Table of Contents
ToggleSignificance of female urinary system in obstetrics
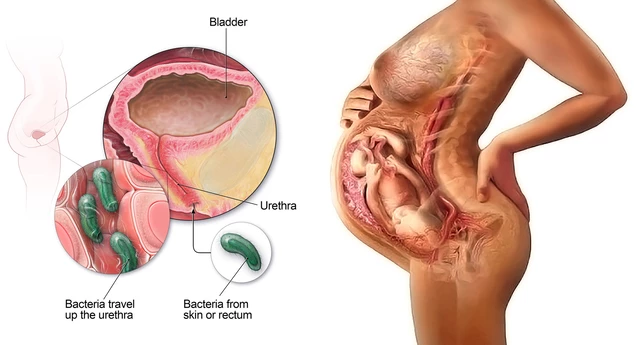
The female urinary system is important in obstetrics because changes to the urinary tract during pregnancy can increase the risk of urinary tract infections (UTIs) and other complications:
- UTIs: UTIs are the most common bacterial infection during pregnancy, affecting up to 18% of pregnancies. Hormonal and mechanical changes during pregnancy can cause urinary stasis, which increases the risk of UTIs. Untreated UTIs can lead to serious complications for both the mother and fetus, such as preterm labor, low birth weight, and fetal death.
- Urinary incontinence: Urinary incontinence (UI) is a common urogenital symptom during pregnancy, affecting between 32% and 64% of pregnant women. UI is usually permanent and can increase toward the end of pregnancy.
- Other urogenital symptoms: Other urogenital symptoms during pregnancy include frequency, nocturia, intermittent urination, straining, genital pain, and discomfort.
The urinary system filters waste from the body, regulates blood pressure and volume, and controls electrolyte and metabolite levels.
THE FEMALE URINARY SYSTEM
COMMON TERMS IN URINARY SYSTEM
- Proteinuria : Daily excretion of proteins in the urine is more than 150mg. It signifies that the kidney is damaged/ perforated.
- Haematuria : Means passing urine containing blood and is due to bleeding into the urinary tract.
- Crystalluria : Presence of crystals like oxalates, phosphates in the urine detected by microscopic examination of urine
- Glycosuria : Means presence of sugar (glucose) in urine either due to diabetes mellitus or due to renal glycosuria
- Azotemia : Increase in the serum concentration of urea and creatinine above their normal values. This occurs when glomerular filtration pressure (GFR) of the kidneys falls due to renal failure. “uremia”.
- Oliguria : Diminished urine volume output of urine i.e. 100 mL to 400 mL per day.
- Anuria – Complete absence of urine formation i.e zero to 100 mL per day
- Dysuria – Difficulty or pain in passing urine
- Polyuria – Urine volume above 3 litres per day
- Retention of urine – occurs due to obstruction of urine outflow from the bladder, this is relieved by catheterization
Anatomy of the Renal System
The urinary system is the main excretory system eliminating waste products from blood through urine.
Its anatomy consists of two kidneys, each joined to the bladder by the tube called ureter, which conveys urine from the kidneys to the bladder for storage. Following bladder contraction, urine is expelled through the urethra.
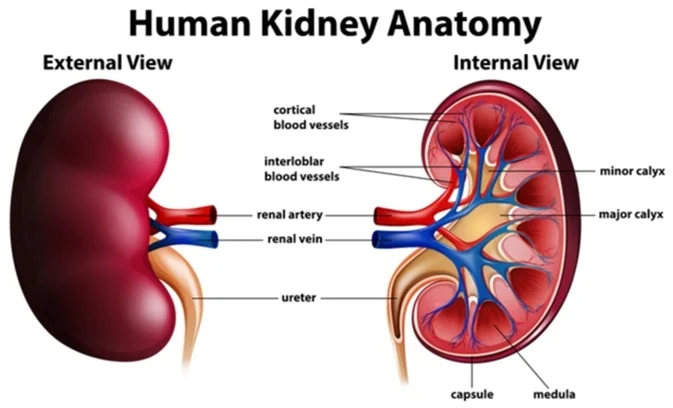
The Kidneys
There are two kidneys which lie behind the peritoneum on either side of the vertebral column. In adults, they measure approximately 12 to 14 cm.
The urine is formed in the kidney by the nephrons.
Each kidney has approximately one million nephrons.
Role of the Kidneys
• Influence blood pressure control
• Release renin to activate the renin-angiotensin system
• Can lead to water retention or excretion
• Waste excretion(Urea, Creatinine, Uric Acid)
• Blood filtration
• Blood glucose regulation(glucose absorption)
• Acid Base Balance/pH regulation
• Electrolyte balance (Sodium, Potassium, Chloride)
•Erythropoiesis regulation(also produces Erythropoietin)
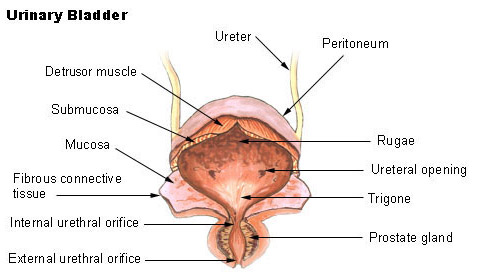
URINARY BLADDER
It is made up of four layers i.e.
- Mucosa; this is the innermost layer with rugae that allows its distention.
- Sub mucosa which provides rich vascular supply
- Smooth muscle layer/ detrusor muscle; which contracts during urination for urine expulsion.
- Serosa: a continuation of peritoneum
The bladder has a triangular area called trigone with three openings at its angles i.e two for ureters laterally and one for the urethra at the apex
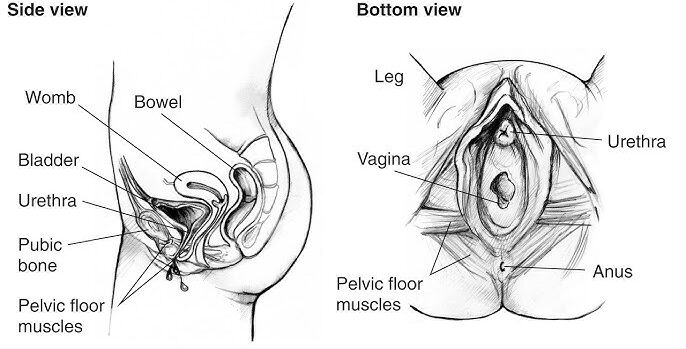
URETHRA
This conveys urine from the urinary bladder to outside of the body.
The internal sphincter of smooth muscle and external urethral sphincter of skeletal muscles constricts the lumen of the urethra causing bladder to fill.
Female urethra is 4cm long and male urethra is 20 cm
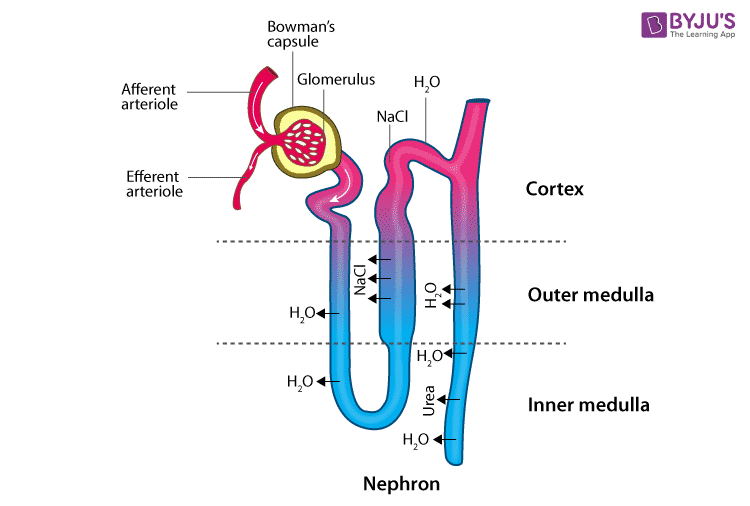
NEPHRON
This is a functional (urine) forming units of the kidneys
Components of the Nephron
- Bowman’s Capsule a cup-like structure made of squamous epithelium and inner layer has modified cell (podocytes) closely associated with glomerular capillaries
- Glomerulus made of highly permeable capillary network
- Proximal convoluted tubule, made of cuboidal epithelium with microvilli. It is a primary site of tubular reabsorption and secretion mechanisms.
- Loop of Henle, both ascending and descending loops are involved in urine concentration
- Distal Convoluted tubule; this is shorter than the proximal and contains macula densa specialized sensory cells which monitor NaCl concentrations. it’s a site of tubular reabsorption and secretion
- Collecting Ducts; these empty urine into the renal pyramids
Physiology of the urinary system
The volume of the urine excreted per day is about 1500m/s or roughly 1 ml /min. The processes responsible for urine formation are ultra filtration at the glomeruli and reabsorption in the tubules of the nephrons.
The kidneys are largely responsible for maintaining this constancy and the excretion of waste products of metabolism.
For example, urea which is a waste product of protein metabolism is excreted in a large quantity. Various renal functions are illustrated below
FUNCTIONS OF THE RENAL SYSTEM
- Regulation of the water content of the body: About 2/3 of water filtered by the glomeruli is reabsorbed in the proximal tubules iso-osmotically. The remaining water is reabsorbed in distal tubules and collecting duct; under the influence of antidiuretic hormone (ADH).
- Regulation of normal acid-base balance of the blood. The kidneys help to maintain a normal internal environment by preventing body fluids from becoming too acidic or too alkaline.
- Regulation of electrolyte content of the body. A large part of sodium ions (Na+), chloride ions (Cl- ) are actively reabsorbed in the PCT, DCT and collecting ducts. The kidney regulates the fluid balance by excreting more urine when a large amount of urine is taken and retains fluid when much has been lost.
- Hormonal and metabolic functions. The kidney produces many hormones which take part in various metabolic functions >Renin is produced in the “Juxta glomerular apparatus” and stimulates aldosterone secretion.
- > Erythropoietin – stimulates red blood cells production
- > Prostaglandins produced in the kidneys help in vasodilation of blood vessels.
Processes Involved in urine formation
- Filtration
- Selective Reabsorption
- Tubular Secretion
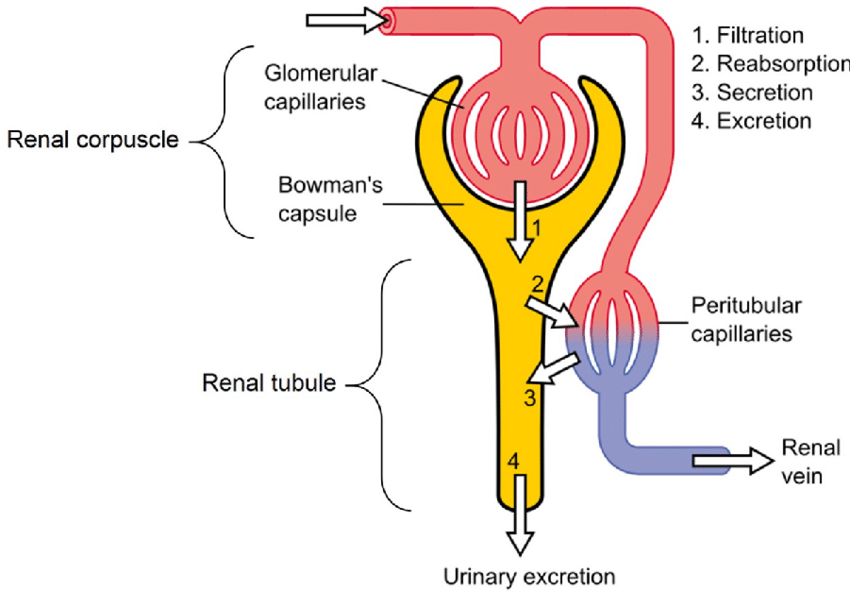
FILTRATION
This takes place through the semipermeable walls of the glomerulus and glomerular capsule/Bowman’s Capsule. Water and other small molecules pass through, although some are reabsorbed later. Blood cells, plasma proteins and other large molecules are too large to filter through and therefore remain in the capillaries.
Filtration takes place because there is a difference between the blood pressure in the glomerulus and the pressure of the filtrate in the glomerular capsule.
Because the afferent arteriole is narrower than the afferent arteriole, a capillary hydrostatic pressure builds up in the glomerulus. This pressure is opposed by the osmotic pressure of the blood, provided mainly by plasma proteins, and by filtrate hydrostatic pressure in the glomerular capsule,
The volume of filtrate formed by both kidneys each minute is called the glomerular filtration rate (GFR). In a healthy adult the GFR is about 125 ml/min, i.e. 180 liters of filtrate are formed each day by the two kidneys. Nearly all of the filtrate is later reabsorbed from the kidney tubules with less than 1%, i.e. 1 to 1.5 liters, excreted as urine. The differences in volume and concentration are due to selective reabsorption of some filtrate constituents and tubular secretion of others
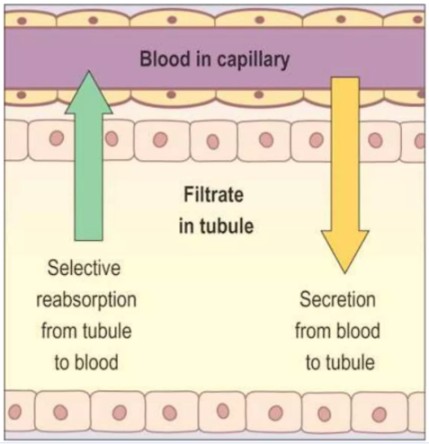
SELECTIVE REABSORPTION
Most reabsorption from the filtrate back into the blood takes place in the proximal convoluted tubule, whose walls are lined with microvilli to increase surface area for absorption.
Materials essential to the body are reabsorbed here, including some water, electrolytes and organic nutrients such as glucose. Some reabsorption is passive, but some substances are transported actively. Only 60–70% of filtrate reaches the loop of the nephron.
Much of this, especially water, sodium and chloride, is reabsorbed in the loop, so only 15–20% of the original filtrate reaches the distal convoluted tubule, and the composition of the filtrate is now very different from its starting values. More electrolytes are reabsorbed here, especially sodium, so the filtrate entering the collecting ducts is actually quite dilute. The main function of the collecting ducts therefore is to reabsorb as much water as the body needs.
TUBULAR SECRETION
Filtration occurs as the blood flows through the glomerulus.
Substances not required and foreign materials, e.g. drugs including penicillin and aspirin, may not be cleared from the blood by filtration because of the short time it remains in the glomerulus.
Such substances are cleared by secretion from the peritubular capillaries into the convoluted tubules and excreted from the body in the urine.
Tubular secretion of hydrogen ions (H+) is important in maintaining normal blood pH.
Effects of a Full Bladder in Labor
A full bladder during labor can have several negative consequences:
- Compression of the bladder: The fetal head can compress the bladder, leading to bruising and edema.
- Delayed descent of the presenting part: A full bladder can impede the descent of the baby.
- Increased pain and prolonged labor: A full bladder contributes to discomfort and can lengthen labor.
- Delayed placental delivery: A full bladder can hinder placental expulsion.
- Retained products of conception and postpartum hemorrhage (PPH): A full bladder increases the risk of retained placental fragments and subsequent PPH.
- Increased risk of urinary tract infections (UTIs) during the puerperium (postpartum period): Urinary stasis increases the chance of infection.
- Vesicovaginal fistula: In severe cases, prolonged pressure can lead to the formation of a fistula between the bladder and vagina.
Importance of the Urinary Bladder in Midwifery (During Pregnancy, Labor, and Puerperium)
Frequency of Micturition:
- First trimester: Frequent urination is due to the pressure of the growing uterus on the bladder.
- Second trimester: Frequency may be caused by UTIs, resulting in dysuria (painful urination).
- Late pregnancy: Frequency is often due to the presenting part descending into the pelvis.
- Labor: Frequent urination can be caused by malpositions (e.g., occipital posterior position) and increased fluid intake, as well as pressure from the presenting part.
- Puerperium: Frequency occurs due to autolysis (self-digestion of tissues) and ischemia (reduced blood flow) as the body eliminates waste products.
Retention of Urine:
- Pregnancy: Retention can be caused by retroversion of the uterus.
- Labor: The bladder lumen is pulled upward due to elongation of the urethra.
- Puerperium: Retention is often due to pain after episiotomy and nerve injury during delivery.
Incontinence of Urine:
- Pregnancy: Incontinence can result from relaxation of the pelvic floor muscles, causing urine leakage with coughing, sneezing, or laughing.
- Labor: Incontinence is often due to the descending presenting part.
- Puerperium: Incontinence may be due to pelvic floor injuries, such as vesicovaginal fistula.
- Stress incontinence: This is caused by increased intra-abdominal pressure.
Prevention of Urinary Complications
During Pregnancy:
- Avoid using traditional medicines that weaken pelvic floor muscles.
During Labor:
- Keep the bladder empty.
- Avoid overstretching of the pelvic floor muscles.
- Perform episiotomy when necessary.
- Avoid prolonged labor; consider Cesarean section to prevent injuries.
During Puerperium:
- Perform postnatal exercises like Kegel exercises.
- Treat any infections, such as UTIs.
- Delay sexual intercourse until after the postpartum period.
Physiology of Micturition (Urination)
The sensation of a full bladder is transmitted to the brain via sensory sympathetic nerves. When it is appropriate to urinate:
- Voluntary nerves relax the membranous sphincter.
- Sympathetic nerves relax the internal sphincter.
- Parasympathetic nerves cause the detrusor muscles to contract, pulling on the pubovesical muscle and opening the internal urethral meatus.
- Intra-abdominal pressure increases, and urine is passed with a bearing-down movement. The bladder pressure increases rapidly once its volume exceeds approximately 400-500 ml.
Clinical Procedure: Catheterization
Scenario: A mother in labor has contractions with delayed descent of the presenting part, possibly due to a full bladder.
Task: Carry out catheterization.
Objectives:
- State indications for catheterization.
- Prepare the requirements for passing a urethral catheter.
- Perform the procedure of passing a urethral catheter.
Indications for Catheterization:
- To obtain a urine specimen for investigation.
- To facilitate descent of the presenting part.
- To prevent retention of products of conception and PPH.
- To ensure an empty bladder before surgery to avoid injury.
Catheterization Procedure
Top Shelf:
A sterile park containing:
- Towel
- Drape 1
- Receiver 2
- Gauze swabs
- Cotton wool swabs
- Gallipot 2
Bottom Shelf:
- Two Foley catheters of required sizes.
- Spigot and drainage bag.
- Sterile water.
- Antiseptic lotion.
- Sterile surgical gloves.
- 3 receivers.
- Sterile water and needle.
- Specimen bottles.
- Mackintosh apron.
- Syringes of sterile water.
- Plastic sterile chart.
- Strapping.
- Measuring jar.
Bed Side:
- Screens
- Hand washing equipment
- Basin
- Soap.
- Hand towel.
EXAMINER’S CHECKLIST.
Station:
Scenario: FEMALE CATHETERISATION.
Examiner’s name ………………………………………..…date………………………………..
School code……………………………………………………candidate’s No……………………………
NO. | AREAS TO BE ASSESSED | SCORE | DONE | PARTIALLY DONE | NOT DONE | TOTAL |
1 | Creates rapport with the patient. | ½ |
|
|
|
|
2 | Explains the procedure | ½ |
|
|
|
|
3 | Screens the bed and extends the trolley to the bed side. | ½ |
|
|
|
|
4 | Puts the small mackintosh and towel to protect the linens | ½ |
|
|
|
|
5 | Washes hands methodically and puts on surgical gloves. | 1 |
|
|
|
|
6 | Inspects and cleans the vulva in a methodical way. | 1 |
|
|
|
|
7 | Drapes the mother | ½ |
|
|
|
|
8 | Selects the appropriate catheter and lubricates the tip with k.y jelly. | ½ |
|
|
|
|
9 | Place the receiver in between the thighs and puts the catheter, inserts slowly until urine is seen emptying into the receiver | 1 |
|
|
|
|
10 | Injects into the catheter to balloon it and aid it remain in situ. | 1 |
|
|
|
|
11 | Connects the catheter to the urinary bag and Fastens it on the thigh | 1 |
|
|
|
|
12 | Removes the receiver, drape, and small mackintosh. | ½ |
|
|
|
|
13 | Measures the urine collected and records in the fluid balance chart. | ½ |
|
|
|
|
14 | Clears away, leaves the mother comfortable and thanks her. | ½ |
|
|
|
|
15 | Washes hands and documents the findings. | ½ |
|
|
|
|
| TOTAL | 10 |
|
|
|
|
Examiner’s comments………………………………………………………………………………………………………
Revision Questions
- Explain the role of the sympathetic nerves.
- Outline the different parts of the kidney.
- Explain the endocrine activity of the kidneys.
- Explain the role of the renin-angiotensin system.
- State five functions of the kidneys.
- Explain the functional part of the renal system.
- Describe the gross structure of the bladder.
- Describe the microscopic structure of the bladder.
- State two functions of the urinary bladder.
- Outline the relations of the bladder.
- Explain the three processes of production of urine.
- Describe the urethra.
- Explain the importance of the urinary bladder during pregnancy.
- Explain the importance of the urinary bladder in labor.
- Outline the importance of the urinary bladder during the puerperium.
- List seven effects of a full bladder in labor.
- Explain the prevention of complications of the renal system during pregnancy.
- List five ways how complications of the renal system can be prevented during pregnancy.

Nice topic