Table of Contents
ToggleDrugs Used in Anaesthesia
Anaesthesia is defined as the absence of feelings, sensation, or pain. Anaesthetics are drugs that reduce or abolish sensation, affecting either the whole body (general anaesthetics) or a particular area or region (local anaesthetics).
Local Anaesthetics
Local anaesthetics provide brief periods of anaesthesia in a small localized area of the skin and adjacent tissues. They may be administered in two ways: topically for surface anaesthesia and by injection for infiltration anaesthesia.
Topical anaesthetics are usually applied to the skin or the mucous membrane to relieve itching, insect bites, hemorrhoids, pruritus, and minor surgical procedures.
Infiltration anaesthesia may be achieved by injecting a local anaesthetic into the immediate area of surgery. It is commonly used during dental extraction and biopsies.
Examples:
- Lidocaine (lignocaine)
- Bupivacaine
- Mepivacaine
Note: Lignocaine is sometimes combined with epinephrine (adrenaline), a powerful vasoconstrictor, that decreases blood flow to the tissue where it is injected. Adrenaline controls bleeding and also prolongs the anaesthetic action of lignocaine.
General Anaesthetics
General anaesthetic drugs are normally given IV or by inhalation to produce rapid, reversible loss of consciousness and insensibility to surgical stimuli.
Examples:
Inhaled Anaesthetics:
- Halothane
- Nitrous oxide
- Ether
Intravenous Anaesthetics:
- Ketamine
- Midazolam
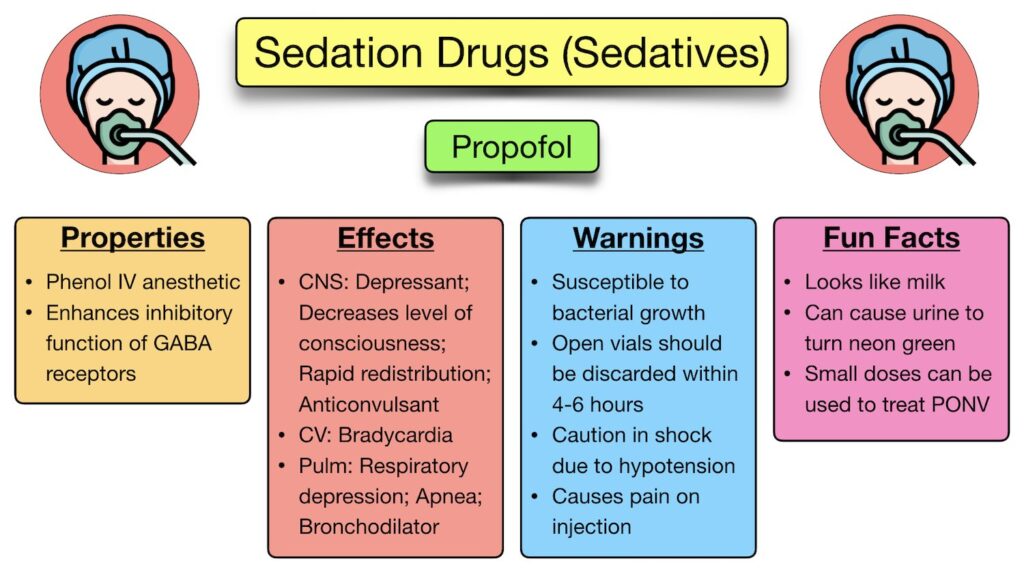
- Propofol
Ketamine
Available Preparations:
- Injection: 50 mg/ml
Available Brands: Ketajex®, Ketalar®
Pharmacokinetics: Ketamine is rapidly and well absorbed after IM injection, rapidly enters the CNS, metabolized by the liver, and excreted in urine.
Indications:
- Induction and maintenance of anaesthesia
- Pain relief
- Diagnostic maneuvers and procedures not involving intense pain
Contraindications:
- Thyrotoxicosis
- Hypertension (including pre-eclampsia)
- History of cerebrovascular accident
- Raised intracranial pressure
- Psychiatric disorders, particularly hallucinations
- Severe cardiac disease
- Recent myocardial infarction
- Stroke
- Known hypersensitivity to ketamine
- Cerebral trauma
- Eye injury
Dosage:
Induction:
- Intravenous Injection: 1-4.5 mg/kg (2 mg/kg usually produces anaesthesia lasting 5-10 minutes)
- Intramuscular Injection: 6.5-13 mg/kg (duration of anaesthesia up to 25 minutes)
- IV Infusion: 0.5-2 mg/kg initially, then infuse at 10-45 mcg/kg/minute, adjust according to response
Maintenance:
- Intravenously: Increments of half or full dose repeated as required
- Analgesic for painful procedures: IV 1-1.5 mg/kg slowly over 2-5 minutes. Give half dose every 10 minutes if required for prolonged procedures
Administration Instructions:
- Dilute dose with an equal volume of water for injection, sodium chloride 0.9%, or glucose 5% before IV injection
- Give IV slowly; rapid administration may result in respiratory depression and enhanced hypertensive response
Side Effects:
- Raised blood pressure and pulse rate
- Increased muscle tone
- Lacrimation
- Hypersalivation
- Raised intracranial pressure
- Redness of the skin
- Postoperative nausea and vomiting
- Pain on injection
- Irrational behavior during recovery
Drug Interactions:
- Inhalation anaesthetics such as halothane may prolong the effect of ketamine and delay recovery
- Prolonged recovery occurs when barbiturates or opioids are given concurrently with ketamine
- Ketamine should not be used with ergometrine
- Concomitant use with thyroid hormones may cause hypertension and tachycardia
Key Issues to Note:
- Warn the patient to avoid tasks requiring motor coordination and/or mental alertness for 24 hours after anaesthesia
- Keep verbal, tactile, and visual stimulation to a minimum during induction and recovery
Lidocaine
Available Preparations:
- Solution: 1%, 2%
- Topical Gel: 2-4%
- Combinations: Xylocaine® (Lidocaine + epinephrine)
Note: Epinephrine is often added to delay absorption and thus reduce anaesthetic systemic toxicity and keep it in contact with nerve fibers, prolonging the duration of action.
Pharmacokinetics: Lidocaine is effectively absorbed from the mucous membranes, widely distributed throughout the body, metabolized in the liver, and excreted in urine.
Indications:
- Infiltration anaesthesia
- Surface anaesthesia of mucous membrane
- Dental anaesthesia
- Ventricular arrhythmias
- Relief of pain in hemorrhoids
Contraindications:
- Adjacent skin infection
- Hypersensitivity
- Heart block
- Hypovolemia
- Severe anemia
- Myasthenia gravis
- Spinal anaesthesia in dehydrated patients
Dosage:
Dental Anaesthesia: Using 2% solution with epinephrine
- Adult: 20-100 mg (1-5 ml)
Local Infiltration and Peripheral Nerve Block: Using 1% solution with epinephrine
- Adult: Up to 400 mg (up to 40 ml)
Note: Use lower doses for elderly, epileptic, or acutely ill patients. Do not use solution containing preservatives for spinal, epidural, intravenous, or regional anaesthesia.
Side Effects:
- Dizziness
- Lightheadedness
- Tremors
- Numbness
- Restlessness
- Convulsions
- Unconsciousness
- Headache
- Blurred vision
- Hypotension
- Cardiac arrest
- Backache
- Sense of heat
- Hypersensitivity reaction
- Urinary retention
Drug Interactions:
- Anti-convulsants may increase the cardiac depressant effect of lidocaine
- Cimetidine and beta-blockers may increase plasma concentration of lidocaine, leading to increased risk of toxicity
- Use of opioid analgesics peri-operatively may have additive respiratory and cardiac depressant effects
Key Issues to Note:
- Doses should be reduced in acute and chronic hepatic diseases
- If solutions discolor or precipitate, they should be discarded