Table of Contents
ToggleHormonal Methods of Family Planning
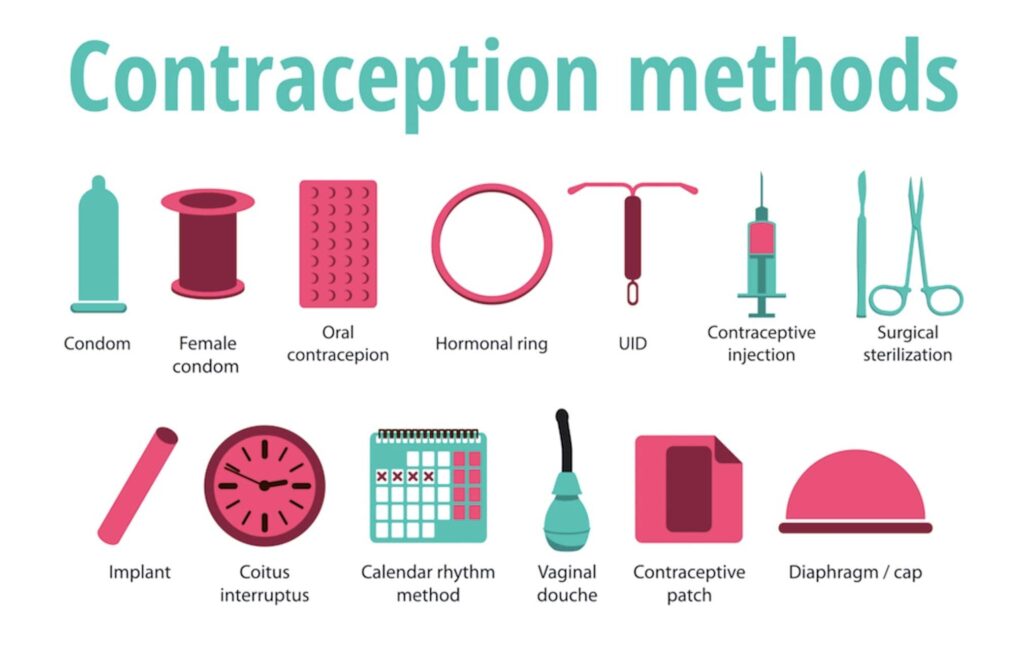
Hormonal family planning refers to the use of hormonal methods to prevent pregnancy. These methods involve the use of hormones, typically synthetic versions of those naturally produced by the body, to regulate a woman’s menstrual cycle and prevent ovulation (the release of an egg from the ovaries). By preventing ovulation, hormonal methods make it difficult for sperm to fertilize an egg and thus prevent pregnancy.
These include;
- Oral contraceptive pills
- Implants
- Injectable contraceptive
- Emergency contraceptive pills
Oral Contraceptive Pills
i) Progesterone Only Pills (POP)
Examples
- Ovrette
- microval
- They contain progesterone hormone
- They are recommended for breastfeeding mothers because they do not affect/suppress milk
Modes of action
- It acts mainly by making cervical mucus thick and viscous, thereby preventing sperm penetration
- Endometrium becomes atrophic so blastocyst implantation is also
- In about 2% ovulation is inhibited and 50% of women ovulate normally
Advantages
- Highly effective
- Limited related side effects
- Protects against unwanted pregnancy
- Do not affect breastfeeding
- May decrease menstrual cramps
- May improve anemia
- Protects against ectopic pregnancy
Contraindications
- Pregnancy
- Unexplained vaginal bleeding
- Recent history of breast cancer
- Arterial diseases
- Thromboembolic diseases
- Active hepatic diseases
- Hypertension
Side effects
- Amenorrhea
- Spotting
- Prolonged or heavy bleeding
- Lower abdominal pain
- Weight gain or lose
- Jaundice
- Nausea and vomiting
- Headache with blurred vision
- Excessive hair growth
- Breast fullness or tenderness
- High blood pressure
i) Combined Oral Contraceptive Pills (COC)
- This contains both oestrogen and It achieves effects of both hormones
- Oestrogen suppresses ovulation and progesterone creates unfavorable conditions for egg transport and thickening of the cervical mucus to impair sperm entrance into the canal.
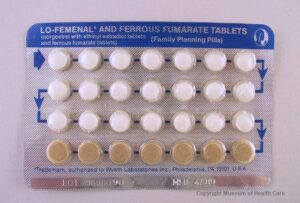
Examples
- Lo-femenal
- Pillplan (duofen)
- Microgynon

Advantages
- Highly effective (99%)
- Protects against unwanted pregnancy
- It is convenient, simple to take and does not interfere with sexual intercourse
- Helps to correct menstrual irregularities
- Reduces risks of ovarian and endometrial cancers by 50%
- Decreased menstrual cramps
- Pelvic examination is not required before use
- Limited related side effects
- Quicker return of infertility
Disadvantages
- Refer to pop Side effects
- Chest pain
- Amenorrhea
- Spotting
- High blood pressure
- Nausea, dizziness & nervousness
- Acne
- Breast fullness & tenderness
- Depression
- Jaundice
- Headache
Implants
Types
- Implanon ( 1 rod capsule for effective 3 years)
- Jadelle (2 rod capsules for 5 years)
- Norplant ( 6 rod capsules labeled for 5-7 years)
Modes of action
- Thickens the cervical mucus 24 hours making it difficult for the sperm to enter the uterus.
- It inhibits ovulation from taking place.
Advantages
- Very effective within 24 hours after insertion
- Easily reversible
- No delay to return to fertility after removal
- Make sickle cell crisis less frequent & less painful
- Highly effective for long term
- Others same as with Depo Provera
Common side effects and disadvantages
- Changes in menstruations
- Spotting
- Heavy bleeding (rare)
- Amenorrhea
- Does not protect against STIs including HIV/AIDs
- Discomfort in the hand after insertion
- Overweight or weight loss
- Minor surgical procedure required for insertion and removal.
Indications
- Breast feeding post-partum mothers
- Adolescents
- Post abortion
- Women with SCD
- Women waiting surgical contraception
- Women on treatment e. ARVs
Contraindications
- Serious problems with heart or blood vessels
- Breast cancer
- Liver diseases- jaundice
- Pregnancy
Signs and problems that need medical attention
- Soreness at the site of insertion
- Capsules come out
- Severe headache
- Heavy bleeding twice as much and twice as long she usually bleeds
- Pregnancy
- Missed period after several regular period or cycles.
Injectable contraceptives
Examples
- Depo provera 150mg
- Injecta plan
- Sayana press 104mg, 65ml subcutaneously
- Noristrat 200mg intramuscularly
- Norigynon 5mg intramuscularly
They both contain only one type of hormones, progestin
Depo Provera

Mode of action
- Inhibits ovulation
- Thickens the cervical mucus making it difficult for the sperm to enter the uterus
- It also makes the lining of the womb thinner. This makes it unlikely that a fertilized egg will be able to implant in the womb.
Indications/who can use it?
- Breastfeeding mothers 6 weeks after delivery or immediately if not breastfeeding
- Women requiring long term contraception
- Known/suspected HIV positive women who need an effective FP method
- Women with sickle cell disease
- Women who cannot use COC due to estrogen content
- Women awaiting surgical method of contraception
Contraindications
- As for POP
- Women without proven fertility unless they have HIV/AIDs
- Pregnancy (known or suspected)
- Liver disease (jaundice)
- Unexplained vaginal bleeding that has not be investigated
- Hypertension 140/90mmg and above
- Serious problem with the heart or blood loss
- Breast or genital malignancy (known or suspected)
- Women with bone thinning/osteoporosis (known or suspected)
Advantages and non-contraceptive benefits
- Very effective
- Does not suppress lactation
- Clients only has to remember the return dates for subsequent injection
- Private-no one can know that the woman is on it
- No estrogen side effects
- Make sickle cell crisis less frequent
- If you want to stop using it you don’t have to go back to your doctor or nurse to have it removed; you just have to wait for it to wear off.
- It does not interfere with sex
Disadvantages and common side effects
- Changes in menstrual bleeding
- Spotting (common in the first 3 months)
- Amenorrhea (often after 1st injection and after 9-12months of use)
- Prolonged heavy vaginal bleeding during 1st 1-2 months after injection
- Weight gain or loss
- The injection cannot be removed once given. Any side-effects will last for more than 2-3 months, until the progesterone goes from your body.
- Delayed return of fertility
- Loss of lido
- Does not protect against STI/HIV/AIDs
- Alopecia
- Milk headache
Signs and problems that need medical attention
- Repeated severe headaches
- Excessive weight gain
- Depression
- Prolonged abdominal pain and pain at injection site
- Heavy bleeding per vagina twice as much and twice as long as she usually bleeds
Management
- Medroxyprogesterone acetate depot (Depo provera) Injection 150mg deep IM into deltoid or buttock muscle
- Do not rub the area as this increases absorption and shortens depot effect
If given after day 1-7 of menstrual cycle
- Advise client
- To abstain from sex or use a back-up FP method, e.g. condoms, for the first 7 days after injection
- To return for the next dose on a specific date 12 weeks after the injection (if the client returns more 2-4 weeks later than the date advised, rule out pregnancy before giving the next dose)
- On likely side effects
- To return promptly if there are any warning signs
Sayana Press

- Sayana press ® is a single-dose container with 104mg Medroxyprogesterone acetate (MPA) in 0.65ml suspension (104mg) formulated for subcutaneous
- It is administered subcutaneously into the anterior thigh or abdomen or arm
- The efficacy of Sayana press depends on adherence to the recommended dosage schedule of administration.
Mechanism of actions
- Its‘ main mechanism of action is to suppress ovulation
- It makes the endometrium unsuitable for implantation if fertilization occurs
- It also increases the viscosity of cervical mucus making the mucus less easily penetrable to sperm.
Indications
Nearly all women can use it safely & effectively including women:-
- Women whose partners have undergone vasectomy until vasectomy is effective
- Have or have not had children
- Any age including adolescents & women over 40 years old
- Have just had an abortion/miscarriage
- Breastfeeding women 6 weeks postpartum
- HIV infected whether or not on ART
Advantages & non- contraceptive benefits
- New formulation for S/C injection
- 30% low side effects compared to Depo-Provera
- Do not interfere with sex
- Private & no one else can tell that a woman is using it
- May help women gain weight
- Do not require daily action
- Prevents pregnancy
- Protects against endometrial cancer, uterine fibroids
- Reduces sickle cell crisis among women with sickle cell anemia
- Protects against symptomatic PID & iron deficiency aneamia
Contraindications
Sayana press is contraindicated in the following:-
- Clients with a known hypersensitivity to MPA
- Pregnancy (known or suspected)
- women with known or suspected malignancy of the breast or genital organs
- clients with undiagnosed vaginal bleeding
- patients with severe hepatic impairment
- patients with metabolic bone disease
- patients with thromboembolic disease
- patients with current or past history of cerebro-vascular disease
Disadvantages & Side effects
- Weight gain or loss
- Does not protect against STI/HIV/AIDs
- Delayed fertility return
- Hypersensitivity reactions
- Decreased/increased appetite
- Loss of libido & irritability
- Dizziness, headache & migraine
- Thromboembolic disorders
- Nausea & vomiting
- Jaundice
- Alopecia & urticaria
- Loss of bone mineral density
- Back & leg pains
- Mood changes
- Abdominal bloating & discomfort
Problems that may need medical attention
- Loss of bone mineral density
- Menstrual irregularities
- Thromboembolic disorders
- Anaphylaxis & anaphylactoid reactions
- Sudden partial or complete loss of vision
Permanent Method/Voluntary Surgical Contraceptives
Because male and female sterilization are permanent methods of contraception, thorough counseling procedures must be followed to ensure that the client fully understands his or her choice and to minimize chances of regret. Clients younger than 30 years old or with fewer than three children require particularly careful counseling and exploration of other long-term method options.
Tubal ligation/tubectomy
- This is a voluntary surgical procedure for permanent termination of fertility in women.
- It can be done by a mini-operation (laparatomy/laparoscopy)
Mode of Action
- Blocking fallopian tube by cutting, cautery, rings or clips
- Prevent sperms from reaching the ovum
Indications
In general, the majority of women who want tubal ligation can have a safe and effective procedure in a routine in a health facility equipped to provide the service, provided they have been counseled. They should also be able to give informed consent. Women who may consider tubal ligation include:
- Those who are certain that they have achieved their desired family size
- Women who want a highly effective permanent method of contraception
- Women for whom pregnancy presents unacceptable risk Family planning should be delayed in case of:
- Pregnancy
- Immediately/early postpartum if woman had severe pre-eclampsia/eclampsia, early rupture of membrane (EROM), sepsis etc.
- Complicated abortion (infection, hemorrhage)
- Current DVT
- Unexplained vaginal bleeding (before evaluation)
- Malignant trophoblastic disease
- Current PID or purulent cervicitis
- Current gall bladder disease
- Severe anemia
- Acute respiratory disease
- Acute systemic infection or gastroenteritis
- Abdominal skin infection – peritonitis
Timing of the tubal ligation
- Immediately after childbirth or within first seven days (if she made voluntary choice in advance)
- Six weeks or more after childbirth
- Immediately after abortion (if she made voluntary choice in advance)
- any time provided pregnancy is ruled out (but between seven days and six weeks postpartum)
- during caesarean section
Benefits
- Highly effective
- Effective immediately
- It is permanent
- It is a simple surgery, usually done under local anesthesia
- No exposure or worries about contraception
- No further expense or worries about conception
- No long term side effects
- Does not interfere with sexual intercourse
Disadvantage
- Does not protect against STIs/AIDs
- It is irreversible
Side effects
- Wound infection
- Post-operative fever
- Bladder and intestinal injuries(rare)
- Hematoma
- Pain at the incision (post operatively)
- Superficial bleeding
Challenges associated with tubal ligation
- Desire for more children after when the operation is done
- Excessive desire in reversal
- Disagrees to sign the informed consent form
- Pressure from the someone else
- Depression
- Marital problems
- Single women
- Women with no children
General complications of tubal ligation
- Obesity
- Psychological upset
- Chronic pelvic pain
- Congestive dysmenorrheal
- Menstrual abnormalities like menorrhagia, hypomenorrhea
- Alteration in libido.
2. Vasectomy
- This is a voluntary surgical procedure for permanently terminating fertility in men
Mode of action
Blocking the vas deferens (ejaculatory duct) so that sperms are not present in the ejaculate.
Indications
- Those who are certain that they have achieved their desired family size
- Men who want a highly effective permanent method
- Men whose wives face unacceptable risk in pregnancy
Contraindications
Vasectomy should be delayed in case of:
- Local infections (scrotal skin infections, orchitis etc)
- Current STI
- Systemic infections
Benefits
- Highly effective
- It is permanent
- It is a simple surgery done under local anesthesia
- No further expense or worries about conception
- No long term side effects
- Does not interfere with sexual intercourse
Side effects
- Wound infection
- Scrotal hematoma
- Granuloma
- Excessive swelling
- Pain at incision sites
Explain the following to the clients
- When to come back for follow up visits
- Common side effects of the method offered
- What to do if there are changes in the menstrual periods
- How soon the method is effective
- How to protect against STIs
- How to care for the wound in case of implants, vasectomy and tubal ligation
General instruction to the clients using permanent methods of family planning
- Inform him or her when to come back for follow up visits
- Explain the common side effects of the method in a simple language
- Tell the client the warning signs or possible problems that may require medical attention
- Tell the client what to do if there are changes in the menstrual periods
- Inform the client how soon the method is effective
- Let the client know that the method does not protect against HIV/AIDs and STIs and emphasize on the use of backup methods like condoms
- Guide the client on how to care for the wound post operatively
Emergency /Post Coital Contraceptives
Emergency contraception (EC) refers to methods of contraception used by women to prevent unintended pregnancy following unprotected sexual intercourse. It should not be used as a routine contraceptive method. EC not a method for termination of pregnancy
Indications
- Any woman who has had unprotected sexual intercourse
- Women who have been raped
- Any woman whose contraceptive method has failed (e.g. condom broke or slipped)
- Any woman who has forgotten to take her COC pills for more than two days or who has forgotten to take her POP at the regular time
- Missed injection for more than two weeks
- Delay in taking pills more than 3 hours
- Sexual assault or rape and the first time intercourse
Contraindications
- Pregnancy
- After 120 hours or 5 days of unprotected sex
Types
- Emergency contraceptive pills (ECP)
- Progesterone only pills regimen.
They are the preferred ECP regimen as they are more effective and have fewer side effects than COC pills
When to start?
This should be started or taken within 5 days or 120 hours but the sooner the better following unprotected sexual intercourse.
What to use and the dose
- Lofemenal or microgynon 4BD for 1 day (low dose COC)
- Eugynon (high dose COC) 2BD for 1day
- Regular POP such as Ovrette or microval can be used in recommended dose
- Levonogestrel 2stat
- Postinar 2 BD for 1day
- vikela orlevonelle-2 or Norlevo plan B may be used
Side effects
- Nausea & vomiting
a) Intrauterine contraceptive devices (IUCDs)
Introduction of copper IUCDs with a maximum period of 5days can prevent conception following accidental unprotected sexual exposure.
Mechanism of action
- Prevents implantation
- Failure rate is about 1%
- Effectiveness is over 99% in preventing pregnancy
Notes
Post coital contraception is only employed as emergency measure and is not effective if used as regular method of contraception with the exception of the copper IUCDs
Women who need emergency contraception should be counseled about regular contraceptive options and encouraged to use regular methods consistently and correctly. Referral:
- Women should be referred for other relevant services such as HIV counseling and testing, post exposure prophylaxis (PEP) and treatment for STIs
- Women should be referred to specialized services such as for sexual and gender based violence.
Basic steps of client care for ECP
- Greet client, introduce yourself, and ask what he/she
- Show a respectful attitude
- Explain that your discussion with the client will be kept
- Explain the different ECP
- Screen the client for ECP use.
- Tell client about ECPs; give clear information about use, side effects, and needs for referral or follow-up.
- Encourage her to ask questions
- Discuss options for regular contraception with client
Counseling ECP clients
When counseling a client about ECP, the provider should:
- Actively involve the client in the counseling process
- Reassure the client that all information she gives you is kept confidential
- Provide a private and supportive environment
- Do not make judgmental comments or indicate disapproval through body language (such as such as crossing your arms over your chest)
- Be responsive to the client‘s needs
- Be supportive of the clients choices
- Be respectful