Table of Contents
ToggleAfrican Trypanosomiasis (Sleeping Sickness)
Trypanosomiasis, commonly known as African trypanosomiasis or sleeping sickness, is a parasitic disease caused by protozoa of the genus Trypanosoma.
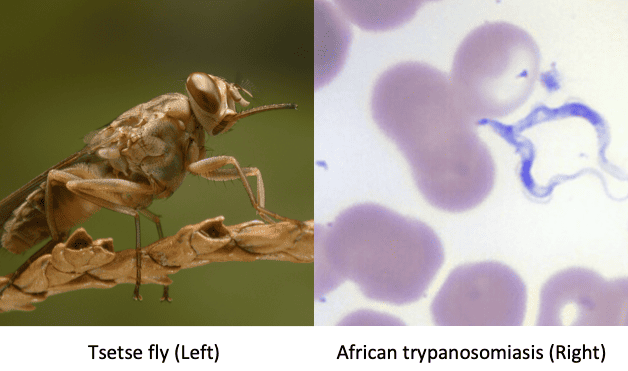
These parasites are transmitted by the tsetse fly and affect both humans and animals. The disease is endemic to sub-Saharan Africa and can be fatal if left untreated.
Aetiology:
Trypanosomiasis is caused by two main species of Trypanosoma:
- Trypanosoma brucei rhodesiense (TBr): This species causes the acute form of the disease and is predominantly found in East and Southern Africa.
- Trypanosoma brucei gambiense (TBg): This species causes the chronic form of the disease and is prevalent in West and Central Africa.
Life Cycle:
Vector (Tsetse Fly):
- Infective stage: The tsetse fly ingests trypanosomes in the metacyclic trypomastigote stage from an infected host.
- Multiplication: Within the fly’s gut, trypanosomes transform into procyclic trypomastigotes and multiply.
- Migration: The trypanosomes migrate to the salivary glands of the fly and differentiate into metacyclic trypomastigotes, the infective stage for humans and animals.
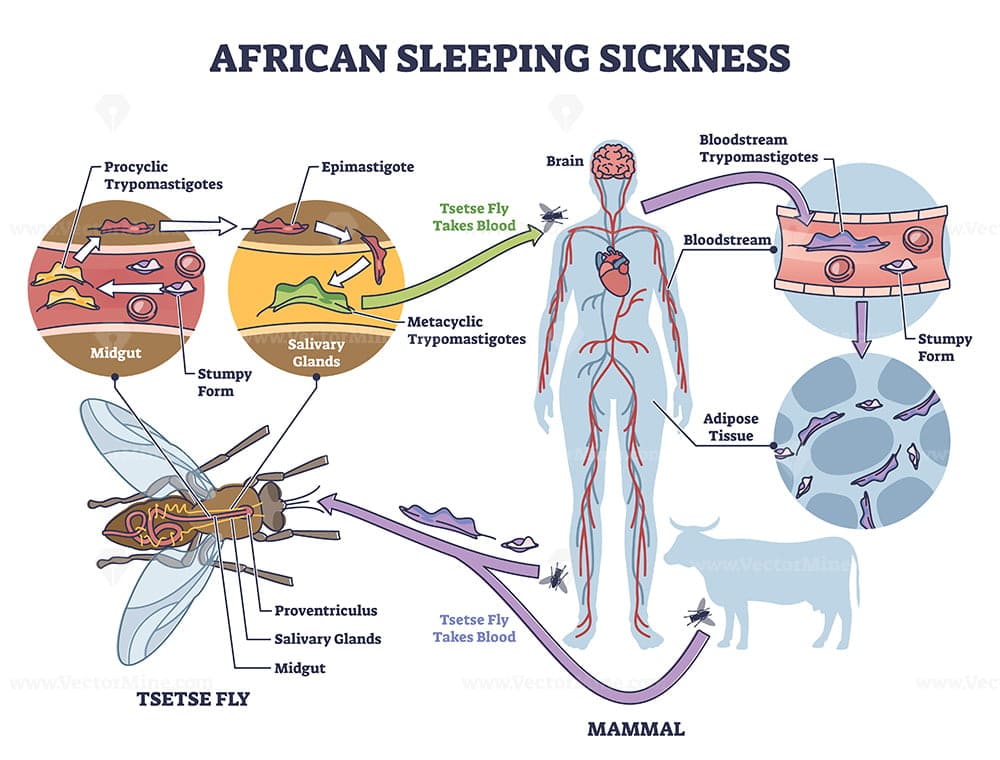
Human:
- Infection: Metacyclic trypomastigotes are injected into the bloodstream during a fly bite.
- Multiplication: The trypanosomes multiply in the bloodstream as bloodstream trypomastigotes.
- Spread: They can cross the blood-brain barrier, reaching the CNS and transforming into meningoencephalitic trypomastigotes.
Forms of Transmission:
- Tsetse fly: This is the primary mode of transmission. The fly acquires trypanosomes by feeding on an infected animal or human. During its subsequent feedings, it injects the parasites into the bloodstream of its new host.
- Blood transfusion: While rare, the disease can be transmitted through contaminated blood transfusions.
- Mother to child: Transmission from mother to child can occur during pregnancy or childbirth.
Hosts:
- TBg: Pigs, dogs, antelopes, cows, sheep, goats, humans.
- TBr: Antelopes, pigs, and humans (humans are the most common source of infection).
Vectors:
- Glossina palpalis (Riverine type): Breeds along rivers and lakes and transmits mainly T. b. gambiense.
- Glossina morsitans (Wounded type): Stays in open, lightly wooded, packed land away from water and transmits T. b. rhodesiense.
Pathogenesis:
Trypanosomiasis arises when humans or animals are infected with trypanosomes through the bite of an infected tsetse fly. The parasite enters the bloodstream and multiplies, eventually reaching the central nervous system (CNS) in the later stages of the disease.
- Toxins: Trypanosomes produce toxins that damage tissues, causing inflammatory changes at the primary chancre, skeletal and heart muscles.
- CNS damage: Toxins may destroy ependymal cells lining the brain ventricles, interfering with serotonin release and causing sleep disturbances.
- Hypersensitivity reactions: The presence of trypanosomes may cause itching (pruritis) and hives (urticaria).
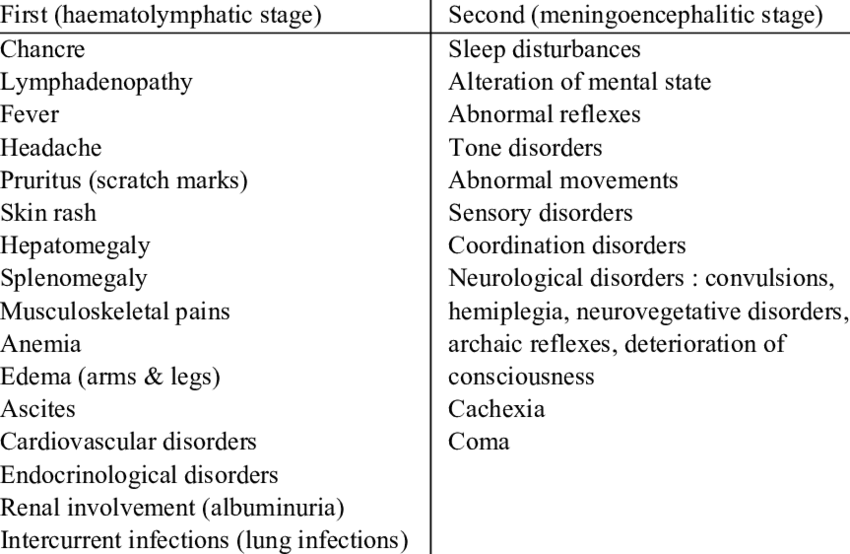
Clinical Presentation:
Onset: Both TBg and TBr follow a similar course, but TBr is often acute and virulent, leading to death within 2-3 years if untreated.
Stage 1: Primary/ Chancre Stage
- History of bite
- Local swelling/ nodule at the bite site, possibly hardened and reddened.
- The chancre may resemble a large boil, but with less pain.
- This stage can last 1-2 weeks and may resolve.
Stage 2: Blood Stage/ Systemic Stage/Haematolymphatic stage.
- Fever: Intermittent fever
- Lymphadenopathy: Swollen spleen and cervical lymph nodes (due to lymphatic spread).
- Physical weakness: Loss of strength accompanied by fever.
- Itchy rashes: Skin patches (15-30 cm in diameter) on the chest and back due to hypersensitivity to trypanosomes.
- Dyspnoea: Shortness of breath due to pericardial effusion and congestive heart failure in chronic cases (TBr).
- Hepatomegaly: Enlarged liver due to liver damage in chronic cases, with potential jaundice.
- Pitting oedema: Swelling on the face, lower limbs, eyelids, and abdomen due to cardiac failure or kidney damage.
- Neurological pains: Muscle cramps are common.
- Reduced appetite and weight loss: Due to constant sleeping and difficulty eating.
- Menstrual irregularities: Amenorrhoea in women.
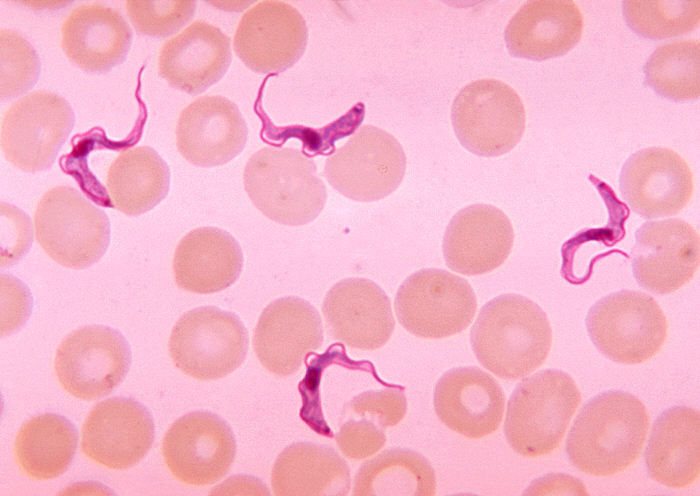
- Anaemia: Due to the destruction of red blood cells by the trypanosomes.
Stage 3: CNS Stage/ Meningoencephalitis
This stage develops after several months or years of infection, but can occur more rapidly in the acute form (TBr). It’s characterized by involvement of the central nervous system.
Sleep disturbances:
- Daytime sleepiness, lethargy, and coma.
- Nighttime insomnia, restlessness, and nightmares.
Behavioral changes:
- Confusion, apathy, and disorientation.
- Personality changes, including aggression and irritability.
- Hallucinations and delusions.
Neurological signs:
- Motor incoordination: Tremors, jerky movements, paralysis (facial palsy, limb weakness, difficulty swallowing), ataxia (unsteady gait).
- Sensory disturbances: Numbness and tingling sensations.
- Headache: Often severe and persistent.
Meningitis:
- Stiff neck (meningismus)
- Photophobia (sensitivity to light)
- Fever
- Nausea and vomiting
Other Symptoms:
- Swelling: The face and limbs may become swollen, especially in the late stages.
- Cardiac complications: Irregular heartbeat, heart failure, and pericarditis can occur.
- Renal complications: Kidney failure can occur in later stages.
Diagnosis:
Clinical examination: Evaluating the patient’s history, symptoms, and neurological signs.
Laboratory investigations:
Microscopy:
- Wet blood smear: Examination of a fresh blood sample under a microscope for the presence of trypanosomes.
- Thick blood smear: A higher concentration of blood is used to improve detection of trypanosomes.
- Staining: Using Giemsa or Wright’s stain to visualize the trypanosomes.
Serology: Blood tests to detect antibodies against trypanosomes.
Lumbar puncture (LP): A spinal tap to collect cerebrospinal fluid (CSF) for examination.
- Microscopy: Examining the CSF for trypanosomes, especially in the meningoencephalitic stage.
- Biochemical analysis: Measuring protein levels and cell counts in the CSF.
Molecular methods: PCR testing can be used to detect trypanosome DNA, especially in the early stages of infection.
Differential Diagnosis:
- Malaria: Can present with fever, chills, sweating, and headaches.
- Tuberculosis (TB): Can cause fever, weight loss, and night sweats.
- Meningitis: Can cause headache, fever, stiff neck, and altered mental status.
- HIV/AIDS: Can cause fever, weight loss, and neurological symptoms.
- Other infections: Meningococcal meningitis, encephalitis, and viral infections.
Management:
Early Stages:
- Suramin: Given intravenously (IV) every 3-5 days for 6-7 doses. Effective against bloodstream trypanosomes, but not CNS involvement.
- Pentamidine: Given intramuscularly (IM) daily for 7-10 days. Effective against bloodstream trypanosomes.
Late Stages (CNS Involvement):
- Melarsoprol (MEL.B): The only drug effective against trypanosomes in the CNS. Given intravenously and requires careful monitoring due to potential side effects.
- Eflornithine: Alternative treatment for late-stage disease, especially in pregnant women.
Supportive Care:
- Bed rest: To reduce the risk of complications and improve recovery.
- Hydration: To prevent dehydration.
- Nutrition: Adequate nutrition is essential to support the body’s fight against infection.
- Symptom management: Medication for fever, headache, and other symptoms.
Prevention and Control:
- Vector control: Reducing the tsetse fly population through insecticides, traps, and clearing of vegetation in endemic areas.
- Early diagnosis and treatment: Active screening and case finding programs are crucial for timely treatment and preventing the spread of the disease.
- Sleeping sickness awareness: Public health education about the disease, its transmission, and prevention measures.
Prognosis:
- Untreated: The disease is almost always fatal.
- Treated: Early treatment is important for a positive prognosis. Late-stage treatment is more challenging and has a higher risk of complications.
Nursing Management:
- Assessment: Monitor vital signs, neurological status, and symptoms.
- Medications: Administer medications according to the doctor’s orders and monitor for side effects.
- Hydration: Ensure adequate fluid intake to prevent dehydration.
- Nutrition: Provide a balanced diet to support the body’s recovery.
- Comfort: Provide comfort measures for symptoms like fever, headache, and pain.
- Patient education: Educate the patient and their family about the disease, its management, and preventive measures.
Early Stage Treatment: Trypanosoma rhodesiense sleeping sickness: For both children and adults: Suramin is the drug of choice for early-stage T. rhodesiense infection. Dosage:
Trypanosoma gambiense sleeping sickness:
Late Stage Treatment: Trypanosoma rhodesiense sleeping sickness:
Trypanosoma gambiense sleeping sickness: Children ≤ 12 years and <35 kg: Eflornithine is the preferred treatment.
Children >12 years up to 15 years: Eflornithine is the preferred treatment.
Adults >15 years:
Relapses: If a relapse occurs, IV melarsoprol at 2.2 mg/kg once daily for 10 days is used. Important Notes: Corticosteroids:
Suramin:
|

Appreciative 😊
Quite enlightening even for non-biological readers. Because the vector-borne diseases may affect every person/creature even after a long time.