the environment to prevent reinfection.
Aims of Management of Scabies- Diagnosis Confirmation:🔍🩺A doctor or nurse examines the skin for the characteristic rash and burrows. Sometimes, a skin scraping is done to look for mites, eggs, or faeces under a microscope.
- Application of Scabicide:🧴The most common treatment is a lotion or cream (like Permethrin 5%). The patient is instructed to apply it to their *entire body* from the neck downwards, making sure to cover all skin folds, between fingers and toes, and under nails.
- Treatment Duration:⏱️⏰The scabicide is usually left on the skin for a specific time (e.g., 8-14 hours, often overnight) before being washed off. A second application might be recommended a week later to kill mites that hatch from eggs missed in the first treatment.
- Treatment of Contacts:🧑🤝🧑 SimultaenousIt is VITAL that all people who had close, prolonged skin-to-skin contact with the infected person (like family members, sexual partners, or housemates) are treated at the *same time*, even if they don't show symptoms yet. This breaks the cycle of transmission.
- Hygiene Measures (Clothing and Bedding):🧺🔥All clothing, bedding, and towels used by the infected person and contacts in the 72 hours before treatment should be washed in hot water (at least 50°C or 122°F) and machine dried on a hot cycle, or dry-cleaned. Items that cannot be washed should be sealed in a plastic bag for at least 72 hours to a week to kill the mites.
- Management of Symptoms:soothe 🌬️Itching can continue for a few weeks even after the mites are dead. Antihistamines can be prescribed to help with the itching, and sometimes topical steroid creams for the rash (but not used if scabicide is on).
- Follow-up:🔄✅A follow-up appointment might be needed to check if the treatment worked and to manage any persistent symptoms or secondary infections.
Management include;
33.(c) Outline five (5) prevention and control measures of the above condition (Scabies).
To prevent and control scabies:
- Early Diagnosis and Prompt Treatment:⏰💡Quickly identifying people with scabies and treating them as soon as possible stops them from spreading the mites.
- Simultaneous Treatment of Contacts:🏠👨👩👧👦Making sure everyone who lived with or had close contact with the infected person gets treated at the same time is essential to prevent reinfection and continued spread.
- Proper Hygiene and Environmental Cleaning:🧼🧺Washing clothes, bedding, and towels in hot water and drying them thoroughly helps kill mites that have fallen off the skin.
- Avoid Close Skin-to-Skin Contact:🙅♀️🤝Avoiding prolonged direct physical contact with someone known to have scabies can prevent transmission.
- Health Education:📚🗣️Educating individuals and communities about how scabies spreads, its symptoms, and the importance of treating everyone in the household at once, and hygiene measures.
34.(a) Outline ten (10) sustainable development goals, excluding good health and well being.
The Sustainable Development Goals (SDGs) are a set of 17 global goals adopted by the United Nations. Here are all seventeen, with ten outlined as requested (excluding SDG 3 Good Health and Well-being):
- SDG 1: No Poverty➡️💵🚫Ending poverty in all its forms everywhere.
- SDG 2: Zero Hunger🍎🥖Ending hunger, achieving food security and improved nutrition, and promoting sustainable agriculture.
- **SDG 3: Good Health and Well-being**❤️🩹💪Ensuring healthy lives and promoting well-being for all at all ages.
- SDG 4: Quality Education📚👩🎓Ensuring inclusive and equitable quality education and promoting lifelong learning opportunities for all.
- SDG 5: Gender Equality👩=👨Achieving gender equality and empowering all women and girls.
- SDG 6: Clean Water and Sanitation💧🚽Ensuring availability and sustainable management of water and sanitation for all.
- SDG 7: Affordable and Clean Energy💡☀️Ensuring access to affordable, reliable, sustainable, and modern energy for all.
- SDG 8: Decent Work and Economic Growth💼📈Promoting sustained, inclusive, and sustainable economic growth, full and productive employment, and decent work for all.
- SDG 9: Industry, Innovation, and Infrastructure🏗️🏭💡Building resilient infrastructure, promoting inclusive and sustainable industrialization, and fostering innovation.
- SDG 10: Reduced Inequalities📉⚖️Reducing inequality within and among countries.
- SDG 11: Sustainable Cities and Communities🏙️🏘️Making cities and human settlements inclusive, safe, resilient, and sustainable.
- SDG 12: Responsible Consumption and Production♻️🛍️Ensuring sustainable consumption and production patterns.
- SDG 13: Climate Action🌍🔥❄️Taking urgent action to combat climate change and its impacts.
- SDG 14: Life Below Water🐠🌊Conserving and sustainably using the oceans, seas, and marine resources for sustainable development.
- SDG 15: Life on Land🌳🦁Protecting, restoring, and promoting sustainable use of terrestrial ecosystems, sustainably managing forests, combating desertification, and halting and reversing land degradation and halting biodiversity loss.
- SDG 16: Peace, Justice, and Strong Institutions🕊️⚖️🏛️Promoting peaceful and inclusive societies for sustainable development, providing access to justice for all, and building effective, accountable, and inclusive institutions at all levels.
- SDG 17: Partnerships for the Goals🤝🌍Strengthening the means of implementation and revitalizing the global partnership for sustainable development.
34.(b) Explain five (5) targets of the third sustainable development goal. (ensure good health and well being)
SDG 3 is "Ensure healthy lives and promote well-being for all at all ages". It has many targets to achieve this goal. Here are five examples:
- Reduce Maternal Mortality:🤰📉A target is to reduce the global maternal mortality ratio (deaths of mothers during pregnancy or childbirth) to less than 70 per 100,000 live births. This means making pregnancy and delivery safer.
- End Preventable Child Deaths:👶➡️grow upA target is to end preventable deaths of newborns and children under 5 years old, aiming to reduce neonatal mortality (deaths in the first month) to at least as low as 12 per 1,000 live births and under-5 mortality to at least as low as 25 per 1,000 live births.
- Fight Communicable Diseases:🚫🦠 ाA target is to end the epidemics of diseases like AIDS, Tuberculosis, Malaria, and neglected tropical diseases, and combat Hepatitis, water-borne diseases, and other major infectious diseases.
- Reduce Non-Communicable Diseases (NCDs):❤️🧠📉A target is to reduce premature deaths from NCDs (like heart disease, cancer, diabetes, lung diseases) by one-third through prevention and treatment, and promote mental health and well-being.
- Achieve Universal Health Coverage (UHC):🏥ForAllA target is to achieve UHC, meaning everyone has access to the health services they need, when and where they need them, without facing financial hardship. This includes access to essential medicines and vaccines.
35.(a) Outline five (5) measures that are used to protect a susceptible host from an infectious disease in the community.
These measures focus on strengthening or protecting the person (the susceptible host) so they don't get sick, even if they are exposed to the disease agent:
- Immunization:💉🛡️Giving vaccines to a healthy person to make their immune system strong against a specific infection, so they don't get the disease or get a milder form if exposed.
- Chemoprophylaxis:💊🛡️Giving medication to a healthy person to prevent them from getting infected, even if exposed (e.g., taking antimalarial drugs when traveling to a malaria area, or medication to prevent TB in contacts).
- Health Education and Behaviour Change:📚🧼🚶♀️Teaching people about how diseases spread and promoting healthy behaviours like handwashing, safe food handling, safe sex, avoiding crowded places during outbreaks, or using bed nets. This empowers the host to reduce their own risk.
- Improved Nutritional Status:🍎💪Ensuring people have good nutrition strengthens their overall immune system, making them less susceptible to infections and better able to fight them off if they do get infected.
- Use of Personal Protective Measures:😷🚫🐜Advising individuals to use personal protective equipment like wearing masks (for airborne diseases), using treated bed nets (for malaria), or filtering/treating drinking water at home (for waterborne diseases).
35.(b) Explain five (5) techniques applied in home visiting.
When a health worker visits a home, they use different techniques to interact effectively with the family:
- Establishing Rapport and Trust:🤝😊From the moment you arrive, focus on making the family feel comfortable and respected. Be polite, listen actively, show empathy, and build a trusting relationship. This opens the door for effective communication and assessment.
- Active Listening:👂🤔Pay full attention to what family members are saying, both verbally and non-verbally. Ask clarifying questions, summarize what you've heard to show you understand, and don't interrupt. This helps uncover their real concerns and needs.
- Using Open-ended Questions:❓🗣️Ask questions that require more than just a 'yes' or 'no' answer (e.g., "Tell me about..." or "How have you been managing...?"). This encourages family members to share more information and express their feelings.
- Observation:👀🔍While interacting, observe the home environment (cleanliness, safety, resources), the family dynamics (how members interact), the health status of individuals, and their interactions with each other. Observation provides valuable non-verbal information.
- Demonstration and Return Demonstration:👩🏫➡️🧑💻When teaching skills (e.g., how to prepare ORS, how to care for a wound, how to breastfeed), first show the family how to do it (demonstration). Then, ask them to do it themselves while you watch and guide (return demonstration) to make sure they learned correctly.
- Collaborative Problem-Solving:🗺️👥💡Work *with* the family to identify solutions to their health problems, rather than just telling them what to do. Discuss options, consider their resources and preferences, and help them choose solutions that work best for them.

it was so amazing
It so awesome