Table of Contents
ToggleEndocrine and Metabolic Drugs
Drugs Used in Diabetes Mellitus
Diabetes mellitus is a chronic disorder characterized by hyperglycemia, altered metabolism of carbohydrates, proteins, and fats, due to insulin deficiency or resistance.
Classification of Diabetes Mellitus
Diabetes mellitus is classified into two:
- Type 1 diabetes mellitus
- Type 2 diabetes mellitus
Type 1 Diabetes Mellitus
This type of diabetes is due to autoimmune destruction of the beta cells. It is more common in young children than adults. Patients with type 1 diabetes require exogenous insulin for survival.
Type 2 Diabetes Mellitus
Type 2 diabetes usually presents in obese adults and has a strong family history. It is caused by insulin deficiency and insulin resistance.
Drugs used in the treatment of diabetes mellitus include:
- Oral antidiabetic drugs
- Insulin
Oral Antidiabetic Drugs
Oral antidiabetic drugs are used in the treatment of type 2 diabetes mellitus which has not responded to lifestyle modification.
Classification of Oral Antidiabetics
Oral antidiabetics are classified as follows:
- Sulfonylureas
- Biguanides
- Thiazolidinediones
- Alpha-glucosidase inhibitors
Sulfonylureas
Sulfonylureas are structurally related to sulfonamides. They are divided into generations as follows:
First Generation
- Tolbutamide
- Chlorpropamide
Second Generation
- Glibenclamide
- Glimepiride
- Gliclazide
- Glipizide
Mode of Action
Sulfonylureas act by stimulating insulin secretion from the beta cells of the pancreas, thus increasing insulin levels. Increased insulin secretion results in lowering of blood glucose levels. These drugs are only effective in the presence of functioning beta cells.
Tolbutamide
Available Preparations:
- Tablets: 500 mg
Pharmacokinetics
Tolbutamide is readily absorbed after oral administration, metabolized in the liver, and excreted in the urine and feces chiefly as metabolites.
Indications
- Type 2 diabetes mellitus
Contraindications
- Severe hepatic and renal impairment
- Presence of ketoacidosis
- Breastfeeding
- Pregnancy
- Porphyria
- Insulin-dependent diabetes mellitus
Dosage
- Adult: 500-1500 mg daily in 2 divided doses, max 2 g daily
Side Effects
- Nausea and vomiting
- Constipation
- Dyspepsia
- Hypoglycemia
- Headache
- Diarrhea
- Skin rash
- Tinnitus
- Taste alteration
Drug Interactions
- Beta-blockers may mask hypoglycemic symptoms caused by tolbutamide
- Hypoglycemic effect caused by tolbutamide may be reduced by corticosteroids
- Disulfiram-like reaction may occur when tolbutamide is taken concurrently with alcohol
- Hypoglycemic effect of tolbutamide may be increased by sulfonamide antibiotics, ranitidine, and cimetidine
Key Issues to Note
- Tolbutamide should be given with or immediately after food
- Elderly, debilitated patients, and those with impaired renal or hepatic function usually require a lower initial dose
- Because of its complete metabolism and short duration of action, it is recommended in the elderly
- The drug should not be taken at bedtime because of the potential for nocturnal hypoglycemia
- Avoid alcohol while taking tolbutamide
Glibenclamide
Available Preparations:
- Tablets: 5 mg
Available Brands: Daonil®, Glibol®, Glibetics®, Euglucon®, Betanase®, Diaben®, Glamide®
Combinations: Duotrol® (Glibenclamide/Metformin) 5/500
Pharmacokinetics
Glibenclamide is reliably and almost completely absorbed when taken orally, metabolized in the liver to weakly active metabolites, and excreted in urine and feces.
Indications
- Type 2 diabetes mellitus
Contraindications
- Presence of ketoacidosis
- Type 1 diabetes mellitus
- Severe renal and hepatic impairment
- Pregnancy and breastfeeding
- Previous hypersensitivity to the drug
Dosage
- Initially 5 mg in the morning, dose adjusted according to response, max 15 mg/day
Side Effects
- Headache
- Weakness
- Epigastric fullness
- Hypoglycemia
- Dizziness
- Nausea
- Weight gain
- Heartburn
Drug Interactions
- Beta-blockers may mask warning symptoms of hypoglycemia caused by glibenclamide
- Hypoglycemic effect of glibenclamide is reduced by drugs which are insulin antagonists such as bendrofluazide, oral contraceptives, and glucocorticoids
- Metformin has a synergistic hypoglycemic action with glibenclamide
- Alcohol increases the hypoglycemic effect caused by glibenclamide and may also cause disulfiram-like reaction
- An enhanced hypoglycemic response to glibenclamide may occur when given together with drugs such as aspirin, cimetidine, fluconazole, and ketoconazole
Key Issues to Note
- Glibenclamide should be given with or 30 minutes before a meal
- Warn the patient of the possibility of hypoglycemia and advise on how to manage it
- Encourage the patient to maintain lifestyle modifications
- Glibenclamide tablets should be stored in a cool, dry place and protected from light
- Avoid alcohol while taking the drug
Biguanides
Biguanides are the drugs of choice in the treatment of type 2 diabetes mellitus in overweight patients. They do not increase insulin secretion; therefore, they do not usually cause hypoglycemia or weight gain. Metformin is the only available biguanide. It may be combined with a sulfonylurea to provide better glycemic control.
Mode of Action
Biguanides act by decreasing the production of glucose by the liver and also promote the uptake of glucose by tissues.
Metformin
Available Preparations:
- Tablets: 500 mg, 850 mg, 1000 mg
Available Brands: Glyformin®, Glucophage®, Glucomet®, Metformin-Denk®, Glycomet®, Bigomet®
Combinations:
- Avandamet® (Rosiglitazone/Metformin) 2/500
- Pionorm-M® (Pioglitazone/Metformin) 30/500
- Piosafe-M® (Pioglitazone/Metformin) 15/500
Pharmacokinetics
Metformin is slowly and incompletely absorbed when taken orally. Food delays or decreases the extent of absorption. It is excreted mainly as unchanged drug in urine.
Indications
- Type 2 diabetes mellitus
- Polycystic ovary syndrome
Contraindications
- Pregnancy
- Hepatic dysfunction
- Acute metabolic acidosis
- Pancreatitis
- Renal dysfunction
- Breastfeeding
Dosage
- Initially 500 mg with breakfast for 1 week, then 500 mg with breakfast and evening meal for at least 1 week, then 500 mg with breakfast, lunch, and evening meal, max 2 g daily in divided doses
Side Effects
- Nausea
- Anorexia
- Rash
- Lactic acidosis
- Malabsorption of vitamin B12
- Vomiting
- Diarrhea
- Metallic taste
- Abdominal pain
Drug Interactions
- There is an increased risk of hypoglycemia when metformin is given with digoxin or furosemide
- Alcohol increases the risk of lactic acidosis associated with metformin
- Nifedipine may enhance the absorption of metformin
- Metformin may interfere with vitamin B12 absorption
- Cimetidine increases peak metformin blood concentrations
Key Issues to Note
- Advise the patient not to change or discontinue the drug without consulting the prescriber
- Avoid alcohol during treatment
- Advise the patient to take the drug with meals
- Extended-release tablets should be taken whole without chewing or crushing
Insulin
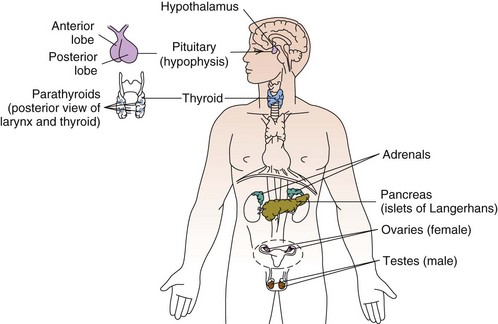
Insulin is a hormone produced by the beta cells of the pancreatic islets of Langerhans.
It plays an important role in the regulation of carbohydrate, protein, and fat metabolism. Insulin lowers blood glucose by inhibiting glycogenolysis and gluconeogenesis in the liver and stimulates glucose uptake by muscles and adipose tissues.
Insulin is used in the treatment of type 1 diabetes mellitus and is also used in type 2 diabetes mellitus in the following cases:
- Severe infection
- Major surgery
- Ketoacidosis
- During pregnancy
- When hyperglycemia does not respond to non-pharmacological measures and oral antidiabetics
Sources of Insulin
Insulin for therapeutic use is extracted from the pancreas of any of the following:
- Cattle
- Pig
- Human
Types of Insulin Preparations
There are 3 main types of insulin preparations which differ in time of onset and duration of action. They include:
- Short-acting insulin (e.g., insulin soluble) – It is the only insulin that can be given by IV bolus, IV infusion, or IM
- Intermediate-acting insulin (e.g., insulin zinc suspension – Lente) – Have slower onset of action but with prolonged duration of action. They are formulated to dissolve more gradually when administered
- Long-acting insulin (e.g., glargine – Lantus) – Has a duration of action of 24 hours
Insulin Administration
Insulin is usually given subcutaneously in the buttock, abdomen, anterior thigh, and dorsal arm. Absorption is usually most rapid from the abdomen, followed by the arm, then the buttock and thigh. The rate of absorption is increased by massage, hot bath, or exercise. The type of insulin used depends on the type of diabetes, patient’s age, and blood glucose levels.
Soluble Insulin
Available Preparations:
- Injection: 100 IU/ml
Available Brands: Actrapid®
Indications
- Type 1 diabetes mellitus
- Diabetic ketoacidosis
- During pregnancy, surgery, trauma, infections, and fever
Contraindications
- Hypersensitivity to insulin
- Hypoglycemia
Dosage
- Insulin dosage is individualized and determined in accordance with the needs of the patient, usual range 0.3-1 unit/kg/day
Side Effects
- Hypoglycemia
- Skin rash
- Edema
- Fat hypertrophy at injection site
- Local reaction
- Urticaria
- Abdominal bloating
- Blurred vision
Drug Interactions
- Alcohol may increase the effects of insulin
- Beta-blockers may mask signs and symptoms of hypoglycemia
- Corticosteroids antagonize effects of insulin and result in increased glucose levels
- ACE inhibitors may increase the hypoglycemic effect of insulin
Key Issues to Note
- Advise the patient to watch out for symptoms of hypoglycemia such as fatigue, confusion, headache, hunger, rapid breathing
- Advise the patient to always carry a quick source of sugar to rectify hypoglycemia when it occurs
- Injection sites should be rotated to avoid lipodystrophy