Table of Contents
ToggleHAEMORRHAGIC FEVERS
Ebola and Marburg
- Ebola and Marburg are severe zoonotic multisystem febrile diseases caused by RNA viruses. They are notifiable diseases.
Ebola Virus:
- Morphology: The Ebola virus is filamentous, often resembling a “U” or “S” shape. It measures approximately 2 μm (micrometers) in length and 70-80 nm (nanometers) in diameter. It has an internal structure (nucleoprotein core) enclosed within an external envelope studded with numerous glycoprotein spikes.
- Multiplication: The virus replicates by budding from its internal structures.
Types of Ebola Viruses:
Ebola Virus (EBOV): This is the species most commonly associated with severe outbreaks in humans.
- EBO-Zaire (EBO-Z): This subtype has a high fatality rate, averaging around 89%.
- EBO-Sudan (EBO-S): This subtype has a fatality rate of 41.65%, although this can vary depending on factors like treatment and location.
Vectors:
- Mosquitoes and Termites: While there have been theories suggesting these insects could play a role in transmission, there is no definitive evidence to support their role as vectors for Ebola.
- Bats: The most likely primary reservoir for Ebola viruses. They can harbor the virus without showing symptoms and transmit it to other animals or humans.
- Dogs: While some sources mention dogs, there is no clear evidence to suggest they are a significant reservoir for Ebola.
Transmission:
Human-to-Human:
- Direct contact with infected bodily fluids, such as blood, vomit, feces, urine, and saliva.
- Contact with contaminated materials like clothing, bedding, needles, and medical equipment.
- Sexual contact with a survivor who is still shedding the virus in semen (this can last for months after recovery).
Animal-to-Human: Contact with infected animals (particularly primates like chimpanzees and gorillas) or their bodily fluids.
Mosquitoes: As mentioned above, mosquitoes are not considered reliable vectors for Ebola virus transmission.
Pathology:
The Ebola virus affects multiple tissues throughout the body, not just a specific organ. It causes widespread damage, including:
- Necrotic Lesions: The virus leads to cell death (necrosis) in various organs, affecting their functionality.
- Immune System Suppression: Ebola weakens the immune system, making individuals vulnerable to other infections.
Incubation Period:
- Primary Infection: The incubation period typically ranges from 2 to 21 days after exposure.
- Secondary Infection: For transmission from human to human, the incubation period is the same, 2 to 21 days.
Causes:
Ebola Virus: The causative agent is the Ebola virus, a member of the Filoviridae family. There are five known species of Ebola virus:
- Zaire ebolavirus (responsible for the most severe outbreaks)
- Sudan ebolavirus
- Reston ebolavirus (not known to cause disease in humans)
- Taï Forest ebolavirus
- Bundibugyo ebolavirus
Marburg: Marburg virus
Risk Factors:
- Communities Around Game Parks: Proximity to wildlife increases the risk of exposure.
- Endemic Areas: Regions with a history of EVD outbreaks.
- Cultural Practices: Burial rituals involving close contact with the deceased can facilitate transmission.
- Poor Infection Control: Inadequate sanitation and hygiene practices in healthcare settings can increase the spread.
- History of Exposure: Contact with infected individuals within 2-21 days prior to symptom onset (e.g., sexual partners, breastfeeding mothers).
- Contact with Infected Animals: Handling infected animals (like monkeys, bats, and infected game meat).
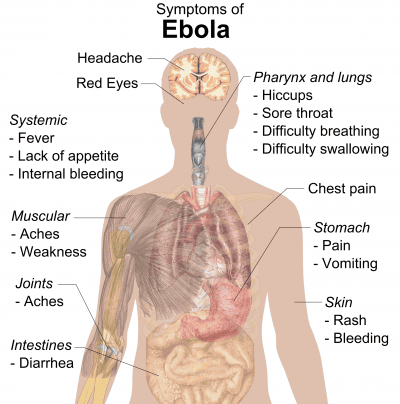
Clinical Features:
Early Signs (Non-Specific):
- Sudden Fever: A rapid onset of high fever (often exceeding 101.5 °F / 38.6 °C).
- Weakness: General feeling of weakness and exhaustion.
- Headache: Intense headache.
- Muscle Pain: Pain in muscles and joints.
- Loss of Appetite: Decreased appetite or inability to eat.
- Conjunctivitis: Inflammation of the conjunctiva (white part of the eye).
Late Signs:
- Diarrhea: Profuse diarrhea, sometimes with blood.
- Vomiting: Severe vomiting.
- Mucosal and Gastrointestinal Bleeding: Bleeding from the nose, gums, eyes, and rectum.
- Chest Pain: Pain in the chest area.
- Respiratory Distress: Difficulty breathing.
- Circulatory Shock: Low blood pressure and impaired blood flow.
- CNS Dysfunction: Confusion, seizures, and coma.
- Miscarriage in Pregnancy: EVD can cause miscarriage or stillbirth in pregnant women.
- Elevated AST and ALT: Elevated levels of liver enzymes, indicating liver damage.
- Kidney Injury: Damage to the kidneys, potentially leading to kidney failure.
- Electrolyte Abnormalities: Imbalances in electrolytes (minerals like potassium and sodium) in the body.
Other clinical presentations include;
- Sudden Onset: Symptoms usually appear abruptly.
- Severe Headache: Intense headache is a common initial symptom.
- Myalgia and Fever: Muscle pain (myalgia) and high fever (often exceeding 38.5 °C).
- Conjunctival Inflammation: Inflammation of the conjunctiva (white part of the eye).
- Gingival Bleeding: Bleeding from the gums.
- Sore Throat: Sore throat with associated chest pain.
- Abdominal Pain: Pain in the abdomen.
- Nausea, Vomiting, and Diarrhea: These symptoms are prominent features of EVD, with diarrhea often being profuse and watery.
- Signs of Dehydration: Dehydration can develop due to fluid loss from vomiting and diarrhea.
- Severe Bleeding: Internal and external bleeding may occur from the gastrointestinal tract, gums, nose, and other orifices. This typically develops between the 5th and 7th days.
- Morbiliform Rash: A rash similar to measles may appear on the 7th day.
- Neurological Manifestations: Neurological complications such as psychosis and hemiplegia (weakness or paralysis on one side of the body) can occur.
- Death: Death often occurs around the 9th day, but can happen between the 2nd and 21st days.
Note: Hemorrhage is not always a prominent feature of EVD. It’s important to remember that EVD symptoms can vary significantly.
Differential Diagnosis:
- Malaria: A parasitic disease that also causes fever, headache, and muscle aches.
- Meningitis: Inflammation of the membranes surrounding the brain and spinal cord.
- Shigellosis: A bacterial infection causing diarrhea, abdominal cramps, and fever.
- Typhoid Fever: A bacterial infection causing high fever, headache, and constipation.
- Anthrax: A bacterial infection causing skin lesions, fever, and respiratory problems.
- Sepsis: A serious bacterial infection causing fever, chills, and rapid heart rate.
- Viral Hepatitis: Inflammation of the liver caused by viruses like hepatitis A, B, or C.
- Dengue Fever: A viral infection transmitted by mosquitoes, causing fever, headache, and muscle pain.
Investigations:
Blood Sample for Specific Testing: Blood samples from suspected EVD cases should be collected by trained healthcare professionals wearing proper PPE.
- Laboratory Testing: The blood sample needs to be sent to a reference laboratory for specific tests to identify the Ebola virus.
- Real-Time PCR: This is the preferred method for detecting Ebola virus.
- Antigen and Antibody Detection: ELISA (enzyme-linked immunosorbent assay) and other antibody tests can identify Ebola virus antigens and antibodies.
Postmortem: If an individual dies from EVD, postmortem examination is critical for confirmation and to prevent further spread.
Notification: Immediately notify the district surveillance focal person if you suspect a case of EVD.
Management
Management Aims:
- Fluid Replacement: Maintain adequate hydration to compensate for fluid loss.
- Prevention of Spread: Isolate the patient and implement strict infection control measures.
- Conservation of Energy: Provide rest and supportive care to conserve energy.
- Symptom Relief: Administer medications to manage symptoms like fever, pain, and vomiting.
Specific Management:
1. Admission: Admit the patient to an isolated room in a medical ward, providing complete bed rest.
- Bed Preparation: Use a freshly prepared bed, with a comfortable position for the patient (supine or semi-recumbent depending on their condition).
2. Protection:
- Handwashing: Strict handwashing before and after attending to the patient.
- Isolation: Isolate the patient in a designated room, and implement barrier nursing techniques. Healthcare workers and patient attendants should wear gowns, gloves, goggles, and gumboots to prevent contact with bodily fluids.
- Identification Tag: Place an “INFECTIOUS” tag on the door to alert others about the infectious nature of the room.
3. Fluid Replacement: Administer intravenous fluids (N/S, RL, and Dextrose 5%) according to the doctor’s prescription.
4. Hygiene:
- Patient Hygiene: Maintain cleanliness of the patient’s skin, secretions, and stool. Disinfect with bleach solutions before disposal.
- Bed Pans: Scrub bed pans thoroughly with strong detergent, rinse, and dry.
- Patient’s Orifices: Wash and dry the patient’s orifices. Apply perineal pads if needed for profuse diarrhea.
- Linens: Disinfect linens in a bleach solution for at least 6 hours. Label and transport them in “infected linen” bags to be sluiced, boiled, dried, and ironed.
- Room Disinfection: Mop the room, scrub the floors and walls, disinfect lockers, and wash and boil patient utensils for at least 10 minutes.
- Refuse Disposal: Place food and hospital refuse in polythene bags and incinerate.
5. Diet: Provide a fluid diet in the acute stage, primarily through IV fluids and oral fluids as much as possible.
6. Terminal Disinfection: Thoroughly disinfect the room and all contaminated materials after the patient is discharged.
7. Notification: Report the case to health authorities to inform the public health system about the outbreak.
Health Education:
- Patient Attendants: Educate patient attendants about the infection, its mode of transmission, and prevention measures.
- General Public: Inform the general public about the disease, its signs and symptoms, and preventative measures.
- Patient Care: Ensure the patient feels supported and understood, preventing isolation and stigma.
Prevention:
- Avoid Contact: Minimize contact with the patient’s blood and secretions.
- Personal Protective Equipment: Wear proper PPE (gowns, gloves, masks, eye protection) when providing care.
- Safe Burial Practices: Use safe burial practices to prevent transmission during funerals.
- Vaccination: The Ebola vaccine is available and should be considered for high-risk individuals.
- Isolation: Isolate infected individuals in designated Ebola treatment centers.
- Contact Tracing: Identify and monitor individuals who have come into contact with infected persons.
Prevention Complications:
- Shock: Monitor for signs of shock (low blood pressure, rapid heart rate, weakness, and cool, clammy skin).
- Organ Failure: Monitor for signs of organ failure (e.g., jaundice for liver failure, decreased urine output for kidney failure).
- Disseminated Intravascular Coagulation (DIC): Be aware of the signs of DIC (bleeding from multiple sites, bruising, and difficulty controlling bleeding).
- Meningitis: Monitor for signs of meningitis (stiff neck, headache, fever).
- Encephalitis: Monitor for signs of encephalitis (confusion, seizures).
- Secondary Infections: Monitor for signs of secondary infections (fever, cough, difficulty breathing).
- Psychological Trauma: Provide psychological support to patients and their families to address potential psychological trauma.