Table of Contents
ToggleCHICKEN POX (Varicella-Zoster Virus)
Chickenpox (varicella) is a highly contagious viral infection caused by the varicella-zoster virus (VZV), a member of the Herpesviridae family.
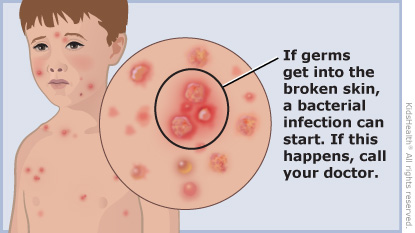
It’s characterized by a pruritic (itchy) rash that progresses through macules (flat spots), papules (raised bumps), vesicles (fluid-filled blisters), pustules (pus-filled blisters), and finally crusts.
The colloquial name “Don’t Touch Me” reflects its contagious nature. The name “chicken pox” likely originates from the French “chich,” meaning chickpea, referring to the appearance of the vesicles.
Aetiology: VZV is a double-stranded DNA virus with an envelope. It’s transmitted via airborne droplets and direct contact with vesicle fluid.
Risk Groups:
- Children under 10 years old (most commonly affected)
- Immunocompromised individuals (those with weakened immune systems due to HIV, cancer, organ transplantation, etc.)
- Pregnant women (risk of congenital varicella syndrome)
- Adults who have not had chickenpox or the vaccine (risk of more severe illness)
Mode of Transmission:
- Airborne: Inhalation of respiratory droplets from an infected person.
- Direct contact: Touching the fluid from ruptured vesicles.
- Indirect contact: Touching contaminated surfaces (fomites) then touching the eyes, nose, or mouth.
Epidemiology/Occurrence:
Chickenpox is globally prevalent, with most cases occurring in children. Mortality is very low, but scarring can occur, and these scars are susceptible to secondary bacterial infections. The infection typically confers lifelong immunity. However, the virus can remain latent in the nervous system and reactivate later in life, causing shingles (herpes zoster). This is especially likely in immunocompromised individuals or those with conditions like diabetes mellitus or leukemia.
Incubation Period: 10-21 days, averaging 14-16 days.
Pathogenesis:
The virus enters the body through the upper respiratory tract mucosa. Primary viremia (virus in the bloodstream) occurs, followed by secondary viremia, which disseminates the virus throughout the body. The virus then infects skin cells, causing the characteristic rash. The subcutaneous tissues and skin are primarily affected, with vesicle formation, rupture, and subsequent scarring during healing.
Signs and Symptoms:
- Prodromal phase (1-2 days): Mild fever, headache, malaise, anorexia, body aches.
- Maculopapular rash: Progresses to vesicles, pustules, and crusts. The rash is widespread, typically beginning on the face, scalp, and trunk, then spreading to the extremities. Different stages of lesions (macules, papules, vesicles, pustules, crusts) are often present concurrently.
- Intense itching: A hallmark symptom.
- Fever: Usually mild to moderate.
- Lymphadenopathy: Swollen lymph nodes. (This is not explicitly mentioned in the provided text but is common).
Differential Diagnosis:
- Impetigo
- Multiple insect bites
Diagnosis
Diagnosis is primarily clinical, based on the characteristic rash and symptoms. Laboratory confirmation (viral culture, PCR, serology) might be done in ambiguous cases or for severe infections.
Management:
Aims:
- Prevent spread of infection.
- Prevent secondary bacterial infections.
- Relieve symptoms (itching, pain, fever).
- Prevent complications.
Actual Management:
- Isolation: Strict isolation precautions are crucial to prevent spread until all lesions are crusted over (typically 5-7 days after rash onset). This includes contact precautions, airborne precautions (depending on local guidelines), and proper disposal of contaminated materials.
- Skin care: Frequent bathing with lukewarm water, gentle patting dry, and application of calamine lotion or oatmeal baths to relieve itching. Keeping fingernails short is vital.
- Medications:
- Antivirals: Acyclovir, valacyclovir, or famciclovir are recommended for high-risk individuals (adults, immunocompromised individuals, pregnant women) if started early in the course of the illness.
- Analgesics/Antipyretics: Acetaminophen (paracetamol) for fever and pain relief. NSAIDs (like ibuprofen) can be considered, but aspirin should be avoided due to the risk of Reye’s syndrome.
- Antihistamines: To help control itching.
- Topical corticosteroids: Might be used in severe cases to reduce inflammation, but this should be at the discretion of a doctor.
- Antibiotics: Only necessary if secondary bacterial infections develop.
- Diet: Nutritious, well-balanced diet to support healing and recovery.
- Supportive care: Ensuring adequate fluid intake, rest, and emotional support.
Symptomatic and Supportive Treatment:
- Skin Care: Frequent bathing with lukewarm water, gentle patting dry, and application of calamine lotion every 12 hours or as needed. Cool, wet compresses can also provide relief from itching.
- Antihistamines: To alleviate itching.
- Chlorpheniramine: Adults: 4 mg every 12 hours. Children under 5 years: 1-2 mg every 12 hours for a maximum of 3 days. (Always follow age-appropriate dosing guidelines; this information should be considered a general guideline only).
- Analgesics/Antipyretics: Acetaminophen (paracetamol) for fever and pain relief. The dose is generally 10 mg/kg every 6 hours, but precise dosing should always be determined by a healthcare professional based on the child’s weight and age.
- Antivirals: For adults and children over 12 years old, oral aciclovir 800 mg every 6 hours for 7 days may be considered, especially for severe cases or high-risk individuals. This decision should be made by a doctor, and early initiation is crucial for effectiveness.
- Isolation: Keep the child home/away from school until all lesions are crusted over to prevent the spread of infection.
Complications:
- Bacterial skin infections (impetigo, cellulitis): Most common complication resulting from scratching.
- Pneumonia: VZV can directly infect the lungs.
- Encephalitis: Rare but serious inflammation of the brain.
- Hepatitis: Inflammation of the liver.
- Myocarditis: Inflammation of the heart muscle.
- Nephritis: Kidney inflammation (often due to secondary bacterial infection).
- Congenital varicella syndrome: If a pregnant woman contracts chickenpox, particularly during the first 20 weeks of pregnancy, the fetus can suffer severe abnormalities.
- Hemorrhagic chickenpox: Rare and severe, with bleeding into the skin.