Table of Contents
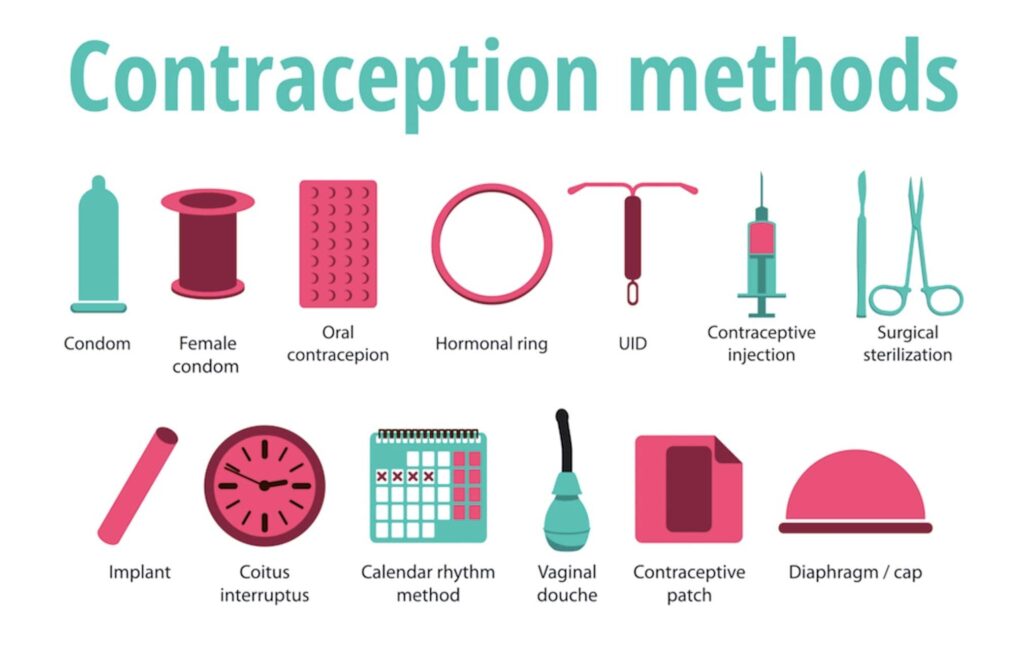
ToggleArtificial Methods of Family Planning
Artificial methods of family planning refer to the use of various techniques and devices to prevent pregnancy. These methods rely on the use of physical barriers, chemicals, or surgical interventions to either prevent sperm from reaching the egg or to interfere with the fertilization process.
FAMILY PLANNING CARD
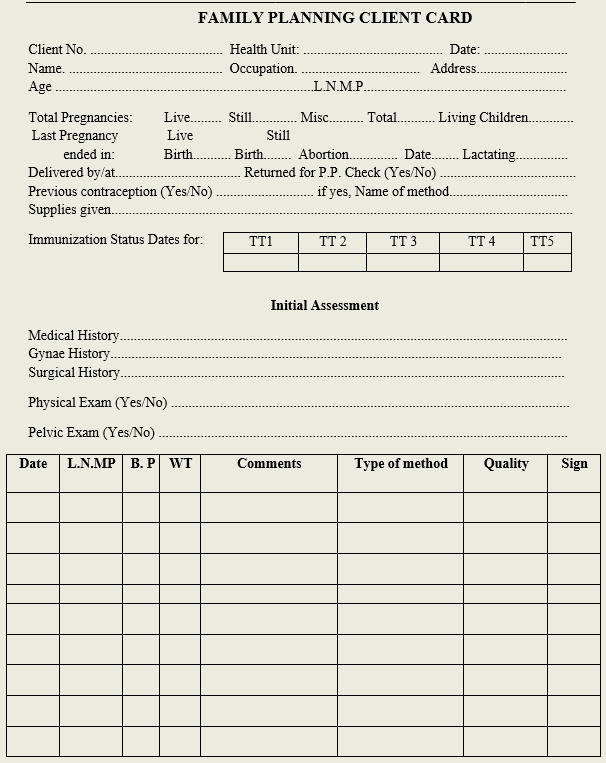
Criteria to follow before a client is put on a family planning methods
History taking
- Personal Age, sex, address, next of kin
- Social Marital status, education, any habits that may affect choices of some family planning methods e.g. smoking
- Medical To identify the presence of medical diseases, problems, sickle cell, medications.
- Reproductive /obstetric history:
- Find out when clients started her period
- How many children/pregnancies she had
- Gynecological To identify any diseases affecting a woman‘s reproductive organs e.g. bleeding, cancer of the cervix, PIDs, breast cancer etc.
- Family planning To find out about previous use of family planning methods.
General examination
Should be done from the head to toes;
- Anemia, edema, jaundice, lymphadenopathy
- Breast for colour changes, masses
- Per abdominal examination to check for masses
- Per vaginal examination to check for abnormal discharges
Note: Weight, blood pressure should be recorded when starting one on family planning especially the hormonal ones.
Artificial methods of family planning
Barrier methods
- Spermicides
- Condoms
- IUCDs
- Diaphragm
- Intra-vaginal contraceptive sponge
- Cervical caps
Condoms (male and female)
- This is the most popular and oldest method
- This is a rubber sheath that is worn by a woman or man during sexual intercourse
- It is the only family planning method that prevents both pregnancy and STIs including HIV/AIDs if used consistently and correctly.
Indications
Condoms can be used by any man or woman regardless of his/her health status. People in particular need of condoms include:
- Men wishing to participate more actively in family planning
- Sexually active adolescents
- Couples who have sexual intercourse infrequently
- People in casual sexual relationships where pregnancy is not desired
- Couples needing a back-up method while waiting for another contraceptive methods to become effective.
- Couples who need a temporary method while waiting to receive another contraceptive method.
- Those who are at increased risk of STIs, (e.g. when one or both partners have other partners)
- Couples where one or both partners are HIV positive

Male Condoms
Male condoms are sheaths or coverings that fit over a man‘s erect penis. Most are made from thin latex rubber; some are polyurethane (plastic).
Primary mechanism of action
- Work by forming a barrier that keeps sperm out of the vagina, preventing pregnancy
- Also keep infectious agents in semen, on the penis, or in the vagina from infecting the other partner
Effectiveness
- Protection against pregnancy:
- As commonly used, about 18pregnancies per 100 women whose partners use male condoms over the first year
- When used correctly with every act of sex, about 2 pregnancies per 100 women whose partners use male condoms over the first year
Protection against HIV and other STIs:
- Male condoms significantly reduce the risk of becoming infected with HIV when used correctly with every act of sex.
- When used consistently and correctly, condom use prevents 80% to 95% of HIV transmission that would have occurred without condoms.
- Condoms reduce the risk of becoming infected,
- Protect best against STIs spread by discharge, such as HIV, gonorrhea, and Chlamydia
- Also protect against STIs spread by skin to skin contact, such as herpes and human papilloma virus (if condom covers lesions)
Any client concerns or questions
- Reinforcing correct condom use and reminding clients that condoms should not be reused
- Allergy to latex
Dispelling myths regarding condoms
Male condoms:
- Do not make men sterile, impotent, or weak
- Do not decrease men’s sex drive
- Do not promote promiscuity
- Cannot get lost in the woman’s body
- Do not have holes that HIV can pass through
- Are not laced with HIV
- Do not cause illness in a woman because they prevent semen or sperm from entering her body
- Do not cause illness in men because sperm may move back up
- Are used by married couples; they are not only for use outside marriage
Who should not use condoms?
Individuals allergic to latex should consider other contraceptive options. However, for those at risks of STIs/HIV, condom use is still appropriate as there are no other methods that offer STI/HIV protection.
How to use male condoms
- Use a new condom for each act of sex. Check package for damage and check the expiration Tear open carefully without using any sharp objects.
- Before any physical contact, put condom on the tip of the erect penis with the rolled side out.
- Unroll condom all the way to the base of the erect penis.
- Immediately after ejaculation, hold rim in place and withdraw penis while it is still Slide the condom off, avoiding spilling semen.
- Dispose of the used condom safely.
Practices to avoid when using condoms
- Unrolling condom before putting it on
- Using oil-based lubricants with latex condoms
- Using condoms that may be old or damaged (e.g. dried out, brittle, sticky)
- Reusing condoms
Practicing dry sex as it increases possibility of condom breakages due to friction

Female Condoms
- Female condoms are sheaths, or linings, that fit loosely inside a woman‘s vagina
- Most common type is Female Condom Two (FC2) made of thin, soft, synthetic rubber film, with flexible rings at both ends
- Latex female condoms are available in some countries Primary mechanism of action
- Work by forming a barrier that keeps sperm out of the vagina, preventing pregnancy
- Also keep infectious agents in semen, on the penis, or in the vagina from infecting the other partner
Effectiveness
Protection against pregnancy:
- When used correctly with every act of sex, about 5 pregnancies per 100 women using female condoms over the first year
- As commonly used, about 21 pregnancies per 100 women using female condoms over the first year.
- Protection against HIV and other sexually transmitted infections (STIs):
- Female condoms reduce the risk of infection with STIs, including HIV, when used correctly with every act of sex.
Characteristics of female condoms
- Safe
- Women can initiate their use
- Have a soft texture that quickly conducts body heat during sex
- Provide dual protection (against STIs/HIV and pregnancy)
- Outer ring provides added sexual stimulation for some women
- Do not require provider‘s help
- Can be inserted ahead of time so do not interrupt sex
- Are not tight or constricting like male condoms
- Do not dull the sensation of sex like male condoms
- Do not have to be removed immediately after ejaculation
- No side effects
- Can be used as a temporary backup method of contraception
- Protect women from conditions caused by STIs (pelvic inflammatory disease, cervical cancer, infertility)
- As typically used, less effective than many other FP methods
- Require partner communication and cooperation
- May be difficult to insert
- Can make noise during sex
Side effects of female condoms:
- None
- Allergic reactions to latex
Who can use female condom?
- All men and women can safely use synthetic rubber female
- All men and women can safely use natural latex female condoms, except those with a severe allergy to latex (extremely rare).
How to use female condoms
- Use a new condom for each act of sex.
- Check the condom
- Do not use if torn, damaged or past the expiration
- Open the package
- Before any physical contact, insert the condom into the vagina. It can be inserted up to eight hours before sex. Find a comfortable position for insertion—squat; raise one leg, sit, or lie down. Grasp the ring at the closed end, and squeeze it so it becomes long and With the other hand, separate the outer lips and locate the opening of the vagina. Gently insert the inner ring into the vagina as far up as it will go. Insert a finger into the condom to push it into place. (The inner ring should be pushed up just past the pubic bone.)
- Ensure that the penis enters the condom and stays inside the
- To remove the condom, hold and twist outer ring to seal in fluids, and gently pull condom out of the vagina. The female condom does not need to be removed immediately after sex, but any time before standing up, to avoid spilling semen.
- Dispose of the used condom safely.
Tips for new users
- Suggest to a new user that she practice putting in and taking out the condom before the next time she has sex. Reassure her that correct use becomes easier with practice. A woman may need to use the female condom several times before she is comfortable with it.
- Suggest she try different positions to see which way insertion is easiest for her.
- The female condom is Some women find insertion easier if they put it in slowly, especially the first few times.
- If a client is switching from another method to the female condom, suggest that she continue with the previous method until she can use the female condom with confidence.
Provide follow up and counseling for
- Any client concerns or questions
- Correct condom use
Dispelling myths regarding female condoms
Female condoms:
- Cannot get lost in the woman‘s body
- Are not difficult to use, but correct use needs to be learned
- Do not have holes that HIV can pass through
- Are used by married couples; they are not only for use outside marriage
- Do not cause illness in a woman because they prevent semen or sperm from entering her body
General Advantages
- Effective when used correctly
- No medical supervision required
- Convenient to carry
- Prevents both pregnancy and STIs including HIV/AIDs
- Easy to use
- Reduce risk of systemic side effects and reaction
- Fairly cheap and available in almost every places
General Disadvantages
- There is loss of spontaneity
- May rupture or lose position during intercourse
- It is often associated with extra marital sex and STIs
- It is not suitable for poorly motivated persons
- There is lack of privacy while purchasing condoms
- It cannot be used by a man who cannot maintain erection
- Requires male responsibility
- It is considered unclean to some people

Spermicides
This involves application of chemicals into the vagina to prevent pregnancy.
Mode of action
- Aims at killing or inactivating sperms
Forms of Spermicides
- Jellies
- Creams
- Foams
- Tablets
- Lubricants in condoms
- Ingredient in vaginal sponge
Advantages
- Available without prescription
- Fairly effective if used correctly
- Can be used as backups
- Used only if required
- Control is in the hand of a woman
- Provide extra-vaginal lubrication
- Protects against some STIs and PIDs
Disadvantages
- Not effective when used alone
- Some couple find the method messy i.e. too fluidic
- Associated to some allergic reaction
- Interrupts sexual intercourse
Intra-Uterine Contraceptive Device (IUCDs)
These are devices inserted into the woman uterus to prevent implantation of the fertilized ovum by local inflammation.
Types of IUCDs
- Copper T 380A effective for 10-12 years
- Multi-load 375 for 5 years
- Mirena R hormonal IUCD
Advantages
- It is very effective since it starts working right way
- She does not need to keep coming for refill
- Can offer protection up to 10 years and above
- Fertility returns is immediate
- Limited side effects reported as compared to other methods
- Does not interfere with sexual intercourse
- Has no effects on breastfeeding
- Only one follow up is needed unless there are problems
Side effects
- Increases menstrual bleeding
- Spotting
- Abnormal vaginal discharge
- Menstrual cramps
- PID
Indications
- Breastfeeding
- Women of any age
- As for POP
Contraindications
- Irregular vaginal bleeding of unknown origin g. cancer of cervix
- Pregnancy
- Heavy and painful menstruation
- Cancer of the uterus
- Current PIDs
- Multiple sexual partners
- Pregnancy
IUCDs users who develop PID should be treated with the IUCD in place if they want to continue using it. If no improvement within 72 hours, remove it.
Insertion of IUCD Timing of IUCD insertion
- Any time provided pregnancy is ruled out
- The first seven days of the menstrual cycle
- Immediately following delivery or any time within 46 hours after childbirth
- Any time beyond four to six weeks after childbirth
- Immediately or within seven days after an uncomplicated abortion
- During caesarean section
Procedure
- Consider aseptic technique like hand washing, wearing sterile gloves.
- The device is put in an introducer and plunger.
- It straightens inside the introducer.
- Insert a Cusco ‘s vaginal speculum and clearly visualize the cervix.
- Clean the cervix and vaginal vault with sterile swabs.
- Measure the length of the uterus with a uterine sound.
- Insert the introducer into the uterus through the cervix.
- The plunger is gently pushed to force device out of the introducer into the uterus.
- In the uterus, the device resumes its original shape and lodges against the uterine walls.
- The two small strings attached to the device hang down through the cervical opening.
- Cut the string with a pair of scissors to reduce the size approximately 3cm hanging out of the cervix.
- After the insertion, the client She can remain on the procedure table until she feels ready to get dressed.
- The woman usually feels the strings in the vagina to ensure that the device is in position.
Post insertion instructions
- To use back up for a minimum of 3 days.
- There may be some slight pain which does not require medication.
- To check the string during menstruation to ensure that it is in place or come back if it is removed or dislodged.
- To return to the facility immediately in case of any discomfort.
Removing the IUDs
- In case a client is finding side effects difficult to tolerate, first discuss the complaints the client has. Weigh if she would rather try to manage the problem or to have the IUD removed.
- Removing IUD is usually It can be done any time of the month.
- Removing may also be easier during monthly bleeding, when the cervix is naturally In cases of uterine perforation or if removal is not easy, please refer the client to an experienced service provider to employ appropriate removal technique.
Steps for IUD removal
- Explain what you are going to do to the client during removal
- Ensure privacy & confidentiality at all times
- Request the client to lie on her back
- The provider inserts a vaginal speculum to visualize the cervix & UID strings
- Carefully cleans the cervix & vagina with an antiseptic solution such as Savlon & do inspection
- The provider requests the client to take slow, deep breaths & to Inform the client to make you know in case she feels pain or any other discomfort during the procedure
- Using narrow forceps, the provider gently pulls the IUD strings & slowly until it comes completely out of the cervix
- Show the removed IUD to the client & let her handle with the hands. This helps to make the client understands that nothing has remain inside the uterus.
- Thank the client for cooperating throughout the procedure
- Clear away
Reasons for missed threads in IUDs
- Coiled thread inside
- Thread torn through
- Device expelled outside unnoticed by the client
- Device perforated the uterine wall and is lying in the peritoneal cavity
- Device pulled by the growing uterus in pregnancy
Methods of identification
- History taking i.e. exclude pregnancy
- Ultrasonography
- Hysterectomy
- Hysteroscopy
- Straight x-ray