Table of Contents
ToggleAnaemia In Pregnancy
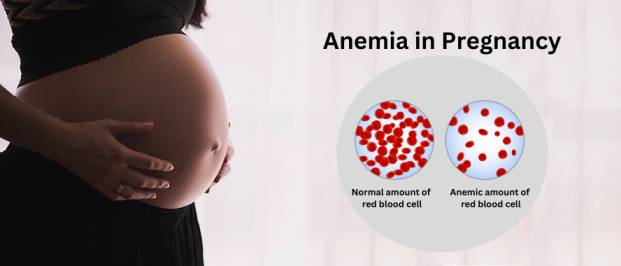
Anaemia means a reduction in oxygen carrying capacity or in quantity of red blood cells.
This may be due to:
> A reduction in number of the red blood cells
> A low concentration haemoglobin
> A combination of both
Degrees
- Mild – 80% = 11 g/dl – 12.5 g/dl
- Moderate – 70% = 8-10.3
- Severe – 60% = 7 g/dl and below
OR
- Mild – 9.0g/dl
- Moderate – 7.8g/dl
- Severe – 6g/dl
Causes
Social and economic factors;
- Ignorance about utilization of food
- Poverty unable to buy the high protein foods
- Native medicine
- Unstable country / Insecurity
- Beliefs – cultural superstition which forbid women from taking certain foods for example chicken and eggs
Obstetrical causes
- Frequent child bearing
- Repeated haemodilution
- Multiple pregnancy due to high fetal demand
- Hyperemesis gravidarum leading to poor absorption of Vitamin B12
- Abortions, ruptured ectopic, PPH, APH, and heavy periods
Medical causes
- Frequent attacks of malaria
- Hookworm infestation
- Infections such as septicaemia, TB
- Sickle cell anaemia
- Drugs like Chloramphenical
Types of Anaemia
- Physiological anaemia.
- Nutritional anaemia.
- Aplastic anaemia.
- Haemorrhagic anaemia.
- Haemolytic anaemia.
- Pernicious anaemia.
- Physiological anaemia: This is the type of anaemia that occurs during pregnancy due to haemo-dilution that occurs during pregnancy where the blood plasma is increased by 25-30%.
- Nutritional anaemia: This is the type brought about about by poor diet whereby there may be deficiency in:
> Folic acid which is responsible for the RBC development bringing about megoblastic anaemia, (Immature Red blood cells)
> Iron deficiency anaemia which is due to the increased fetal demand from the 28th week of pregnancy or due to excessive morning sickness, vitamin B12 and vitamin c deficiency with lack of protein leading to pernicious anaemia. - Aplastic anaemia: This is due to the damage of the red bone marrow caused by prolonged use of chloramphenical depressing the bone marrow
> Radiation where insufficient protection from the x-rays was not provided
> Diseases such as cancer and leukaemia
> Poison from insecticides - Haemorrhagic anaemia: This when there is increased blood loss as may occur in the following cases
> Frequent child bearing that the mother does not get time to regain her haemoglobin levels
> Worm infestation such as hookworms
> Abortions, PPH and APH
> Ruptured ectopic pregnancy
> Trauma and accidents
> Haematemesis and haemoptysis - Haemolytic anaemia: This is when there is increased blood destruction due to:
> Infections such as septicaemia, Pyelonephritis and Bacterial Streptococcus
> Diseases for example malaria
> Mis-crossmatched transfusion
> Sickle cell disease – big spleen disease
> Drugs for example primaquine - Pernicious anaemia
This is when the intrinsic factor is missing leading to mal absorption of vitamin B12. It may occur in the following conditions:
> Diseases of the stomach for example cancer
> Hyperemesis gravidarum
> Surgical operations for example gastrectomy. However, this condition rarely occurs during child bearing age
Signs and symptoms
On history taking
- Patient gives history of general body weakness
- Dizziness
- Faintness
- Palpitations
- Loss of appetite (Anorexia)
- Headaches
- Breathlessness
- History of heavy bleeding may be there
On Examination
- Pale mucus membranes and conjunctiva for example gums, kips, tongue, soles of the feet and palms of the hands
- Distention of the jugular veins
- In severe cases oedema of the ankles, feet or it may be generalized
- On abdominal palpation, there may be enlarged spleen and liver
- Jaundice
Laboratory Tests
Haemoglobin level will be low below 12.5 g/dl
Diagnosis
Based on three factors:
- History taken from the patient about her home including the surrounding
diet, parity and hygiene. - Examination of the patient to detect pale mucus membranes and venous return for example oedema of the upper limbs, wedding rings and puffiness of the face.
- Investigations: Investigations carried out
(a) . Haemoglobin estimation that any haemoglobin of 10 g/dl or below is regarded as anaemia
(b) . Packed cell volume (Normal is 40%)
(c) . Blood film – thick to identify the shape, maturity and consistency, thin red blood cells.
(d) . BS for malarial parasites
(e) . Sickling test to exclude abnormal cells
(f) . Blood film for the thin:
- Microcytosis and hypochromia for iron deficiency
- Megaloblastic cells – Normochromic for vitamin B12 and folic deficiency
- Sickle cell disease
- Target cells
- Reticulocytes for haemolysis whether its going on mainly in the spleen, whether it is a mixture of no. 1 and 2 which will be indicating nutritional
anaemia
(g) . Coombs test for haemolytic anaemia to see whether the mother s developing antibodies against the red blood cells. Usually gets recurrent anaemia.
(h) . Bone marrow – to confirm the shape of the cells
(i) . Urinalysis for protein indicating damage to the kidney. Microscopic – for put
cells in case of severe pyenehiritis
(j) . Stool for intestinal parasites, the commonest is hookworm anaemia
(k) . Haemoglobin: Electrophoresis to confirm SCD
Effects of anaemia on pregnancy and labour
- General body fatigue with tiredness, breathlessness, palpitations and headache.
- Placental insufficiency due to lack of oxygen may lead to:
> Intra-Uterine Fetal Death – intra uterine fetal death
> Small for dates
> Neonatal death
> Abortion and premature labour - Post partum haemorrhage
- Stress of labour may not be tolerated by a very anaemic and even minor blood loss may be fatal
- Fetal and maternal distress leading to instrumental delivery
- May go into heart failure
- More likely to have venous thrombosis
- Less resistance to infection
- Poor lactation
Management
Will depend on the severity of the grade of anaemia, stage of gestation and investigation or cause.
Early pregnancy with mild or moderate anaemia in a maternity centre and hospital
A mother with mild or moderate anaemia treated as an out patient.
- Put the mother in bed
- Take history from the mother concerning the type of diet way of living and her surrounding to know the cause of anaemia
- Carry out general examination for degree of anaemia by use of a tallquist book
- The midwife is only allowed to treat mild and moderate anaemia in early pregnancy
- The condition is managed according to the cause
- If no clinical examination the haemoglobin is found to be below 60% is sent to the hospital for investigations
Active Treatment
For a mother with haemoglobin of 60% and above may be treated with the following:-
- Where malaria is common, the mother is given three doses of Fansidar 960 mgs tablets.
- Mebendazole 200 mgs bd x 3 days for hookworm
- Iron therapy of ferrous Sulphate and folic acid then review after 2 months, ferrous sulphate 200 mgs bd, forric acid 5 mgs od
NB. In the maternity centre moderate anaemia in late pregnancy, refer to hospital.
In the hospital
- Admit in the hospital in Antenatal ward
- Take history about the diet, environment and hygiene
- Observations – temperature, Pulse, Respirations and blood pressure taken
- Any underlying cause will be treated accordingly
- The mother is given routine nursing care
- Proper hygiene
- Given a high protein diet
Severe anaemia in early pregnancy and late pregnancy
In maternity Centre – refer to hospital please
- In Hospital
- The mother is admitted and history taken
- Observations and investigations carried out
- Patient is resuscitated immediately with:
(a) Blood transfusion or parenteral iron dextran (Inferon) infusion if blood is not available. (N.B Total dose of inferno is given slowly and only in severe anaemia nearly to the time of delivery, and after delivery, should be transfused with packed cells under Lasix.) - Dueretics are given for example lasix 120 mg IV
- The patient with severe anaemia should be nursed propped up in bed and given all the care of a very ill patient.
- Mouth should be given special attention as stomatitis and glossitis are common in anaemia patients diet – high protein diet with green vegetables plus fresh fruit
- Strict fluid balance chart, observe for signs of impending cardiac failure which are raising pulse and respirations. Should report breathlessness if the patient has tuberculosis
N.B. IV inferon – 5 ampoules of 250 mgs each in 100 mls of dextrose 5% or normal saline 500mls.
Prevention of anaemia
- Good antenatal care – by detecting anaemia and malaria early and treat them.
- Health education about diet, personal hygiene, environmental, sanitation by proper use of latrines
- Protection against malaria
- Reduce blood loss in 3rd stage even after by good management of all the stages of labour
- Replace proteins at least during lactation by giving extra protein
- Administration of extra Iron and folic acid
- To carry out the routine examination of blood for haemoglobin
Advice to the mother
- Explain to the mother the reason why she has become anaemic, dangers of anaemia and how to prevent it.
- Rest to avoid overworking
- Diet and types of food
- Advise the mother to take any treatment ordered regularly
- The need to prevent mosquitoes to avoid malaria
- To avoid frequent child bearing (family planning)
- To deliver in the hospital
In labour
- Good management of 3rd stage of labour to prevent much blood loss
- Administration of iron during puerperium
On discharge
- Tell the mother to report immediately when they become pregnant in order to receive appropriate prophylactic treatment of iron therapy