Table of Contents
ToggleThe Perineal Body
The perineal body is a small, pyramid-shaped mass made of muscles and fibrous tissue, located between the lower end of the rectum and the vagina.
Size: It measures about 4 cm but can stretch significantly during the second stage of labor.
Shape: It has a triangular shape, with the base being the skin and the apex pointing upwards.
Location: It lies between the vagina and the rectum.
Structure: The perineal body is composed of three layers of tissue:
- Outer covering: The skin.
- Superficial pelvic floor muscles: These include muscles like the Bulbocavernosus and Transverse Perineal muscles.
- Deep pelvic floor muscles: These provide additional support.
Blood Supply
- Arterial Supply: Pudendal arteries, which are branches of the internal iliac arteries.
- Venous Drainage: Blood is drained through veins corresponding to the pudendal arteries.
Lymphatic Drainage: Lymph drains into the inguinal lymph nodes.
Innervation/Nerve Supply: The perineal body is innervated by the perineal branch of the pudendal nerves.
Functions
- Childbirth: The perineal body stretches to allow the baby to pass through during childbirth.
- Defecation: It plays a role in the process of defecation.
- Surgical Importance: It is the area where an episiotomy may be performed during childbirth. Trauma to this area can lead to complications such as urinary or fecal incontinence and prolapse of pelvic organs.
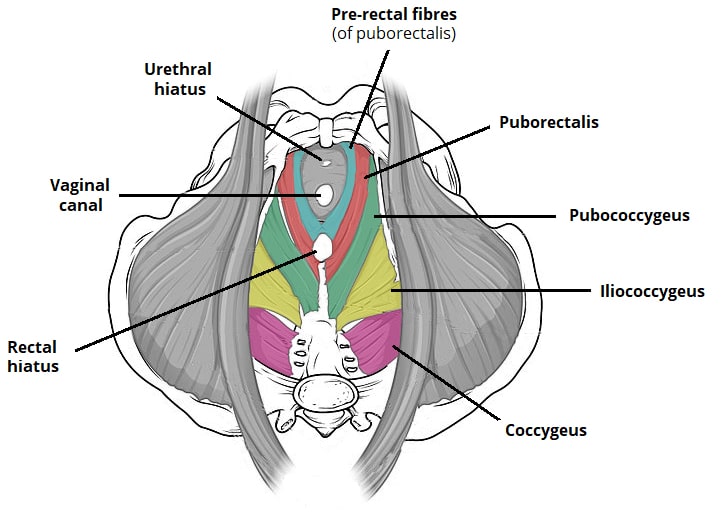
The Pelvic Floor Muscles
The pelvic floor muscles form a muscular diaphragm that fills the pelvic cavity, supporting the organs within.
Shape: The pelvic floor is gutter-shaped, which influences the rotation of the baby’s presenting part during childbirth.
Functions
- Support: The pelvic floor muscles support pelvic and abdominal organs, preventing them from prolapsing.
- Pressure Maintenance: They help maintain pressure during activities like coughing and sneezing.
- Bowel and Urinary Function: These muscles are involved in bowel movements and urination.
- Labour: During the second stage of labor, the pelvic floor provides necessary resistance to help push the baby through the birth canal.
Gross Structure: The pelvic floor is pierced by three openings:
Urethral Orifice
Vagina
Rectum
Layers of the Pelvic Floor
From inside to outside, the pelvic floor is composed of:
- Peritoneum
- Fascia Layer
- Deep Muscle Layer
- Subcutaneous Layer
- Skin
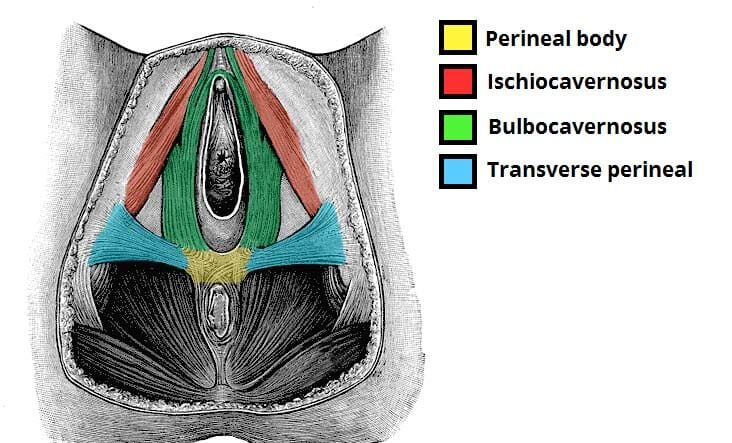
Superficial Pelvic Floor Muscles
These muscles include:
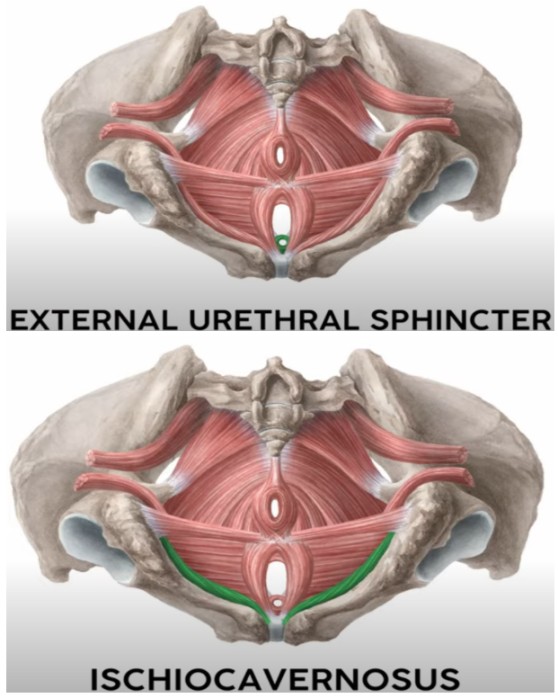
- Urethral Sphincter: Controls the passage of urine.
- Ischiocavernosus: Arises from the ischial tuberosities and runs along the pubic arch to the clitoris. (Ischium to the genitals)
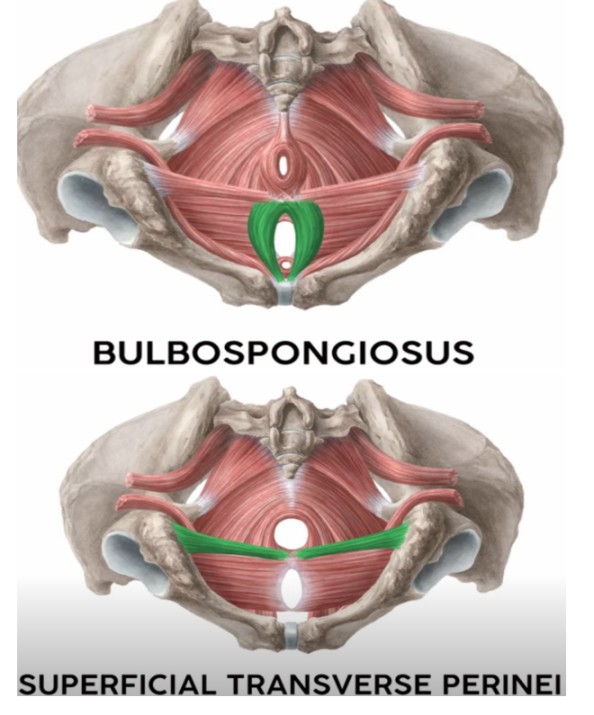
- Bulbocavernosus (Bulbospongiosus): Encircles and strengthens the vaginal orifice, extending from the perineal body to the pubic bone.
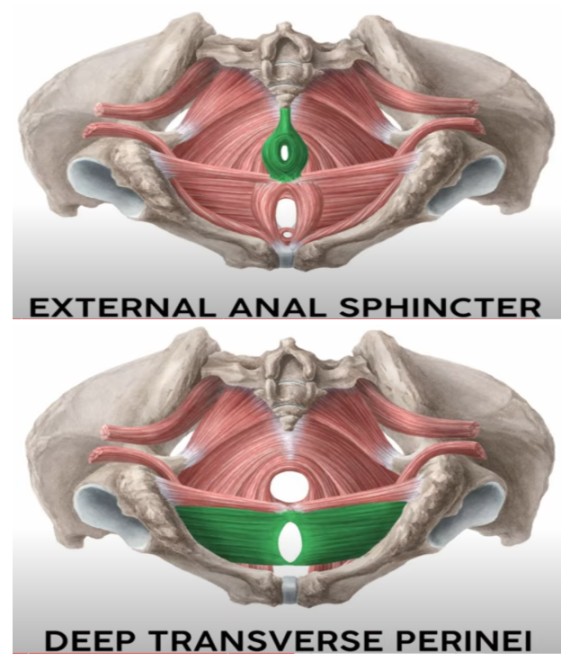
- Transverse Perineal Muscle: Runs from the ischial tuberosities to the centre of the perineum. (surface, side to side)
- External Anal Sphincter: Surrounds the anus and attaches to the coccyx.
Deep Pelvic Floor Muscles
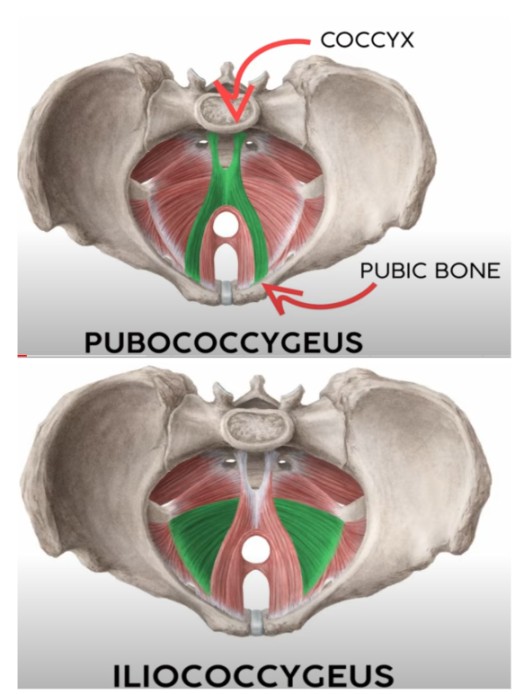
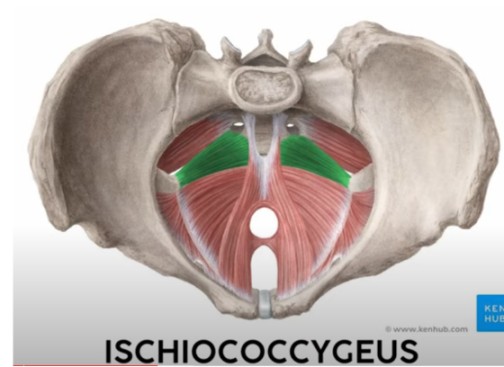
The deep muscle layer consists of three paired muscles collectively known as the levator ani. They are the most significant muscles of the pelvic floor. They are the floor of the pelvis. Keeps organs from falling out of the pelvis.
- Attachment Points:
- Front: Lateral part of the symphysis pubis.
- Back: Ischial spines and pubis.
- Sides: Obturator foramen.
Muscles:
- Pubococcygeus: Arises from the pubic bone, surrounds the urethra, vagina, and anus, and inserts into the coccyx.
- Iliococcygeus: Arises from the ilium at the white line of fascia and inserts into the coccyx.
Ischiococcygeus: Arises from the ischial spines and passes backward to insert into the coccyx.
Clinical Notes
- During Labour: The anterior pelvic wall moves upwards and forwards during the second stage of labour, pulling the bladder and urethra upwards, making them abdominal organs. This can cause urinary retention, so emptying the bladder before the second stage is crucial.
- Post-Delivery: After childbirth, the pelvic floor, bladder, and urethra return to their pre-delivery positions, a process known as the “swing door action” of the pelvic floor muscles.
Functions of the Pelvic Floor Muscles:
- Support: The pelvic floor muscles provide essential support for the pelvic organs (bladder, uterus, rectum) and prevent prolapse (the downward displacement of these organs).
- Continence: The coordinated action of the urethral and anal sphincters and the levator ani muscles is vital for maintaining urinary and fecal continence. Weakness in these muscles can lead to incontinence.
- Sexual Function: The pelvic floor muscles play a role in sexual function in both men and women. Their strength and tone influence sensations and orgasmic response.
- Pressure Regulation: These muscles help regulate intra-abdominal pressure, preventing the prolapse of pelvic organs during activities like coughing, sneezing, and lifting heavy objects. Weakness in these muscles can exacerbate prolapse.
- Childbirth: During the second stage of labor, the pelvic floor muscles provide controlled resistance to facilitate the descent of the baby through the birth canal. The interplay between the muscles’ strength and elasticity influences the risk of perineal tearing.
Superficial Pelvic Floor Muscles:
- Urethral Sphincter (Internal and External): The internal urethral sphincter is involuntary, while the external urethral sphincter is under voluntary control and contributes to urinary continence.
- Ischiocavernosus: These muscles contribute to erection and clitoral engorgement in females and penile erection in males.
- Bulbocavernosus (Bulbospongiosus): This muscle contributes to vaginal constriction, clitoral erection, and ejaculation in females and penile erection and ejaculation in males.
- Transverse Perineal Muscle: These muscles contribute to support of the perineal body.
- External Anal Sphincter: This muscle, along with the internal anal sphincter (involuntary), controls defecation.
Injury to Pelvic Floor Muscles During Labor
Overstretching:
- During late pregnancy, progesterone softens ligaments in preparation for labour.
- First Stage: Bearing down prematurely can cause excessive strain on the peri-cervical tissue and transverse cervical ligaments, leading to a retroverted uterus.
- Second Stage: Prolonged labor can overstretch the fascia supporting the bladder, leading to prolapses like cystocele, rectocele, urethrocele, and uterocele.
Tears and Lacerations:
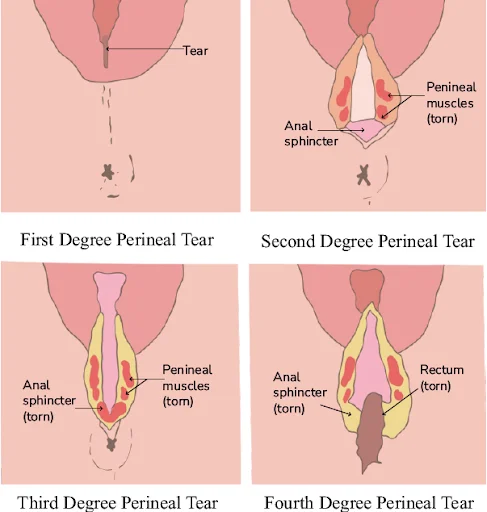
Tears can affect the levator ani muscles and surrounding tissues. These tears are classified by severity into four degrees:
- 1st Degree: Involves the fourchette, vaginal mucosa, and perineal skin, but not muscles.
- 2nd Degree: Involves the fourchette, skin, and muscles of the perineum.
- 3rd Degree: Extends to the anal sphincter.
- 4th Degree: Extends through the rectal lining, potentially leading to pelvic floor dysfunction and fecal incontinence.
Prevention of Pelvic Floor Injuries
During Pregnancy:
- Antenatal Care: Encourage regular antenatal visits and hospital delivery for high-risk mothers.
- Weight Management: Maintaining a healthy weight gain during pregnancy minimizes strain on the pelvic floor.
- Ultrasound Scans: Advise mothers to undergo ultrasounds to detect malpresentations and plan the mode of delivery.
- Nutrition: Promote a nutritious diet to build healthy skin and correct anemia.
- Hygiene: Educate mothers on maintaining hygiene to prevent infections.
- Exercises: Recommend exercises like walking and hill climbing to strengthen the pelvic floor muscles.
- Constipation Management: Constipation increases intra-abdominal pressure, potentially stressing the pelvic floor. Adequate fiber intake, hydration, and stool softeners can help prevent constipation.
- Hydration: Adequate hydration helps prevent constipation and maintains tissue elasticity.
- Labor Preparation: Teach mothers what to do during labor, including avoiding native medicines that may weaken the perineal muscles.
During Labor:
- Pain Control: Effective pain management techniques, such as epidurals, reduce the urge to push prematurely and allow for more controlled descent of the baby, decreasing the risk of perineal trauma.
- Positional Changes During Labor: Encouraging different labor positions (e.g., upright, lateral) can facilitate optimal fetal descent and reduce the strain on the pelvic floor.
- Controlled Pushing: Guided pushing techniques, under the guidance of a skilled birth attendant, help prevent excessive straining and reduce the risk of injury.
- Skilled Birth Attendant: Ensure that delivery is managed by a skilled birth attendant who can recognize and prevent impending tears.
- Instrumental Delivery Techniques: Proper use of forceps or vacuum extraction minimizes the risk of injury if necessary, and should only be performed by experienced practitioners.
- Perineal Massage: Perineal massage during the later stages of pregnancy may help increase perineal elasticity and reduce the risk of tearing during labor. (Evidence is mixed, and this needs to be discussed with the patient).
- Episiotomy: Perform an episiotomy if necessary to prevent severe tears.
Postpartum Prevention:
- Postnatal Pelvic Floor Assessment: A post-delivery pelvic floor assessment is useful to identify any damage or weakness.
- Postnatal Pelvic Floor Muscle Training (PFMT): Early initiation of PFMT post-delivery helps repair and strengthen the pelvic floor, improving recovery and reducing the risk of long-term problems.
- Physiotherapy: Physiotherapy may be beneficial for women with significant pelvic floor damage or persistent issues, providing specialized exercises and guidance.
- Lifestyle Modifications: Maintaining a healthy lifestyle, including appropriate diet, exercise, and weight management, is essential for long-term pelvic floor health.
- Continence Management: If necessary, strategies for managing urinary or fecal incontinence (behavioral modification, medication) can be initiated.
Revision Questions
- Name four superficial pelvic floor muscles.
- List three parts of the perineal body.
- Describe the swing door action of the pelvic floor muscles.
- Identi fy three types of pelvic floor injuries during labor.
- Explain ten ways to prevent perineal tears.
- How would you determine if a tear is a third-degree tear?